- Colorectal Cancer-Patient Version - (http://www.cancer.gov/cancertopics/types/colon-and-rectal)
- Colorectal Cancer - (http://www.nlm.nih.gov/medlineplus/colorectalcancer.html)
- Bowel Cancer - (http://about-cancer.cancerresearchuk.org/about-cancer/bowel-cancer)
- What Is Colorectal Cancer? - (https://www.cancer.org/cancer/colon-rectal-cancer/about/what-is-colorectal-cancer.html)
- Colorectal Cancer-Patient Version - (https://www.cancer.gov/types/colorectal)
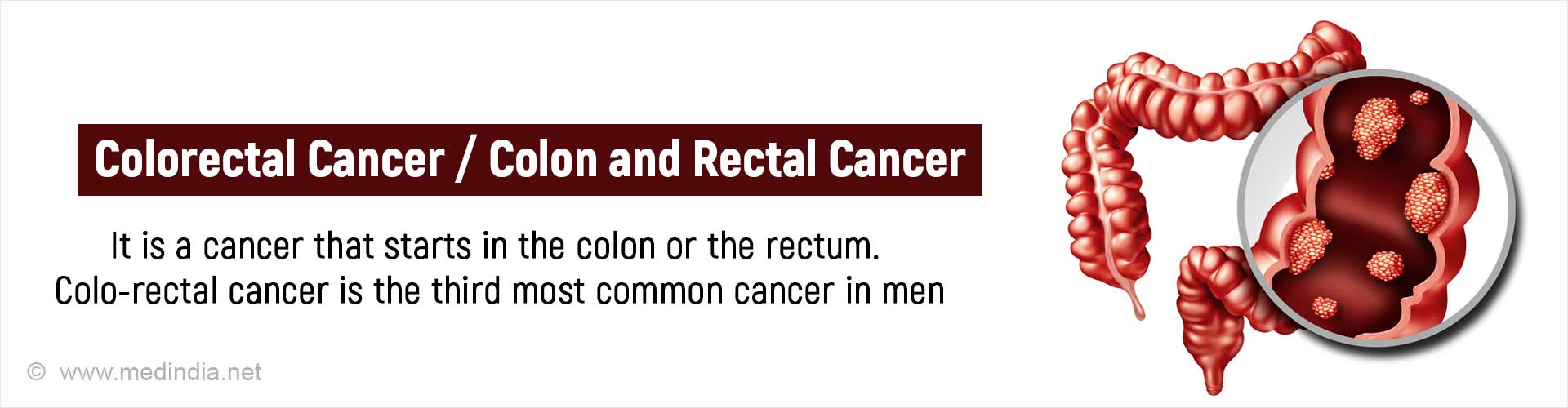
What is Colorectal Cancer?
Colorectal cancer is a cancer that starts in the colon or the rectum. Cancer occurs when cells in a part of the body begin to grow out of control.This uncontrollable growth of abnormal cells crowds out the normal cells and replaces them. The walls of the colon and rectum have several layers of tissues. Colorectal cancer begins in the innermost layer and slowly spreads to the other layers as the disease progresses.
Cancer cells can sometimes break away from a tumor and spread to other parts of the body through the blood or lymph system. Most colon cancers are adenocarcinomas, that begin as growths called ‘polyps’ on the inner lining of the colon. They may not manifest until they either bleed or grow in size to the extent that they block the lumen of the intestine.
The chance of changing into a cancer depends on the type of polyp. There are 2 common types of polyps:
- Adenomatous polyps (adenomas)
- Hyperplastic polyps and inflammatory polyps
There seems to be an increasing incidence of these cancers in the older age group and in some patients who have a strong family history of the disease.
The colon and rectum are parts of the body's digestive system. The digestive system consists of a group of organs where the food is processed to create energy and the waste material is stored until it passes out of the body as stool. Together, the colon and rectum form a long, muscular tube called the large intestine. The colon is the first 6 feet of the large intestine, and the rectum is the last 8 to 10 inches.
Anatomy and Physiology of the Colon and Rectum
Anatomy
The colon is about six feet long and has four parts namely the ascending colon, transverse colon, the descending colon, and the sigmoid colon. Beyond the sigmoid colon are the rectum and the anus. The portion of the colon from the cecum to the mid-transverse colon is also known as the right colon. The remainder is known as the left colon.
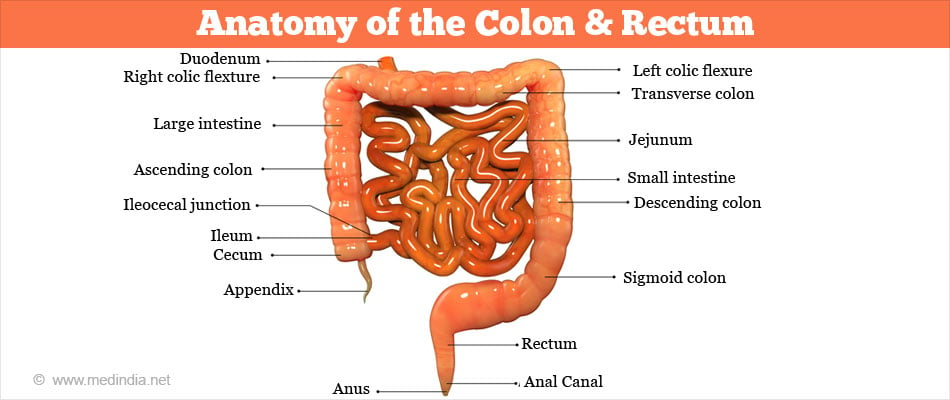
The ascending colon, on the right side of the abdomen, is about 12.5 cm long. It is the part of the colon from the cecum to the hepatic flexure (hepatic means liver). The transverse colon extends from the hepatic flexure to the splenic flexure (near the spleen). The descending colon extends from the splenic flexure to the beginning of the sigmoid colon. The sigmoid colon starts after the descending colon and ends before the rectum. The name sigmoid means S-shaped.
The rectum is about eight inches and connects the sigmoid colon with the anal canal. The anal canal is 2.5 - 4 centimeters long. It is situated between the rectum and anus.
Physiology
The functions of the colon are absorption of water and minerals and the formation and elimination of feces. The small intestine absorbs the nutrients from the food and pours the leftover sludge into the cecum. This sludgy waste then moves from the cecum to the colon for further processing. The colon absorbs water from the sludge while transporting it toward the rectum.
The colon stores the waste material until it is time for it to be evacuated. The colon moves the waste material through, by involuntary wavelike contractions made possible by smooth muscles within the colon wall, a process which is referred to as peristalsis.
The urge to defecate is signaled by the propulsion of feces from the sigmoid colon to the rectum. Distention of the rectum causes relaxation of the internal anal sphincter (involuntary sphincter). For defecation to proceed, the external anal sphincter must voluntarily relax. Defecation is facilitated by squatting or sitting and by increasing intra-abdominal pressure.
Facts About Colorectal Cancer
- Globally, colorectal cancer is the third most common cancer in men.
- It was the fourth most common cancer in 1975 and reached the second position by 1990, with about 49% increase in the number of cases globally over 15 years.
- In the developed countries it is the second most common cancer after lung cancer.
- It is the fifth-most common cancer in India.
- In developing countries there has been an increase in incidence among the younger people. It is also seen that patients diagnosed under the age of 50 are associated with more advanced stage at diagnosis & poorer outcomes
- Incidence rates range from 25.3 per 100,000 in Eastern Europe to 45.8 per 100,000 in Australia.
- Forty percent of the deaths from rectal cancer is misclassified as colon cancer deaths
- The overall lifetime risk of developing colorectal cancer is: 1 in 21 for men and 1 in 23 for women.
- Incidence rates in India are quite low - about 2 to 8 per 100,000.
- Early screening can prevent 39,700 new cases of colorectal cancer and 37,200 deaths by 2030.
- The disease has slightly higher occurrence in men than women, and is highest in African American men.
- Colorectal cancer burden has been steadily rising in women.
What are the Types of Cancer in the Colon & Rectum?
Adenocarcinomas make up for 95% of colorectal cancer cases. In the digestive tract adenocarcinoma starts in cells that make mucus to lubricate the inside of the colon and rectum. Some subtypes of adenocarcinoma, such as signet ring and mucinous, may have a worse prognosis (outlook).
Othe rare types of tumors can also start in the colon and rectum. These include:
Carcinoid tumors grow slowly and start from specialized hormone-making cells in the intestine. This cancer makes up for 1 % of all colorectal cancers.
Gastrointestinal stromal tumors (GISTs) start from specialized cells in the wall of the colon called the interstitial cells of Cajal. Some are non-cancerous (benign) but some turn into cancer and these cancer cells can be found anywhere in the digestive tract, but are not common in the colon.
Colorectal lymphomas are cancers of immune system cells that typically start in lymph nodes and account for 0.5 % of colorectal cancers; but, it is possible for them to start in the colon, rectum, or other organs too.
Sarcomas can start in blood vessels, muscle layers, or other connective tissues in the walls of the colon and rectum. Sarcomas of the colon or rectum are rare. They are discussed in soft tissue sarcoma.
What are the Causes and Risk Factors of Colorectal Cancer?
The exact cause of colorectal cancers is not known. However there are a number of known risk factors that increase the chances of developing the disease.
A small percentage of colorectal cancers are caused by gene mutations. Most people with colorectal cancer do not have an inherited gene mutation. Instead, the gene mutations develop spontaneously.
Genetic Predisposition and Mutations: Changes in a gene called APC, are responsible for diseases of the colon like Familial Adenomatous Polyposis (FAP) and Gardner syndrome. Over time, cancer will nearly always develop in these conditions. Changes in the APC gene lead to a loss of the “brake” molecule resulting in an increased growth of colorectal cells.
A defective DNA repair mechanism is responsible for Hereditary Nonpolyposis Colon Cancer (HNPCC). The error can affect the growth-regulating genes and this can lead to the development of cancer.
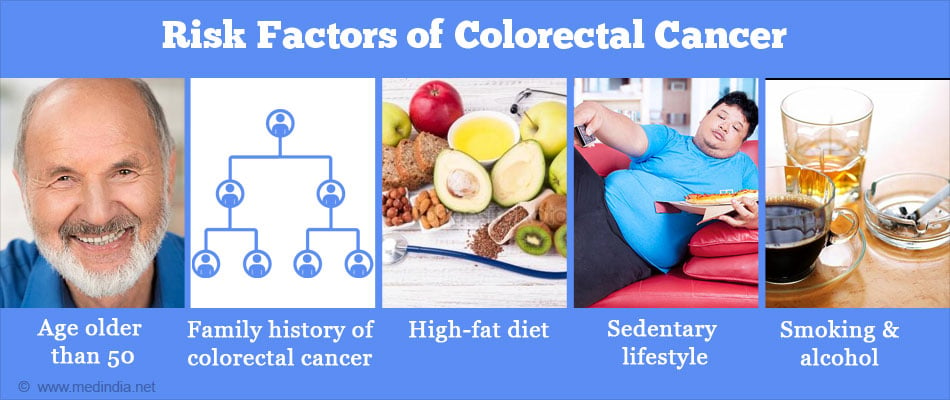
Factors that Increase the Risk of Colorectal Cancer
- Age: Over 90% of people diagnosed with colorectal cancer are older than 50.
- Family history: A family history of intestinal polyps or colorectal cancer results in an increased risk for the disease. If there is a positive history in more than one close family member the risk is even higher.
- Medical history: Medical history of Inflammatory Bowel Diseases (IBD) like ulcerative colitis, Crohn's disease and granulomatous colitis increases the risk of developing the disease.
- Race: Blacks are more likely than any other racial groups to develop colon cancer. Further, blacks have lower survival rates because diagnosis of their cancers is often delayed. Colon cancer may occur at a higher than average rate among Jews of Eastern European (Ashkenazi) descent.
Other lifestyle factors that increase the risk include the following:
- Diet: A high saturated fat, low-fiber diet and high caloric diet appears to increase the risk of developing colon cancer. Consumption of red meat too is associated with higher risk
- Sedentary lifestyle: People who are physically inactive are more likely to develop colon cancer
- Smoking: Smoking doubles the risk of developing colon cancer
- Obesity: Being extremely overweight increases the risk for colorectal cancer
- Diabetes: Diabetes increases the chances of developing colon cancer by about one-third. It may also increase the chances of dying of the cancer
- Alcohol use: Excessive intake of alcohol doubles the risk of developing colon cancer
- Radiation therapy for cancer. Radiation therapy directed at the abdomen to treat previous cancers may increase the risk of colon cancer
What are the Staging & Grading of Colorectal Cancer?
Staging is one of the most important factors in determining how to treat the cancer.
Staging means mapping the extent of the disease and grading is the type of disease, both of which are essential to plan therapy and to determine the prognosis.
Staging describes the spread of the cancer in relation to the layers of the wall of the colon or rectum, the organs next to the colon and rectum, and other organs farther away.
The American Joint Committee on Cancer (AJCC) has come out with the TNM System for describing the extent of disease progression in cancer patients. The TNM system describes the extent of the primary Tumor (T), the absence or presence of spread to nearby lymph nodes (N), and the absence or presence of distant metastasis (M).
The extent of the Tumor (T) is described as:
Tumor Growth involving the layers of the colon
Tis: The cancer is in the earliest stage. It involves only the mucosa, which is the innermost layer of the colon. This stage is also known as carcinoma in situ or intramucosal carcinoma.
T1: The cancer has grown through the muscularis mucosa and extended into the submucosa.
T2: The cancer has grown through the submucosa, and extends into the muscularis propria.
T3: The cancer has grown completely through the muscularis propria into the subserosa but not to any neighboring organs or tissues.
T4: The cancer has spread completely through the wall of the colon or rectum into nearby tissues or organs.
Spread to the Lymph Nodes (N):
N0: No lymph node involvement is found.
N1: Cancer cells found in 1 to 3 nearby lymph nodes.
N2: Cancer cells found in 4 or more nearby lymph nodes.
Metastasis (M) to distant organs like lungs and liver is expressed as:
M0: No distant spread is seen.
M1: Distant spread is present.
Based on a patient’s TNM status staging the disease from stage I (the least advanced stage) to stage IV (the most advanced stage) is as follows:
Stage 0: Tis, N0, M0: The cancer is in the earliest stage. It is found only in the innermost lining of the colon or rectum. Carcinoma in situ is another name for Stage 0 colorectal cancer.
Stage I: T1, N0, M0, or T2, N0, M0: The cancer has grown through the muscularis mucosa into the submucosa or it may also have grown into the muscularis propria, but it has not spread to nearby lymph nodes or distant sites.
Stage IIA: T3, N0, M0: The cancer has grown through the wall of the colon or rectum into the outermost layers. It has not yet spread to the nearby lymph nodes or distant sites.
Stage IIB: T4, N0, M0: The cancer has grown through the wall of the colon or rectum into other nearby tissues or organs. It has not yet spread to the nearby lymph nodes or distant sites.
Stage IIIA: T1-2, N1, M0: The cancer has grown through the mucosa into the submucosa or it may also have grown into the muscularis propria, and it has spread to 1-3 nearby lymph nodes but not distant sites.
Stage IIIB: T3-4, N1, M0: The cancer has grown through the wall of the colon or rectum or into other nearby tissues or organs and has spread to 1-3 nearby lymph nodes but not distant sites.
Stage IIIC: Any T, N2, M0: The cancer can be any T but has spread to 4 or more nearby lymph nodes but not distant sites.
Stage IV: Any T, Any N, M1: The cancer can be any T, any N, but has spread to distant sites such as the liver, lung, peritoneum (the membrane lining the abdominal cavity), or ovary.
Recurrence: This is cancer that has been treated and has returned after a period of time. The disease may return in the colon or rectum, or in another part of the body.
Grading of cancer cells is based on how closely the cells resemble normal colorectal tissue.
Low grade means the tissue closely resembles normal tissue
High grade means the tissue appears most unlike normal tissue.
High-grade cancers are associated with a poorer outcome than low-grade cancers.
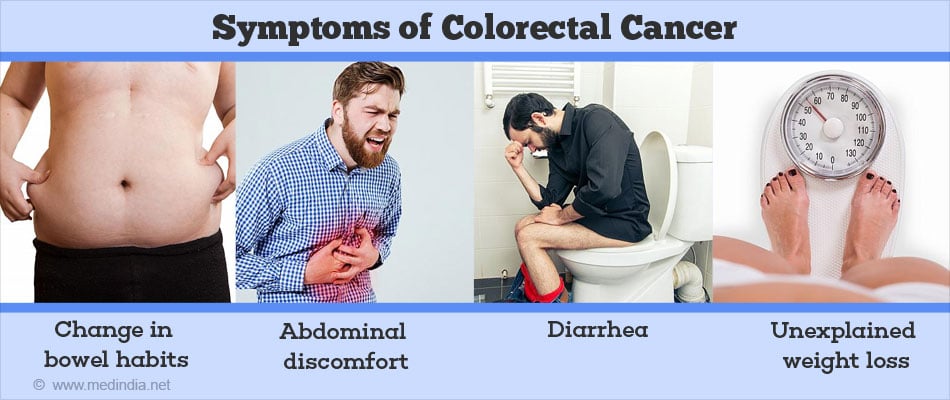
What are the Symptoms of Colorectal Cancer?
Colorectal cancer is often a silent disease, developing with no symptoms at all.
When symptoms do occur they may include the following:
- Change in bowel habits
- Blood and mucus in the stool, which may be bright red or dark in color
- Stools that are narrower than usual
- Abdominal discomfort (e.g., pain, bloating, cramping, fullness)
- A feeling of incomplete evacuation
- Nausea
- Vomiting
- Diarrhea or constipation
- Unexplained weight loss
- Rectal bleeding
- Constant tiredness
Most often, these symptoms are not due to cancer. Other health problems can cause the same symptoms. Anyone with these symptoms should consult a doctor to rule out colorectal cancer
Screening of Colorectal Cancer
Testing people without symptoms or signs of colon cancer is called screening.
Screening for colorectal cancer involves one or more tests performed to identify whether a person with no symptoms has a disease or condition that may lead to colon or rectal cancer. The goal is to identify the potential for disease or the condition early when it is easier to prevent or cure.
A simple questionnaire helps determine if a person needs to undergo screening tests or procedures.
- Are you aged 50 or older?
- Has a parent, brother, sister or child of yours had colorectal cancer?
- Has a parent, brother, sister, or child of yours had colon polyps?
- Do you have a chronic inflammatory bowel disease such as ulcerative colitis or Crohn's disease?
- If the answer is "yes" to any of the following questions, talk to your healthcare provider about getting screened for colorectal cancer
Simple screening tests include - Fecal Occult Blood Test (FOBT) and Fecal Immunochemical Test (FIT). If these are positive a Colonoscopy is advised.
If there is a family history screening at earlier age is advised.
How can Colorectal Cancer be Diagnosed?
A few symptoms and signs should help alert a doctor of the possibility of Colorectal Cancer and include blood or mucus in the stools, and unexplained change in bowel habits like diarrhea or constipation or loss of appetite, unexplained weight loss, excessive gas or abdominal pain.
Standard tests used for detecting colon cancer include:
- Fecal Occult Blood Test (FOBT)
- Fecal Immunochemical Test (FIT)
- Flexible Sigmoidoscopy
- Colonoscopy
- Double contrast Barium enema
- Digital Rectal Exam (DRE)
Digital Rectal Exam (DRE) - here a doctor examines the rectum with the gloved end of a finger. A DRE is often included as part of a routine physical exam. This simple test, which is not usually painful, can detect any growth in the anal canal or lower rectum.
Fecal Occult Blood Test (FOBT) is used to detect tiny amounts of invisible blood in the feces. Blood vessels on the surface of colorectal polyps or cancers are often fragile and easily damaged by the passage of feces. The damaged vessels usually release a small amount of blood into the feces. Only rarely is there enough bleeding to color the stool red. The FOBT detects blood through a chemical reaction.
Immunochemical Fecal Occult Blood Test (iFOBT) is a new test, which helps to detect hidden blood in the stools. It is more specific than the FOBT and reduces the number of false positive results.
Flexible Sigmoidoscopy is a test which allows the physician to look directly at the lining of the lower colon and rectum with the help of a lighted instrument called a sigmoidoscope. This test allows the physician to look for early signs of colorectal cancer like bleeding and polyps.
Colonoscopy allows the physician to visualize the entire colon and rectum using an instrument called colonoscope. Here a long flexible tube with a light is inserted into the rectum. The colonoscope is also connected to a video camera and display monitor so the doctor can see and closely examine the inside of the colon.
Biopsy: Usually if a suspected colorectal cancer is found by any diagnostic test, it is biopsied during colonoscopy. In a biopsy, the doctor removes a small piece of tissue with a special instrument passed through the scope. The biopsy specimen is sent to the pathology laboratory where a pathologist, a doctor trained to diagnose cancer and other diseases in tissue samples, examines the tissue under a microscope.
Double contrast Barium enema consists of a series of x-rays of the entire colon and rectum. ‘Double contrast’ refers to the use of both barium and air to outline the lining of the colon. The x-rays are taken after the patient is given an enema with a barium solution and air is introduced into the colon. This procedure helps to outline large polyps and cancers.
Two new tests
Researchers are working on less-invasive screening technologies that may be better tolerated and more accepted. Two emerging screening methods are:
- DNA stool testing: By examining a sample of the stool for cellular markers, this test can reveal the presence of colon cancer as well as precancerous polyps.
- Virtual Colonoscopy (CT colonography): This technology uses data from a conventional CT scan to create three-dimensional images of the interior of the colon, allowing the doctor to detect abnormal growths without inserting a colonoscope.
Tests are done to detect the stages and spread of cancer:
Imaging studies and blood tests help to stage and grade colorectal cancers.
Tests done to stage the disease include:
- Imaging tests such as chest x-ray, ultrasound and CT scan (computerized tomography) are used to detect metastasis to lymph nodes, liver, or lungs.
- Blood count: This is done to detect anemia. Many people with colorectal cancer become anemic because of prolonged bleeding from the tumor.
- Liver Function Tests (LFT): This test is done to detect any abnormalities in the liver enzymes, because colorectal cancer can spread to the liver and cause abnormalities.
- Tumor Markers: Colorectal cancer produces substances such as Carcinoembryonic antigen (CEA) and CA 19-9 that are released into the bloodstream. Blood tests for these "tumor markers" are often used for follow-up of patients who already have been treated for colorectal cancer. They may provide an early warning of a cancer that has returned. They can also help to monitor the effectiveness of therapy.
- Endorectal Ultrasound: Here an ultrasound probe is inserted into the rectum and the pictures were taken may show how deep a rectal tumor has grown or whether the cancer has spread to lymph nodes or other nearby tissues.
What are the Treatment Methods for Colorectal Cancer?
Treatment of colorectal cancers depends on the extent of spread of the disease and the general health status of a person. It is clearly related to the degree of penetration of the tumor through the bowel wall, the presence or absence of nodal involvement, and the presence or absence of distant metastases. These three characteristics form the basis for all staging systems developed for this disease. Different types of treatment are available for patients with colon cancer.
The 4 main types of treatment for colorectal cancer are the following:
- Surgical Treatment
- Chemotherapy
- Radiation therapy
- Biological therapy
Surgical Options for Colon Cancer
The surgical options for colon or rectal cancer depend on the location and the extent of the tumor.
Surgery is the most common treatment for all stages of colon cancer. The options available are:
Local excision: If the cancer is found at a very early stage, removal of the tumor is performed through a colonoscope. This is called a local excision. If the cancer is found in a polyp (a small bulging piece of tissue), the operation is called a polypectomy.
Segmental resection: Also referred to as Partial Colectomy and Hemicolectomy, it is the most commonly performed surgery and is used to treat 80-90% of colorectal cancer patients. In this procedure the segment of the colon that contains the tumor and the nearby lymph nodes are removed and healthy segments of the colon are reconnected. This procedure may be performed through a large incision in the abdomen (called open surgery) or through several small incisions (called laparoscopic surgery).
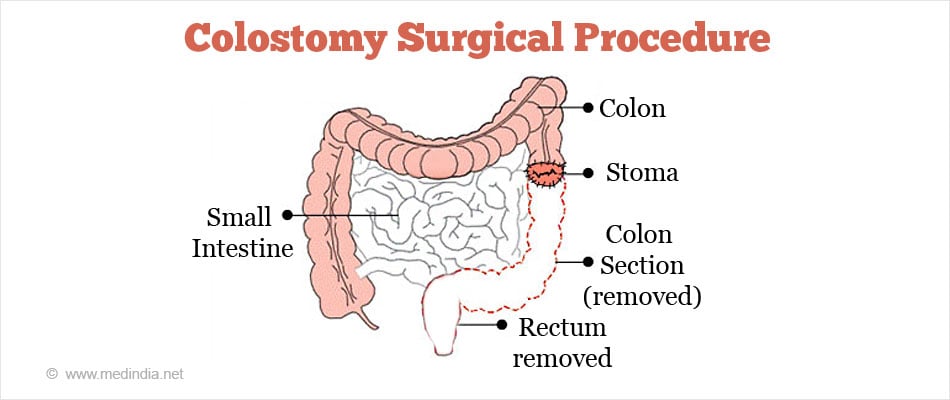
Segmental Resection and Colostomy: If after segmental resection of the colon the doctor is not able to approximate the 2 ends of the colon back together, a stoma (an opening) is made on the outside of the body for waste to pass through. This procedure is called a Colostomy. A bag is placed around the stoma to collect the waste. Sometimes the colostomy is needed only until the lower colon has healed, and then it can be reversed. This is referred to as a Temporary Colostomy. However if the doctor needs to remove the entire lower colon, then it becomes a Permanent Colostomy.
Surgical Options for Rectal Cancer
Surgery is the most common treatment for all stages of rectal cancer.
Local trans-anal resection: Here the tumor as well as some surrounding normal rectal tissue is removed. If the cancer is found in a polyp, removal of the polyp namely polypectomy is done. Polypectomy and Local trans-anal resection are done with instruments inserted through the anus, without making a surgical opening in the skin of the abdomen.
Low anterior resection: This surgery is performed through the abdomen and is used for cancers in the upper two thirds of the rectum, close to where it is connected with the colon. In this procedure the tumor can be removed without affecting the anus. After low anterior resection, the colon will be attached to the anus and the waste will be eliminated in the usual way through the anus.
Abdominoperineal resection: This is the procedure of choice if the cancer is in the distal third of the rectum (the part nearest to the anus) and especially if it is growing into the sphincter muscle (the muscle that keeps the anus closed and prevents stool leakage). Here the surgeon makes incisions in the abdomen as well as in the perineal area around the anus. Here the anus and the tissues surrounding it including the sphincter muscle are removed. To facilitate removal of stools a permanent colostomy is done.
Surgical procedures used to treat metastatic colorectal cancer may include partial hepatectomy (removal of part of the liver) and oophorectomy (removal of the ovaries).
Some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after surgery to increase the chances of a cure is called Adjuvant Therapy.
Chemotherapy is a cancer treatment that uses medicines to stop the growth of cancer cells, either by killing the cells or by stopping the cells from dividing.
Systemic chemotherapy
Here the medicines are taken by mouth or injected into a vein and enter the bloodstream to reach cancer cells throughout the body.
Regional chemotherapy
Here the medicines are concentrated in areas where there is cancer cell growth. These medicines are injected directly into the spinal column, an organ, or a body cavity such as the abdomen.
Chemotherapy drugs used to treat colorectal cancer include:
- 5-fluorouracil
- Leucovorin
- Irinotecan
- Capecitabine
- Oxaliplatin
Chemotherapy drugs kill cancer cells but also damage some normal cells. The side effects of therapy are:
- Nausea
- Vomiting
- Diarrhea
- Loss of appetite
- Hair loss
- Hand and foot swelling
- Rashes
- Mouth sores
- Increased chances of infection (due to a shortage of white blood cells)
- Bleeding or bruising after minor cuts or injuries (due to a shortage of blood platelets)
- Fatigue (due to low red blood cell counts)
Radiation Therapy:
Radiation therapy uses high energy x-rays to destroy cancer cells and to reduce the size of the tumors.
There are two types of radiation therapy.
- External radiation therapy uses a machine outside the body to send radiation toward the cancer
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer
The type of radiation therapy given depends on the stage of the cancer being treated.
The side effects of Radiation therapy are:
- Fatigue
- Hair loss
- Skin or rectal irritation
- Diarrhea
- Nausea
- Sexual problems
- Burning micturition
Biological Therapy:
Biological therapy causes fewer side effects than chemotherapy drugs.
Cancer cells are different from normal cells. Biological or targeted therapies make use of this principle to attack cancer cells. Because of this, they should cause fewer side effects than chemotherapy drugs.
The medications used in this therapy are:
- Cetuximab
- Panitumumab
- Bevacizumab
Cetuximab was the first targeted therapy approved for treating colorectal cancer. It is a man-made protein called a monoclonal antibody. It specifically attacks the epidermal growth factor receptor (EGFR), a molecule that often appears in high amounts on the surface of cancer cells, thereby causing shrinkage of the tumor. Panitumumab also acts in a similar way.
Bevacizumab is another monoclonal antibody, approved for first-line use against metastatic colorectal cancer. It is used along with chemotherapy drugs. This antibody is directed against vascular endothelial growth factor (VEGF), a protein that helps tumors form new blood vessels.
Clinical trials are in progress to study different combinations of chemotherapy agents and targeted therapies.
Available treatment options for therapy based on staging:
The therapy for colorectal cancer depends upon the extent of tumor spread and the type of tumor.
Since the treatment options rely on the stage of the cancer, recurrence of cancer and the patient's general health, the available options for therapy based on staging are:
Stage 0 colon cancer
Treatment may be one of the following:
- Local excision or simple polypectomy to remove all the cancer
- Bowel resection
Stage I colon cancer
Treatment is usually surgery (bowel resection) to remove the cancer and join the cut ends of the bowel.
Stage II colon cancer
Treatment may be one of the following:
- Treatment is usually surgery (bowel resection) to remove the cancer
- Clinical trials of chemotherapy, radiation therapy, or biological therapy following surgery
- If the tumor has spread to nearby tissue, a patient may also receive chemotherapy and/or radiation therapy following surgery
Stage III colon cancer
Treatment may be one of the following:
- Treatment is usually surgery (bowel resection) to remove the cancer followed by chemotherapy
- Clinical trials of chemotherapy, radiation therapy, and/or biological therapy following surgery
Stage IV colon cancer
Treatment may be one of the following:
- Surgery (bowel resection) to remove the cancer or to make the colon go around the cancer so that it can still work
- Surgery to remove parts of other organs such as the liver, lungs, and ovaries, where the cancer may have spread
- Radiation therapy to relieve symptoms
- Chemotherapy to relieve symptoms
- Clinical trials of chemotherapy or biological therapy
Recurrent colorectal cancer
Depending on the site of recurrence treatment options are:
- Surgery: If the cancer is localized in only one part of the body
- Chemotherapy or radiation therapy: If the cancer has spread to several parts of the body
Follow-up care
It is important after treatment for colorectal cancer to have regular checkups to ensure that changes in health are noticed. If the cancer recurs or develops in another area, it needs to be treated as soon as possible. Checkups may include a physical exam, a fecal occult blood test, a colonoscopy, chest x-rays, and lab tests. Testing for tumor makers namely carcinoembryonic antigen (CEA) and CA 19-9 can detect early recurrences. Between scheduled checkups, a person who has had colorectal cancer should report any health problems to the doctor as soon as they appear.
What is the Prognosis for Colorectal Cancer?
The Prognosis for Colorectal cancer depends on the stage at which it is diagnosed and the treatment given.
The Survival Rates for Colorectal Cancer
Nine out of 10 people, whose colorectal cancer is found and treated at an early stage, before it has spread, live at least for five years. The 5-year survival rate is the percentage of patients who are alive 5 years after their cancer is detected. Once the cancer has spread to nearby organs or lymph nodes, the 5-year survival rate goes down. Some patients might live more than 5 years after their cancer is detected.
Colon cancer survival rates are based on the American Joint Committee on Cancer (AJCC) staging system, which divides stages II and III into sub-stages. Rectal cancer survival is about the same.
- Stage I - 93%
- Stage IIA - 85%
- StageIIB - 72%
- Stage IIIA - 83%
- Stage IIIB - 64%
- Stage IIIC - 44%
- Stage IV - 8%
The statistics give an overall picture and the survival rates could vary for different individuals.
How do you Prevent Colorectal Cancer?
Healthy lifestyle measures and regular screening can help prevent colorectal cancer.
The measures to be adopted are:
- Screening: Get screened regularly beginning at age 50. If there is a family history of colorectal cancer or inflammatory bowel disease then the screening begins earlier
- High fiber diet: Eat plenty of vegetables, fruits and high-fiber foods. It is recommended to include at least five servings of fruits and vegetables each day and several servings of other food from plant sources such as breads, cereals, grains, rice, pasta, or beans
- Low fat diet: Avoid foods that are high in fat. A low-fat, high-fiber diet with plenty of fruits and vegetables can prevent colorectal cancer and provide additional health benefits
- Ideal body weight: Exercise and maintain a normal body weight. Since obesity has been identified as a risk factor for colorectal cancer, maintaining a healthy weight can reduce this risk
- Diet: Eating a low fat diet and getting regular exercise are excellent ways to stay fit
- Smoking and alcohol: Avoid smoking or smoke and drink alcohol only in moderation. Studies indicate that smokers are 30 to 40 percent more likely than nonsmokers to develop colorectal cancer because they are more likely to develop polyps
- Some studies suggest that taking a daily multivitamin with folic acid may also lower risk for colorectal cancer. Others indicate that getting more calcium, either via supplements or calcium-rich foods, may have a beneficial effect.