- Craniosynostosis - (http://www.mayoclinic.org/diseases-conditions/craniosynostosis/home/ovc-20256651)
- Craniosynostosis - Overview - (http://www.chw.org/medical-care/neuroscience/conditions/craniosynostosis/)
- Twigg SRF, Wilkie AOM. A genetic pathophysiological framework for craniosynostosis. AJHG. 2015;97(3):359-377.
- Heuzé Y, Holmes G, Peter I, Richtsmeier JT, Jabs EW. Closing the Gap: Genetic and Genomic Continuum from Syndromic to Nonsyndromic Craniosynostoses. Current genetic medicine reports. 2014;2(3):135-145. doi:10.1007/s40142-014-0042-x
- Panigrahi I. Craniosynostosis genetics: The mystery unfolds. Indian Journal of Human Genetics. 2011;17(2):48-53. doi:10.4103/0971-6866.86171
- Ko JM. Genetic Syndromes Associated with Craniosynostosis. Journal of Korean Neurosurgical Society. 2016;59(3):187-191. doi:10.3340/jkns.2016.59.3.187
- Kabbani H, Raghuveer TS. Craniosynostosis. 2004;69(12):2863-2870.
What is Craniosynostosis?
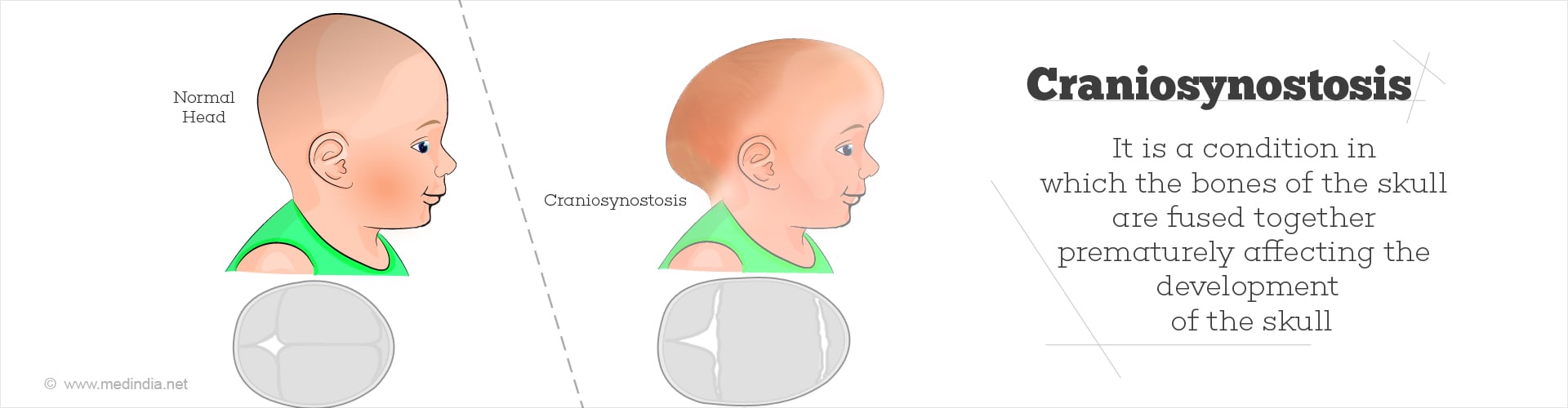
Craniosynostosis is a condition where the bones of the skull prematurely fuse together either in the womb or soon after birth. Craniosynostosis hampers the development of the skull and, in some cases, the brain. The skull, at birth, consists of bones that are connected by fibrous tissue called sutures. These sutures begin to close gradually by the age of 2 in the child’s development to form the skull.
What is the Normal Growth Pattern of the Head?
There are 7 bones in the normal skull of a baby. There are 4 fibrocellular tissues or sutures (coronal, sagittal, lambdoid, and metopic) that connect and fuse the bones by the age of 2. Cranial sutures coordinate the growth of the skull with the developing brain.
What are the Types of Craniosynostosis?
There are different types of craniosynostosis based on the suture that is affected and the resulting shape of the skull. The different types of craniosynostosis are classified as follows:
- Sagittal synostosis (40% - 55%)
- Coronal synostosis (20% - 25%)
- Metopic synostosis (5% - 15%)
- Lambdoid synostosis (<5%)
What are the Causes of Craniosynostosis?
Craniosynostosis predominantly occurs by chance (sporadic) most probably due to a combination of genetic and environmental factors; this type is called nonsyndromic craniosynostosis.
It can also be caused due to the inheritance of specific genes; there are more than 180 genetic syndromes that are known to be associated with this type of craniosynostosis, and hence it is named syndromic craniosynostosis.
Out of the 2500 craniosynostosis live births, 85% of these births are nonsyndromic craniosynostosis, while 15% of the patients have syndromic craniosynostosis.
Some of the syndromes associated with syndromic craniosynostosis are:
- Crouzon syndrome
- Saethre-Chotzen syndrome
- Apert syndrome
- Greig cephalopolysyndactyly
- Pfeiffer syndrome
- Antley-Bixler syndrome
- Muenke syndrome
- Craniofrontonasal syndrome
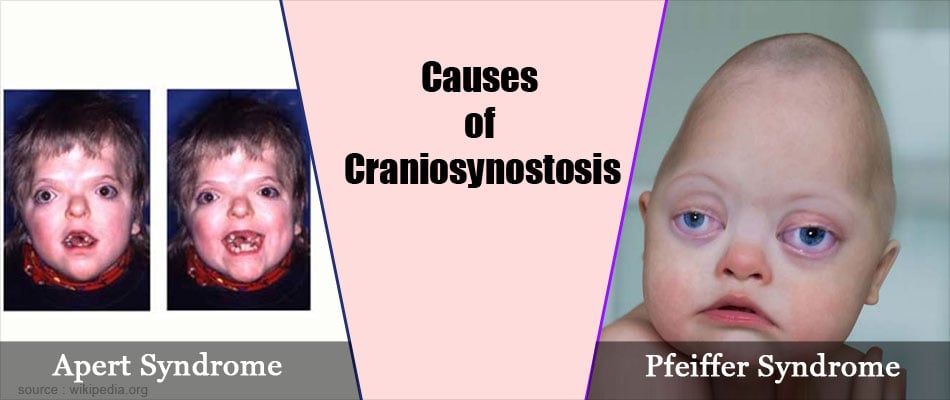
The genetic mutations in these disorders or syndromes occur in fibroblast growth factor receptor genes
- TWIST1
- FGFR1
- FGFR2
- FGFR3
- EFNB1
What are the Symptoms of Craniosynostosis?
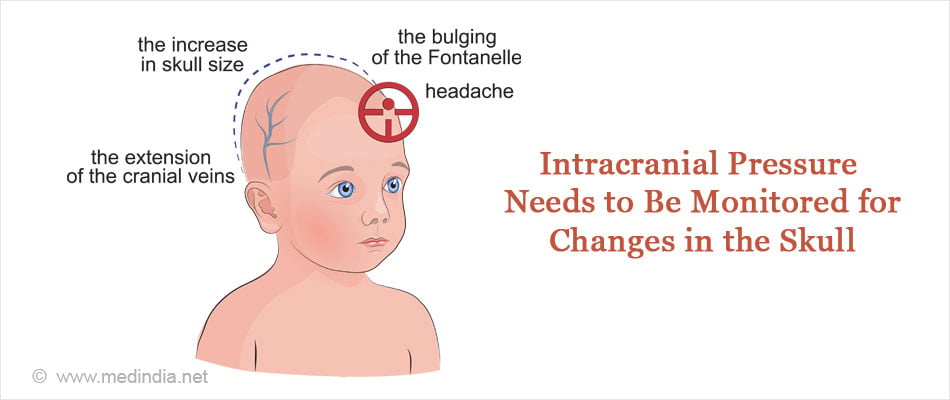
Craniosynostosis can be detected by the following signs at birth or progressively during the initial months of a baby’s life:
- Affected sutures determine the irregularities in the skull shape
- Ocular hypertelorism or widely-spaced eyes
- Beak-shaped nose
- Bulging eyes or proptosis
- Limited or no progress in head growth with the growth of the baby
- The baby’s skull does not feel normal due to a disappearing fontanel
- A hard ridge develops as a raised structure along the sutures
How do you Diagnose Craniosynostosis?
Craniosynostosis is difficult to diagnose when it is a mild condition. The best way to diagnose the condition is with a physical examination.
Clinical examination: An abnormally-shaped head with ridging at the suture lines is indicative of craniosynostosis. Infants with craniofacial abnormalities should have their toes, digits, spine, and neck examined in the case of syndromic craniosynostosis.
In Apert’s syndrome, the diagnostic features include abnormalities within the brain (e.g. accumulation of fluid in the brain), misshapen skull, widely spaced eyes, shallow orbits, and abnormal development of the midface.
Crouzon’s syndrome is diagnosed with hydrocephaly, widely spaced bulging eyes, and abnormalities within the brain. Infants are not affected in their hands and feet.
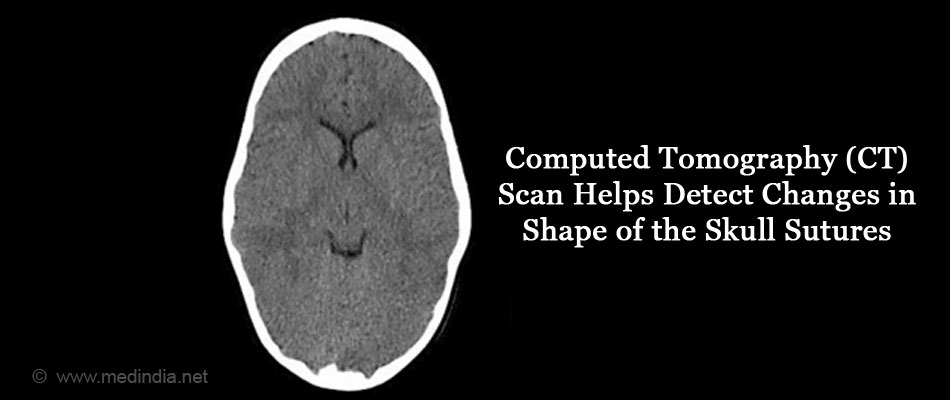
Radiographic examination: Radiography helps to detect craniosynostosis due to single sutures. The examination helps to detect changes in the thickness and shape of the suture that will help diagnose the condition. Computed tomography (CT) provides a 3-dimensional view of the brain allowing for surgical reconstruction. Accurate identification of the sutures is possible with a CT scan.
How do you Treat Craniosynostosis?
Surgery (preparation before, during and after):
The best way to treat craniosynostosis is with a multidisciplinary approach, for example, surgery in collaboration with clinical psychology and speech therapy. Once the condition is diagnosed, craniosynostosis is ideally treated with surgical intervention. The skull is remodeled to provide extra volume for the brain. Surgical correction in infants is normally between the ages of 3 and 9 months. Increased intracranial pressure should immediately be treated with decompression. The neurosurgeon and the craniofacial surgeon are involved in deciding the appropriate treatment. There are 2 types of surgical procedures: open surgery and endoscopic surgery.
The surgical interventions for nonsyndromic craniosynostosis involve correcting defects in limbs between the ages of 1 and 2. Craniosynostosis is corrected between the ages of 3 and 6 months through endoscopic surgery. Open surgery is performed on babies older than 6 months. Young adults are surgically treated to correct dental malformations and facial abnormalities.
Helmets are required to provide shape to the skull. Helmets are used following endoscopic treatment. However, helmets are not required if there is open surgery.
In mild cases, surgery is not required. Doctors recommend a helmet if the sutures are open. This gives the brain a chance to develop and eliminates the abnormal shape of the head.
How do you Prevent Craniosynostosis?
It is necessary to monitor the patient regularly for any changes in intracranial pressure and circumference of the head. It is also essential to confirm that the sutures do not fuse again.