- DiGeorge Syndrome - Immune Deficiency Foundation (IDF) - (https://primaryimmune.org/about-primary-immunodeficiencies/specific-disease-types/digeorge-syndrome)
- 22q11.2 Deletion Syndrome - Genetic Home Reference (GHR), U.S. National Library of Medicine, National Institutes of Health (NIH), USA - (https://ghr.nlm.nih.gov/condition/22q112-deletion-syndrome#)
- DiGeorge Syndrome (22q11.2 Deletion Syndrome) - (https://www.mayoclinic.org/diseases-conditions/digeorge-syndrome/symptoms-causes/syc-20353543)
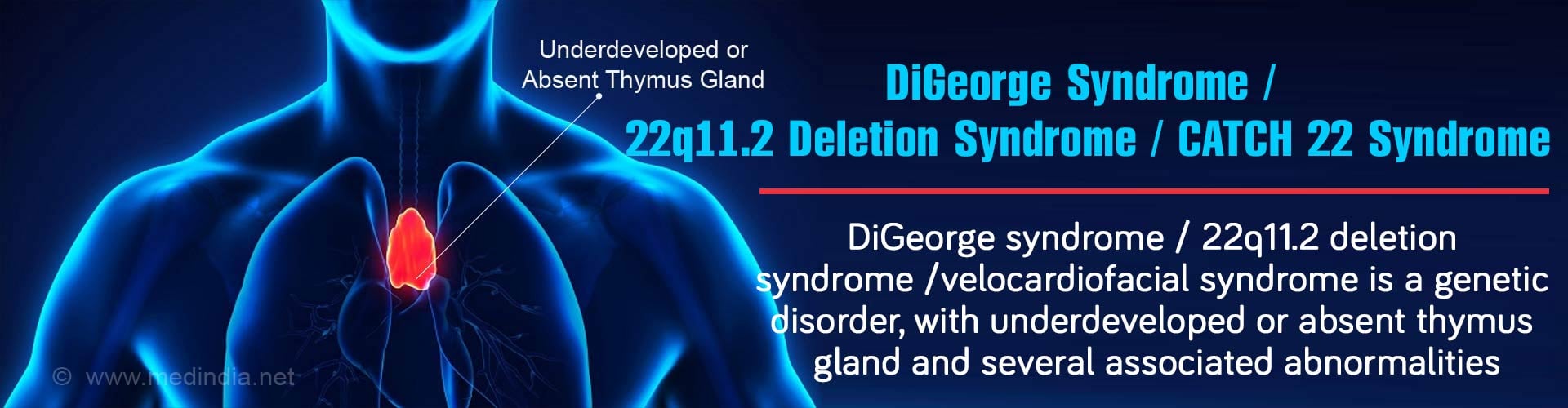
What is DiGeorge Syndrome?
DiGeorge syndrome, also known as 22q11.2 deletion syndrome, is a genetic disorder caused by a small deletion in chromosome 22 at position q11.2. The condition is usually not passed on from parents to the child except in some cases. Most cases occur spontaneously without any identifiable cause even when both parents are normal.
The 22q11.2 deletion is the most common type of deletion in humans and is characterized by hypocalcemia (due to hypoparathyroidism), heart defects, and thymus abnormalities. These patients also experience recurrent infections caused by primary immunodeficiency, often resulting in the development of autoimmune disorders such as rheumatoid arthritis and Graves’ disease.
The syndrome is named after the Italian American physician and pediatric endocrinologist, Dr. Angelo M. DiGeorge, who first described the condition in 1968. The underlying genetic cause was established in 1981.
Clinical Features of DiGeorge Syndrome
DiGeorge syndrome is also known by a variety of other names, including velocardiofacial syndrome (VCFS) and conotruncal anomaly face (CTAF) syndrome. Interestingly, the syndrome has an acronym, known as "CATCH 22", which describes the major clinical features of the syndrome:
"CATCH 22"
- Cardiac abnormalities
- Abnormal facies
- Thymic abnormalities
Cleft palate - Hypocalcemia
- Chromosome 22
Epidemiology of DiGeorge Syndrome
DiGeorge syndrome has an incidence of 1 in 3000 live births. Approximately 90% of 22q11.2 deletions occur spontaneously during fetal development, while 10% are inherited from a parent. It is an autosomal dominant disorder, which means that a defect in a single chromosome in each cell is sufficient for occurrence of the disorder.
What are the Causes of DiGeorge Syndrome?
The primary cause of DiGeorge syndrome is 22q11.2 deletion, which largely occurs randomly without any identifiable cause. However, in case of about 5-10% children, the 22q11.2 deletion is inherited from a parent suffering from a mild – often undiagnosed – form of DiGeorge syndrome. Because the symptoms of this disorder are so variable, even patients from the same family may present with different clinical features.
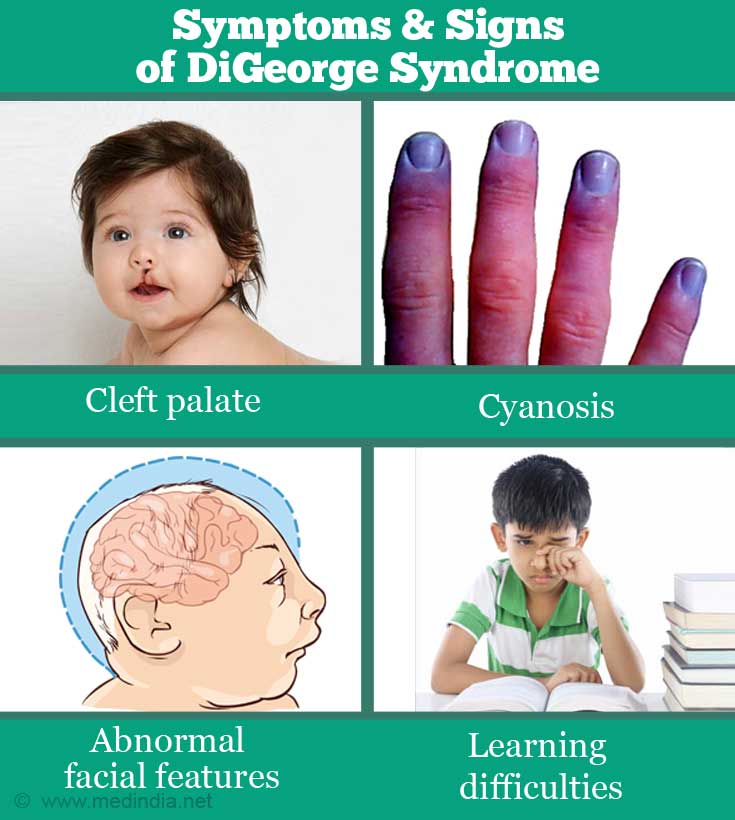
What are the Symptoms & Signs of DiGeorge Syndrome?
The symptoms and signs of DiGeorge syndrome are associated with defects in several organ systems of the body as well as other anomalies. These include the following:
- Cleft palate i.e. a split in the roof of the mouth that causes feeding difficulties and speech difficulties when the child becomes older.
Cyanosis i.e. a bluish discoloration of the skin due to poor circulation or inadequate oxygenation of the blood.Hearing loss - Hypocalcemia, which can cause seizures and shaking episodes and muscle spasms.
- Developmental defects e.g. delay in growth and speech.
- Abnormal facial features e.g. small mouth / upper lip / jaw; low-set and/or abnormally folding ears.
- Thymus gland abnormalities such as lowered T-cell production with increased risk of getting infections such as chest infections, ear infections and oral thrush. This is because the body’s defense system (immune system) is weak and does not function properly.
- Learning difficulties e.g. cognitive deficits and attention deficit disorders.
- Mental and behavioral disorders e.g. susceptibility to mental health conditions such as schizophrenia and bipolar disorder.
How do you Diagnose DiGeorge Syndrome?
DiGeorge syndrome can be diagnosed based on the following strategies:
- Clinical Evaluation: Observation of the baby’s facial features by a doctor will help to make a presumptive diagnosis. These features include (i) cleft palate, (ii) underdeveloped jaw, (iii) thin upper lip, (iv) small mouth, (v) upward or downward slanting eyes, (vi) small head, (vii) epicanthal folds, (viii) smooth philtrum, (ix) small eye openings, (x) short nose, and (xi) low nasal bridge.
- Echocardiography: This procedure is used to detect any heart defects associated with DiGeorge syndrome.
- Blood Tests: These measure the blood calcium level to see whether there is a deficit of calcium (hypocalcemia), which is a characteristic symptom of DiGeorge syndrome. The ESR (erythrocyte sedimentation rate) can be determined to see if there is any infection, as DiGeorge syndrome patients are more prone to infections.
- Immunological Tests: Thymus gland function can be evaluated by doing a TC (total count) and DC (differential count) on a blood sample to see the levels of white blood cells or leucocytes (including lymphocytes). A subpopulation of lymphocytes (T lymphocytes or T cells) have a surface marker called CD4, which help to determine the levels of T cells in the blood. A low level of T cells indicates thymus gland dysfunction.
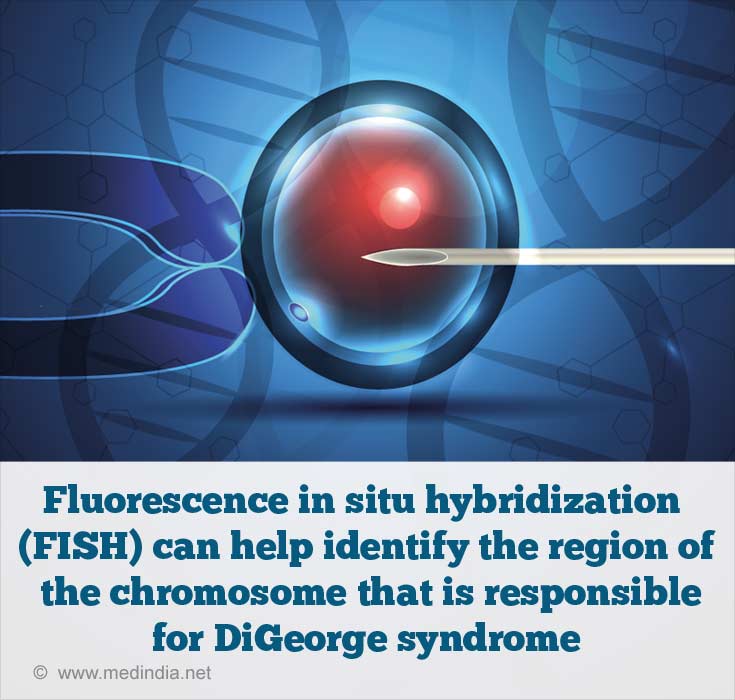
- Fluorescence in situ Hybridization (FISH): This is very powerful genetic testing method in which fluorescent probes (DNA or RNA fragments) are used to identify the region of the chromosome that is responsible for DiGeorge syndrome. The FISH test can be carried out on a blood sample from a baby after birth, or on amniotic fluid obtained before birth by
amniocentesis . - Chromosomal Microarray: This is similar to the FISH test, except that it scans all the chromosomes to look for defects in the genes. For example, in case of chromosome 22, the missing gene can be specifically mapped to the q11.2 location.
How do you Treat DiGeorge Syndrome?
- Treatment is aimed at correcting the defects in the affected tissues and organs. Since the tissues and organs involved and the severity of the complications vary, treatments must be personalized.
- For example, mild T cell defects can be treated with antibiotics and close follow-up. However, in severe T cell impairment, bone marrow and/or thymus transplantation may be required.
- Severe defects associated with the heart and facial abnormalities may require corrective surgery.
- Hypocalcemia and hypoparathyroidism can be treated by calcium supplementation and parathyroid hormone replacement, respectively.
Importantly, children with DiGeorge syndrome will benefit appreciably from a multi-specialty approach to treatment, since this disorder is usually associated with a spectrum of complications. These fall under various different medical specialties including cardiology, ENT, immunology, endocrinology, neurology, urology, genetics, psychology, psychiatry, speech therapy, and physiotherapy.
What is the Prognosis for DiGeorge Syndrome?
The outlook for babies with DiGeorge syndrome depend on the condition of the various organ systems, particularly the severity of heart complications. Advancements in heart surgery and strategies to manage immunodeficiency disorders have reduced the mortality rate to 4%. As a result, most children survive into adulthood. As the patient gets older, the heart and speech problems usually subside, but learning, behavioral and mental symptoms remain a problem in daily life. It has been observed that early diagnosis and treatment improves the prognosis appreciably.
DiGeorge Syndrome Support Groups
There are many DiGeorge syndrome support groups around the world which have vast knowledge resources for providing useful advice on finding ways to cope with the disorder. These groups also aim to spread awareness about the disorder and provide psychological support to families having an affected child. One such support group in the UK is Max Appeal (http://www.maxappeal.org.uk/).