- G6PD Deficiency - (https://www.hopkinsmedicine.org/healthlibrary/conditions/hematology_and_blood_disorders/g6pd_glucose-6-phosphate_dehydrogenase_deficiency_85,P00091)
- Kumar and Clark’s Clinical Medicine 7th Ed - (https://www.hopkinsmedicine.org/healthlibrary/conditions/hematology_and_blood_disorders/g6pd_glucose-6-phosphate_dehydrogenase_deficiency_85,P00091)
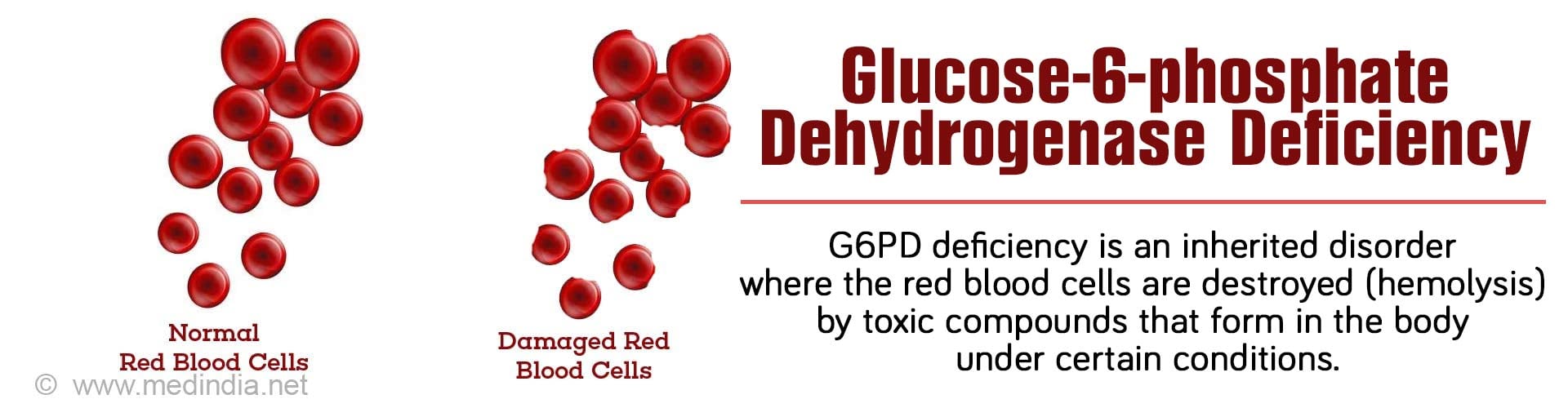
What is Glucose-6-phosphate dehydrogenase Deficiency?
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is a genetic disorder caused due to a defect in an enzyme called glucose-6-phosphate dehydrogenase that causes red blood cells to break down prematurely.
G6PD is an enzyme that protects the red blood cells from damage and destruction by harmful and toxic compounds that form in the body under certain conditions like stress, fever, or following the ingestion of certain foods or drugs. The enzyme generates compounds that can neutralize the toxic compounds formed in the body.
G6PD deficiency is a fairly common disorder that affects several people worldwide. It is more common in Africa, the Mediterranean, Middle East and Southeast Asian regions.
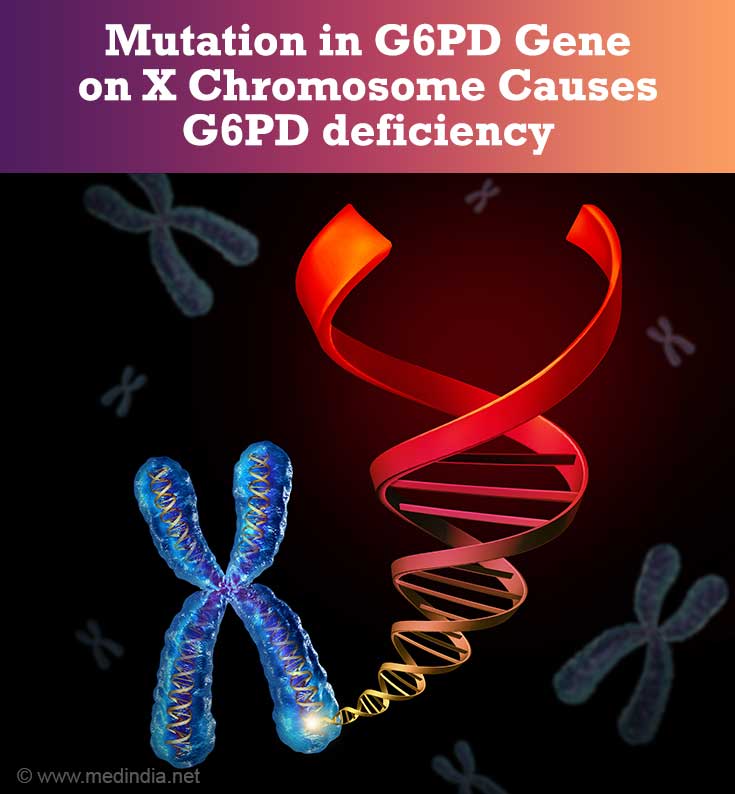
What are the Causes of G6PD Deficiency?
G6PD deficiency occurs due to mutations in the G6PD gene, which encodes for the G6PD enzyme. The G6PD gene is located on the X chromosome. The mode of inheritance is X-linked recessive. The symptoms of G6PD deficiency manifests more commonly in males, while females can be silent carriers of the disease.
There can be several types of mutations associated with reduced G6PD enzyme activity. The most common variant is the A-type seen in Africans and results in a milder form of hemolysis. The other variant is the Mediterranean type characterized by severe enzyme deficiency and associated with severe hemolysis that may result in death unless the condition is recognized promptly and the person given an urgent blood transfusion.
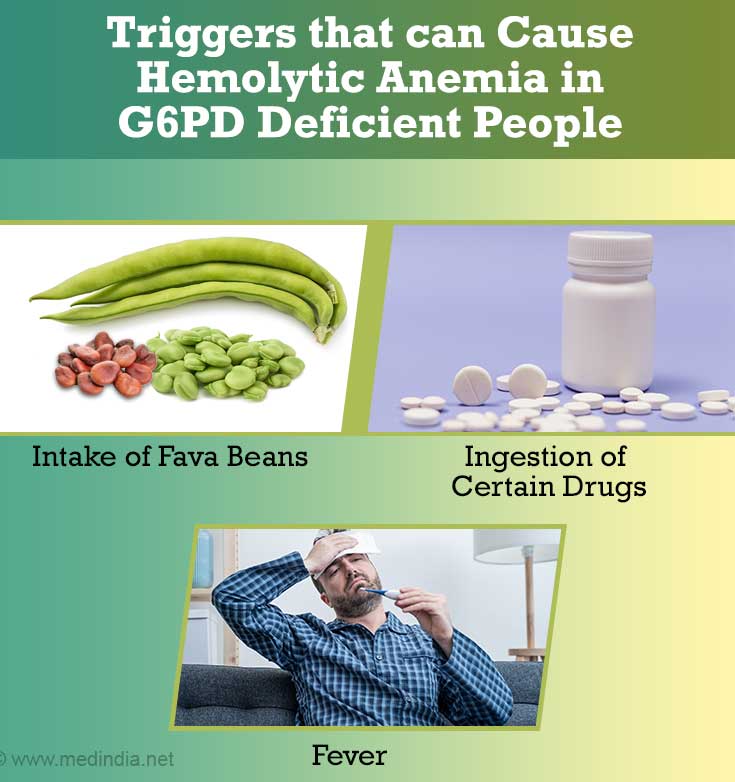
How does a Hemolytic Crisis occur in G6PD deficiency?
Normally, when a person develops infections, fever or other stressful conditions, certain toxic chemicals called reactive oxygen species are generated that can cause damage and breakdown of red blood cells. This is prevented by protective compounds (produced by normal G6PD enzyme activity) which neutralize and remove the toxic compounds produced in the body during such situations.
Symptoms of Hemolytic Crisis
- In G6PD deficient individuals, the protective effect of this enzyme is missing.
- Thus, situations such as fevers, ingestion of certain drugs such as aspirin, antimalarial drugs, certain antibiotics and other drugs, ingestion of foods such as fava beans cause the circulating red cells to breakdown with release of its hemoglobin (intravascular hemolysis).
- Part of the released hemoglobin pigment (which is red in color) is excreted in the urine giving the urine a dark brown color (hemoglobinuria).
- Some of the hemoglobin is processed in the liver and converted to bilirubin. The high bilirubin levels result in jaundice with yellowish discoloration of the skin and eyes.
- At the same time, since oxygen transport to the various parts of the body is affected due to destruction of red blood cells, the person becomes anemic, tired and breathless.
If the condition is not recognized promptly and blood transfused immediately, it may sometimes result in death.
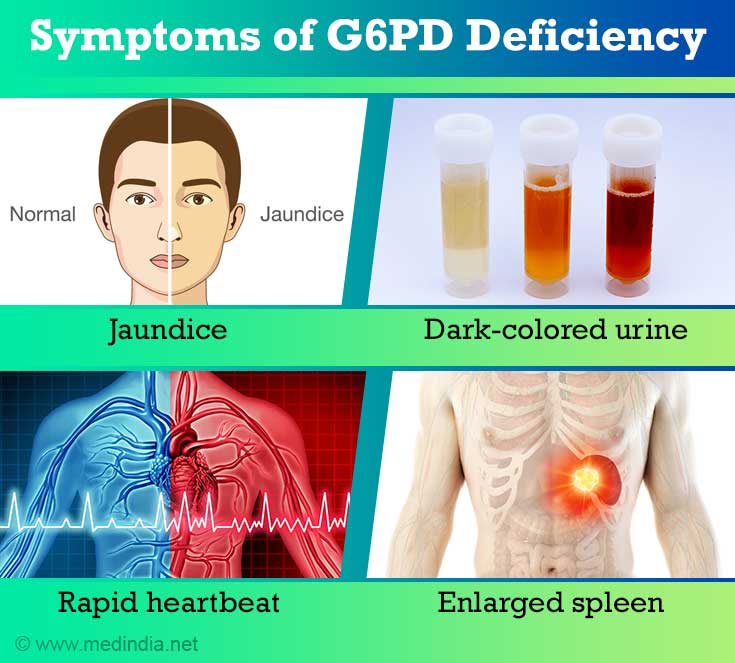
What are the Symptoms of G6PD Deficiency?
The clinical features of G6PD deficiency include varying severity of hemolytic symptoms (see above) depending on the degree of G6PD deficiency. The hallmark of the condition is sudden hemolysis following the intake of a drug, fava beans, or conditions like fever or infections resulting in anemia, jaundice and hemoglobinuria. Most persons have only mild hemolysis. Severe life-threatening hemolysis is fortunately rare. The clinical features may also include:
- Tiredness and dizziness
- Paleness
- Confusion
- Enlarged spleen
- Chronic hemolytic anemia in mild G6PD deficiency
- Prolonged jaundice in the newborn due to G6PD deficiency
- Dark-colored urine
- Rapid heartbeat
Drugs Causing Hemolysis in G6PD Deficiency
The following drugs can cause hemolysis in a patient with G6PD deficiency and should be strictly avoided:
| Drug Type | Names of Drugs |
| Analgesics | Aspirin, Phenacetin |
| Antimalarials | Primaquine, Chloroquine, Quinine, Pyrimethamine, Pamaquin |
| Antibacterials | Sulphonamides, Dapsone, Quinolones, Nitrofurantoin, Chloramphenicol |
| Miscellaneous | Dimercaprol, vitamin K, Probenecid, Quinidine |
Exposure to mothballs containing naphthalene should also be avoided.
How to Diagnose G6PD Deficiency?
The diagnosis of G6PD deficiency is based on the following:
History
The diagnosis of G6PD deficiency may be made from a careful drug and food intake history with symptoms of jaundice, tiredness and passing dark colored urine following ingestion of certain drugs or foods. Previous history of such episodes may also be reported. The patient is normal between episodes. Details of the ethnicity (especially for patients of African or Mediterranean origin) may be a valuable clue.
Blood tests
Blood tests may reveal low red blood cell count, increased bilirubin levels, and increased plasma hemoglobin levels. Other blood tests may confirm presence of intravascular hemolysis. However, the blood tests may be normal between the attacks.
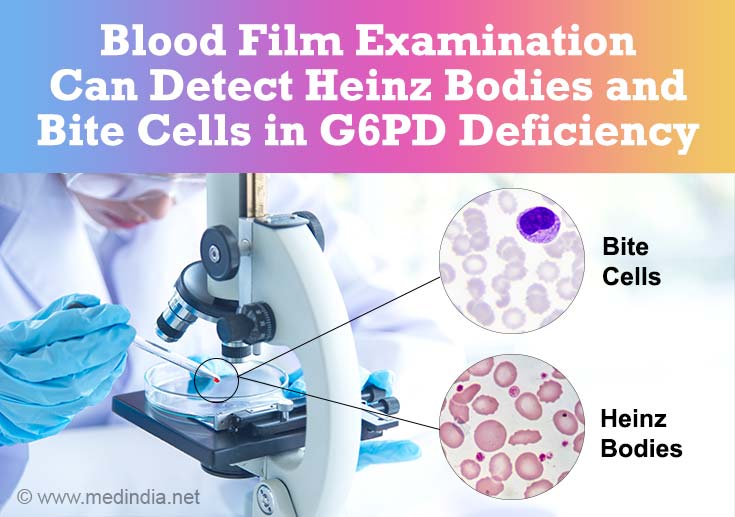
Blood film examination
Examination of a stained blood film under the microscope may show abnormal broken red cells (hemolytic RBCs). Special stains show denatured hemoglobin within red cells (Heinz bodies) and increased immature red cells (reticulocytes) due to formation of new red cells (erythropoiesis) by the bone marrow as compensatory response. If the abnormal cells have the appearance of a bitten piece they are termed bite cells.
Urine tests
The urine specimen during the attack is dark colored and positive for hemoglobin and hemosiderin
Screening tests to detect low G6PD levels
Several screening tests are available that demonstrate the decreased capacity of G6PD deficient cells to reduce dyes. The enzyme can also be directly assayed.
How to Treat G6PD Deficiency?
- Stop any offending drug the person may be taking immediately
- Treat any underlying infection with safe antibiotics
- Blood transfusion may be required depending on the degree of anemia
- Severe favism may need exchange transfusion
- Newborn infants with prolonged neonatal jaundice should receive phototherapy or exchange transfusion if appropriate (rapidly rising bilirubin levels) to prevent brain damage (kernicterus)
- Folic acid supplements should be given to persons with chronic hemolysis
- Long-term follow-up with a hematologist is necessary to prevent future attacks. It is important for the patient to inform treating physicians about the diagnosis and check with them before starting any new drug
- Recent evidence suggests that vaccination of G6PD deficient patients against hepatitis A and B may be useful in preventing severe hemolytic complications if they develop these infections.
Unlike other causes of hemolytic anemia, splenectomy will not be useful in G6PD deficiency.
How to Prevent G6PD Deficiency?
As G6PD deficiency is an inherited disorder, it cannot be prevented but persons with known G6PD deficiency may benefit from genetic counseling.
The important thing is to avoid triggers such as foods and drugs known to precipitate hemolysis.