- Hepatorenal Syndrome - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc1904420/)
- Hepatorenal Syndrome: Aetiology, Diagnosis, and Treatment - (http://dx.doi.org/10.1155/2015/207012)
- Arroyo V, Fernandez J, Gines P. Pathogenesis and Treatment of Hepatorenal Syndrome. Seminars in Liver Disease 2008; 28(1): 81-95.Schepke M. Hepatorenal syndrome: current diagnostic and therapeutic concepts. Nephrol. Dial. Transplant. (2007) 22 (suppl 8): viii2-viii4.doi: 10.1093/ndt/gfm656
- Kiser TH. Hepatorenal Syndrome. International Journal of Clinical Medicine Vol.5 No.3(2014), Article ID:42456,9 pages DOI:10.4236/ijcm.2014.53018
- Giné s P, Guevara M, Arroyo V, Rodé s J. Hepatorenal syndrome. The Lancet 2003; 362 (9398):1819-1827
What is Hepatorenal Syndrome?
Hepatorenal syndrome refers to functional kidney failure that may occur in patients suffering from cirrhosis (advanced liver disease) with ascites (fluid accumulation in the abdominal cavity). Hepatorenal - Hepato refers to the liver while renal refers to the kidneys. The kidneys are structurally normal i.e. there is no primary kidney disease accounting for the kidney failure.
The diagnosis of hepatorenal syndrome is based on a combination of clinical and laboratory parameters. Liver transplantation is the definitive form of treatment, which may provide the chance of a recovery. Short-term therapies aim to prolong patient survival, enabling them to undergo a liver transplant.
How is Hepatorenal Syndrome Caused?
The liver receives blood from two main sources, the portal vein which brings nutrient-rich blood (which also contains toxins and drugs) to the liver from the digestive tract and the hepatic arteries, which provide additonal oxygen of the liver. The hepatic arteries form a part of the splanchnic circulation, which also supplies oxygen-rich blood to other abdominal organs like the stomach, intestines, pancreas and spleen.
Typically, patients who go on to develop hepatorenal syndrome suffer from portal hypertension due to advanced liver conditions like cirrhosis, alcoholic liver disease, or metastatic tumors. It has also been described in patients with acute liver disease.
Most patients with hepatorenal syndrome are in their 60’s or 70’s with a male preponderance.
The most widely accepted theory to explain the development of hepatorenal syndrome is the ‘peripheral arterial vasodilation’ theory. The theory has been simplified and presented below for easy understanding:
- Advanced liver disease causes high blood pressure in the portal circulation, referred to as portal hypertension. This causes the release of several blood vessel-relaxing substances like nitric oxide which dilate the splanchnic circulation.
- The dilation of the splanchnic circulation results in pooling of blood in the splanchnic vascular bed, thereby reducing the effective volume of blood in circulation.
- In initial stages, the heart tries to maintain the blood flow in the body.
- With progression of cirrhosis, there is further pooling of blood in the splanchnic bed, and decrease in the capacity of the heart to maintain the blood flow to the body. The heart muscle may also be weakened due to advanced cirrhosis.
- The reduced blood flow to the body results in activation of neurohormonal mechanisms like the Renin Angiotensin Aldosterone (RAA) system, the sympathetic system and the release of arginine vasopressin.
- These systems tighten the vessels of the kidney, brain and peripheral circulations. In addition, they cause salt and water retention.
- Initially, compensatory mechanisms within the kidney, like the release of prostaglandins, help to maintain kidney blood flow.
- When the compensatory renal mechanisms fail in due course, the blood vessels of the kidney undergo severe tightening, leading to a severe decrease in kidney blood flow and functional kidney failure, termed as hepatorenal syndrome.
What are the Types of Hepatorenal Syndrome?
HRS can be divided into types 1 and 2.
Type 1 HRS is more serious, and characterized by a rapid and progressive decline of renal function, indicated by a doubling of the initial serum creatinine to more than 2.5 mg/dL in less than 2 weeks. The Glomerular Filtration Rate (GFR) is also typically less than 20 ml/min. The average duration of survival is less than 2 weeks and most patients die within 8–10 weeks following the onset of kidney failure.
Type 2 HRS follows a less dramatic clinical course with serum creatinine levels between 1.5 and 2.5 mg/dL. The predominant clinical effect of type 2 HRS is diuretic-resistant ascites (fluid accumulation in the abdominal cavity), that is, the ascites does not reduce on intake of water-losing pills. Patients show an average duration of survival of approximately 6 months.
What are the Clinical Features of Hepatorenal Syndrome?
Clinical features of hepatorenal syndrome reflect the underlying liver disease, impaired kidney function and circulatory abnormalities that are a part of the condition.
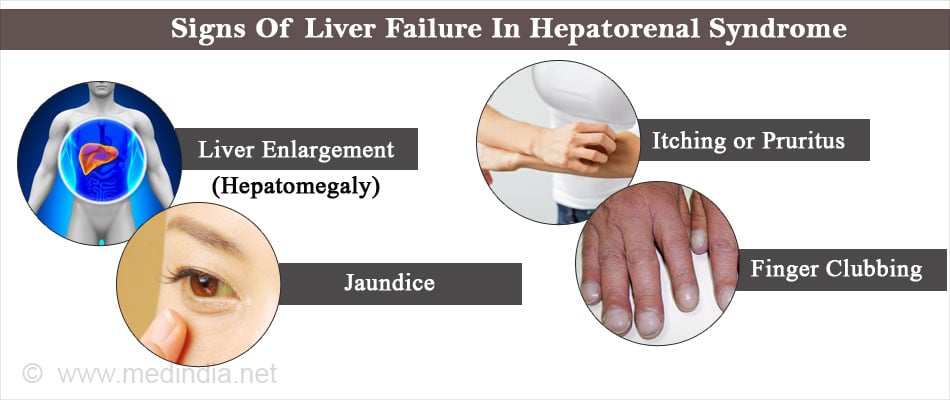
Signs of liver failure in HRS
- Liver enlargement (hepatomegaly)
- Ascites
- Jaundice
- Itching or pruritus
- Features of portal hypertension (e.g. dilated blood vessels at the base of the food pipe and around the belly button, and depression of brain functions)
- Clotting abnormalities
- Enlarged breasts in men (gynecomastia)
- Finger clubbing (changes in the nails associated with liver disease)
- Reddish discoloration of palms (palmar erythema) and beneath the skin (spider nevi)
- Generalized disturbances such as weakness, exhaustion, loss of appetite, and poor nutritional status
Signs of Kidney Impairment
- Kidney impairment causes a decrease in urine output. The urine output is reduced suddenly in type 1 HRS, while the decrease is slower in type 2 HRS.
- Blood tests demonstrate a progressive increase in serum creatinine levels, which indicates kidney impairment
- The urine sediment may be normal and the patient may have absent or minimal proteinuria (protein in the urine)
Circulatory Abnormalities in HRS
Problems in blood circulation may be reflected clinically as:
- Increased heart rate with a bounding or high volume pulse
- Low mean arterial pressure (MAP)
- Low jugular venous pressure (JVP). The jugular vein drain the head region
- Wide pulse pressure. The pulse pressure is the difference between the systolic and diastolic blood pressures
Blood tests may also reveal other abnormalities like:
- Increased plasma renin activity
- Elevated plasma noradrenaline activity
- Elevated blood urea nitrogen
- Low plasma sodium level
- Elevated serum potassium (hyperkalemia)
- Decreased plasma osmolality
- Elevated urinary osmolality, and decreased urinary sodium excretion
- Increased serum bilirubin
- Reduced serum albumin
- Prolonged prothrombin time
What is the Treatment of Hepatorenal Syndrome?
Treatment of decreased liver function results in improvement of hepatorenal syndrome. The liver function can be improved by:
- Abstinence of alcohol by alcoholics

- Treatment of hepatitis B with antiviral medications
- Treatment of hepatic failure with medications or ultimately liver transplantation
However, if the improvement of liver function is not possible in the short-term, medical treatment should be initiated in an attempt to reverse the associated kidney function impairment and to raise the mean arterial pressure. Regular monitoring of fluid intake, urinary output and serum chemistries are necessary in these patients.
Vasoconstrictor Therapy: Vasoconstrictor drugs tighten blood vessels and increase blood pressure.
- Epinephrine in combination with albumin is given to hepatorenal syndrome patients who are very sick. Intravenous vasopressin is also used in certain cases to maintain the mean arterial pressure.
- In less critically ill patients, albumin may be administered with terlipressin when available. If terlipressin is unavailable, midodrine or octreotide is given as initial treatment along with albumin.
Transjugular intrahepatic portosystemic shunt
In patients who don’t respond to the above treatment, and if they are fit enough, a procedure called transjugular intrahepatic portosystemic shunt (TIPS) may be tried and might be successful. In this procedure, a stent is introduced through a neck vein to connect the portal vein to a hepatic vein. This reduces the portal vein pressure and improves blood circulation. However, the procedure is associated with many complications and may even cause kidney damage since contrast material is used.
Dialysis
- Many experts prefer dialysis as the first option in cases that fail to respond to medical therapy described above, and especially when serum creatinine remains above 1.5 mg/dl. Hemodialysis may be useful in patients fit for liver transplant who develop problems like metabolic acidosis, volume overload or refractory hyperkalemia (high blood potassium levels that does not respond to treatment).
How can Hepatorenal Syndrome be Prevented?
- Proper fluid management is necessary in patients with advanced liver disease to prevent kidney disease.
- Patients with an abdominal infection called spontaneous bacterial peritonitis are at a higher risk of developing hepatorenal syndrome. Administration of albumin in these patients could prevent the circulatory dysfunction and subsequent development of HRS. The reason is that it can prevent the reduction in blood volume and arterial underfilling with subsequent activation of vasoconstrictor mechanisms.
- A study found that that the use of an antibiotic such as cefotaxime in combination with albumin was associated with a lower risk of HRS development in patients with spontaneous bacterial peritonitis than when cefotaxime was administered alone.
- A drug called pentoxifylline, had been shown to reduce the incidence of HRS in patients with liver disease.

What is the Prognosis of Hepatorenal Syndrome?
In general, the death rate of patients with liver failure is significantly higher if they develop hepatorenal syndrome. In the absence of treatment, most patients die within a few weeks following the appearance of renal failure. The prognosis may improve in patients with improvement of liver failure which may occur either spontaneously, following medical treatment, or following a successful liver transplantation.
Conclusion
Ever since the existence of the entity of HRS was recognized over a century ago, significant progress has been made in the understanding of its causes and natural course. Standard diagnostic criteria have been evolved aiding uniform diagnosis and accurate reporting of the disease. However, a major drawback is the absence of a reliable diagnostic marker for HRS. Such a marker could help in the early diagnosis and help to initiate treatment early, and improve patient outcome.