- Before, During & After Surgery - (http://www.fda.gov/medicaldevices/productsandmedicalprocedures/implantsandprosthetics/phakicintraocularlenses/ucm059240.htm)
- Intraocular lens - (https://en.wikipedia.org/wiki/intraocular_lens#materials)
- IOL Implants: Lens Replacement and Cataract Surgery - (https://www.aao.org/eye-health/diseases/cataracts-iol-implants)
- Cataract and Intraocular Lens Implantation in Cataract Surgery - (http://my.clevelandclinic.org/health/articles/cataract-intraocular-lens-implantation-in-cataract-surgery)
- Extracapsular cataract extraction compared with small incision surgery by phacoemulsification: a randomised trial - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc1724033/)
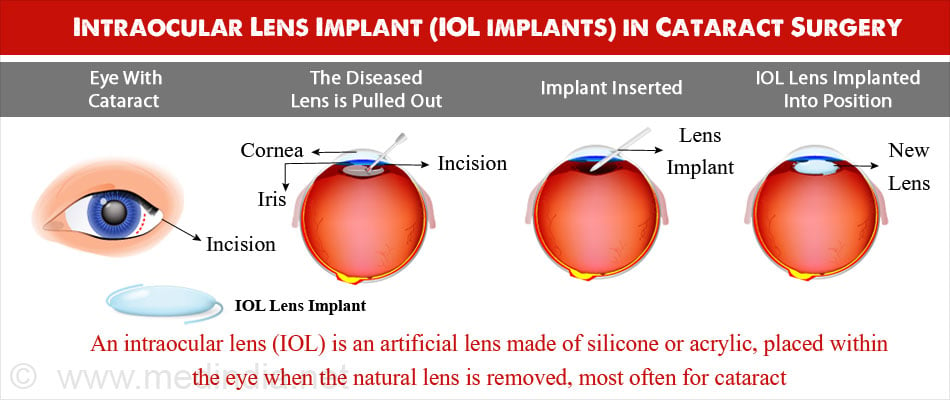
What is Intraocular Lens Implant?
An intraocular lens (IOL) implant is an artificial lens placed within the eye when the natural lens is removed, most often for the treatment of cataract.
It is termed an implant as it is an artificial substitute for the natural lens and takes over its image-focusing function.
What is Cataract?
Cataract refers to the condition when the natural lens of the eye which is normally clear becomes cloudy, most often due to aging. Symptoms due to cataract are blurred vision difficulty in reading and the need for bright light, poor night vision and colors appearing faded.
In the initial stages, cataract might be treated by prescribing different glasses, but as the disease progresses, the vision becomes more blurred necessitating surgery. Surgery is usually undertaken when the blurred vision begins to affect the patient’s lifestyle and daily activities.
History of IOL Implant Surgery
The first IOL implant surgery, with a lens manufactured using polymethylmethacrylate (PMMA), was performed by Sir Harold Ridley in 1949 at St. Thomas’s Hospital London.
Polymethylmethacrylate, also referred to as Perspex or Plexiglas, was chosen by Sir Ridley because he noticed that it stayed inert in the eyes of Royal Air Force pilots, when it entered accidentally from windshields.
PMMA lenses are seldom used nowadays since the material is rigid and cannot be folded. This entails a larger incision to place it within the eye.
With advances in technology, silicone and acrylic have become popular materials for use in intraocular lenses. These are soft and foldable and can be inserted into the eye through a much smaller incision.
What are the Types of Intraocular Lens?
The two types of IOL implants are pseudophakic IOL and the phakic IOL (PIOL) implants.

The pseudophakic lens is the most common type of IOL used, which replaces the natural crystalline lens affected by cataract. The pseudophakic lens then performs the function of the natural lens.
The phakic lens, on the other hand, is placed over the already present natural lens during refractive surgery to correct the optical power of the eye to treat nearsightedness or myopia.
What are the Procedures done for IOL Implant in Cataract?
Insertion of IOL implant is the most common eye surgery procedure. Approximately six million procedures are done annually by eye surgeons.
The two types of procedures done for cataract are phacoemulsification and extracapsular cataract extraction (ECCE). In ECCE, the lens is removed as a whole, but its posterior capsule is left behind. Phacoemulsification (Phako) involves breaking down the natural diseased lens into minute pieces and removing them using suction. It requires a smaller incision as compared to ECCE and has largely superseded ECCE in developed countries. However, since it requires huge capital investment for the surgical and theatre equipment, in developing countries, ECCE is still performed in certain areas with refinements to the traditional technique to treat cataract.
How should I Prepare before the IOL Implant Surgery?
You will have to undergo routine tests as well as tests to assess eye function before the procedure.
Routine Tests
Routine tests which are done before any surgery include:
- Blood tests like hemoglobin levels, blood group and liver and kidney function tests
- Urine test
- Electrocardiogram (ECG) to study the electrical activity of the heart
- Chest x-ray
In older patients, a detailed assessment of the heart may be required. You will be asked to stop medications like aspirin for around a week prior to the surgery.
Eye tests:
You will have to undergo a detailed eye examination to ensure that you need the surgery and you do not have any other illness like glaucoma that could cause complications following the procedure.

What is the Operative Procedure of IOL Implant for Cataract?
IOL implantation for cataract is usually performed as day procedure under local anesthesia. You will be awake during the procedure, but may be administered a sedative to calm down. You can have a light breakfast before coming to the hospital. The procedure will be done while you are lying down on the operating table with the surgeon at the head end. It usually takes up to around 30 minutes.
Described below are the two types of surgical procedures undertaken for IOL implant in the treatment of cataract.
Phacoemulsification
- Before the procedure, eyedrops to dilate the pupil are instilled into the eye.
- Local anesthesia is administered as drops and may also be injected into the tissues around the eye to numb the area.. The area around the eye is cleaned, and the remaining part of the face is draped. The eye is kept open with the help of a lid speculum.
- A tiny cut or incision is made on the transparent tissue in front of the eye (cornea) where it meets the white portion or the sclera.
- Another circular incision is made on the front of the lens covering (capsule).
- A tiny probe that emits ultrasound waves is inserted through the corneal incision to break the lens into fragments.
- The fragments are then liquified and sucked out using another probe.
- After the diseased lens is removed, the IOL is folded and inserted through an injector through the small incision in the cornea.
- Once in place, the implant unfolds and takes the position of the natural lens.
- The incisions heal by themselves without the need for stitches. The eye is covered with a bandage.
Extracapsular Cataract Extraction
- The procedure for extracapsular cataract extraction are similar to phacoemulsification with the following differences.
- A larger incision of 8 to 10 mm is made on the transparent tissue in front of the eye (cornea) where it meets the white portion or the sclera.
- A second incision is made on the front portion of the lens (lens capsule) and the diseased lens is expressed out and removed along with any lens material.
- The IOL is placed within the lens capsule and the incision is closed with stitches.
What is the Recovery Period after IOL Implant Procedure?
- You will be discharged within a few hours of the procedure.
- Usually there is not much pain after the operation. In case there is pain, pain killers such as paracetamol or ibuprofen may be advised.
- You will be given instructions to follow and things to avoid over the next few days. You will be asked to contact the hospital in case of any complications.
- Eye drops will be prescribed to prevent infections and to promote healing.
- You will need to re-visit your doctor either on the same day or the next to remove the bandage. Wearing sunglasses following this will help to prevent the discomfort due to bright lights for a few days. You will also be advised to avoid strenuous activities and avoid washing your hair for a few days following the procedure.
- Further follow-ups will be as directed by the doctor.
What are the Complications of IOL Implantation Surgery?
IOL implantation for cataract is a relatively safe procedure and incidence of complications is infrequent. Most of the incidental complications are easily treated and do not have any long term effect on vision.
Complications may be seen in persons with other chronic underlying conditions such as inflammation of iris and the ciliary body (uveitis), diabetes, or severe shortsightedness.
Complications during surgery
- Tearing of the lens covering (capsule)
- Bleeding within or in front of the eye
- Inability to remove the cataract completely
- Escape of a piece of cataract into the back of the eye
Complications after surgery
- Swelling of the transparent covering of the eye (corneal edema); usually clears by itself
- Swelling and redness of eye

- Detachment of the nerve layer at the back of the eye (retinal detachment)
- Infection within the eye (endophthalmitis)
- Swelling and fluid accumulation in the central retina (cystoid macular edema)
Delayed Complications
- Dislocation of the IOL
- Detachment of the nerve layer at the back of the eye (retinal detachment)
- Increased pressure in eye (glaucoma)
- Glare from bright lights
- Drooping of the upper eyelid (ptosis)
- Opacification of the posterior covering of the lens that remains after the operation (posterior capsular opacification)





