- Necrotising fasciitis. Updated May 23, 2016. Cited July 1, 2018. - (https://www.nhs.uk/conditions/necrotising-fasciitis/)
- Necrotizing fasciitis. Updated July 3, 2017. Cited July 1, 2018 - (https://www.cdc.gov/features/necrotizingfasciitis/index.html)
- Sadasivan J, Maroju NK, Balasubramaniam A. Necrotizing Fasciitis. Indian Journal of Plastic Surgery: Official Publication of the Association of Plastic Surgeons of India. 2013;46(3):472-478. doi:10.4103/0970-0358.121978.
- Wang J, Lim H. Necrotizing fasciitis: eight-year experience and literature review. Braz J Infect Dis. 2014;18(2).
- Taviloglu K, Yanar H. Necrotizing fasciitis: strategies for diagnosis and management. World journal of emergency surgery: WJES. 2007;2:19. doi:10.1186/1749-7922-2-19.
What is Necrotizing Fasciitis?
Necrotizing fasciitis is a rare, highly infectious disease where bacteria infect tissues present below the skin and the coverings of muscles and organs (fascia). Toxins released by the bacteria, cause damage to the soft tissues. Necrotizing fasciitis is also called “flesh-eating disease” because the infected tissues begin to die due to the bacterial toxins, and the condition may become fatal if prompt treatment is not given. Necrotizing fasciitis may be caused by a variety of microbes or a single bacterial organism. Timely diagnosis and treatment prevents the condition from becoming life-threatening.
Classification of Necrotizing Fasciitis
Necrotizing fasciitis is classified based on the infecting microorganism.
Etiological Classification -
- Type 1 – Polymicrobial infection (aerobic and anaerobic bacteria). Occurs mostly in persons with weak immune system
- Type 2 – Group A Streptococcus: can occur in any age group and also affects healthy people
- Type 3 – Gram-negative infection
- Infections with marine organisms (e.g. Vibrio spp. and Aeromonas hydrophilia following contamination of cuts or wounds with seawater)
- Marine infection are particularly serious and can be fatal within 48 hours
- Infection with Clostridium spp following traumatic injuries
- Type 4 – Fungal infection (e.g. candida in persons with weak immunity or zygomycetes infection in injuries caused by trauma)
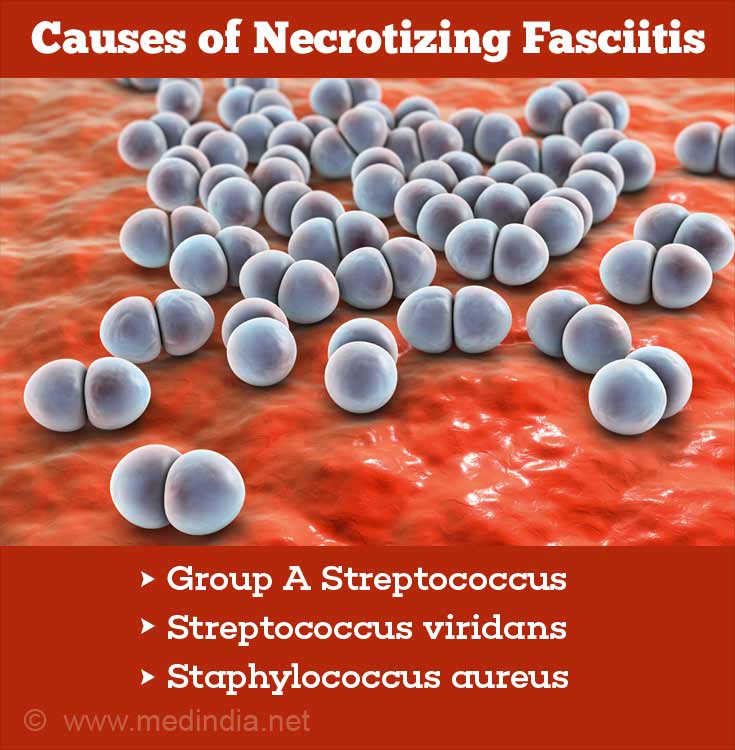
What are the Causes of Necrotizing Fasciitis?
Necrotizing fasciitis is caused mainly by the following organisms. More than one organism may also be identified on culture of the wound:
- Group A Streptococcus – prevalent in most infections
- Streptococcus viridans
- Staphylococcus aureus
Other microorganisms responsible for the infection are:
- Clostridium spp
- Escherichia coli
- Aeromonas hydrophila
- Klebsiella pneumoniae
- Proteus mirabilis
- Pseudomonas aeruginosa
- Vibrio vulnificus
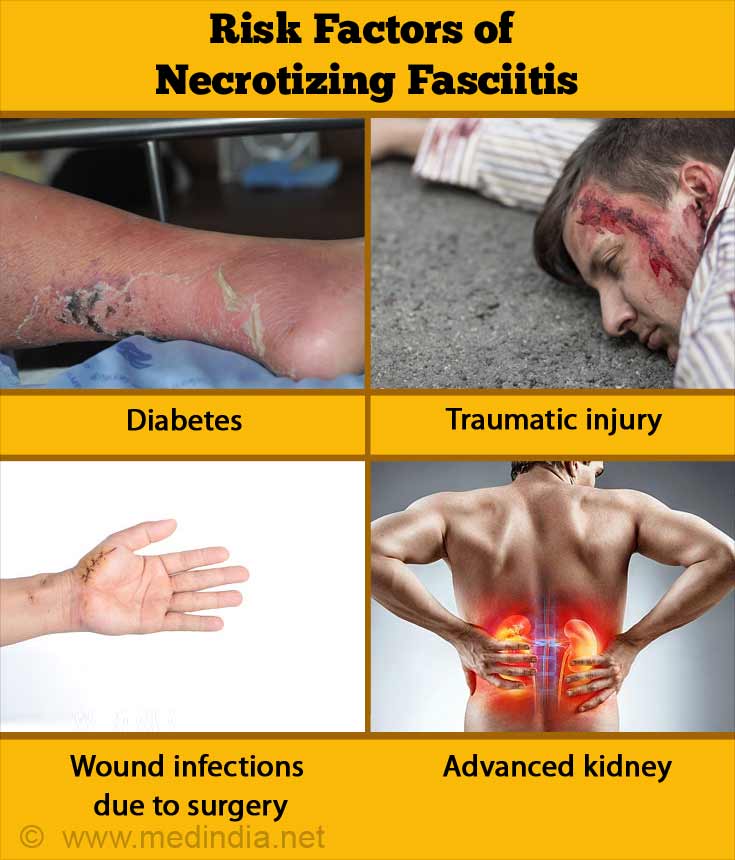
What are the Risk Factors of Necrotizing Fasciitis?
Traumatic injury in otherwise healthy persons or relatively minor injury in persons with a weak immune system can increase risk of necrotizing fasciitis
- Diabetes
- Chronic disease
- Intravenous drug use
- Traumatic injuries
- Insect bites
- Burns
- Persistent ulcers
- Wound infections due to surgery
- Immunodeficiency states eg AIDS, post-transplant patients
- Nonsteroidal drugs
- Alcoholism
- Cancer chemotherapy
- Advanced kidney disease
- Advanced age
- Malnutrition
- Obesity
What are the Symptoms & Signs of Necrotizing Fasciitis?
Necrotizing fasciitis is observed in the extremities, groin, genital areas, and abdomen. In the beginning, the person notices symptoms within a space of a few hours of the injury. Initially, it appears as a skin condition that does not appear to be serious. These initial symptoms which should raise a clinical suspicion include:
- Intense pain disproportionate to the type of injury
- Minor cut or scratch on the skin, which is painful
- Dehydration
- Flu-like symptoms
- Combination of all the above symptoms
- Lack of response to antibiotics (unlike simple cellulitis)
Symptoms that appear later in 2-3 days with fast deterioration of the patient, are:
- Vomiting and loose bowels
- Fever
- Dark skin patches that develop into blisters filled with black-coloured fluid
- Fatigue
- Red or purple swollen patches that are painful and warm to touch
- Chills
- Breakdown of skin near the wound with a flaky, mottled, white, bluish, or dark appearance resulting in gangrene
- Tachycardia – Abnormal heart rate
- Functional deterioration of multiple organs
- Gas within the internal tissues of the skin
- Cracking or grating sounds during movement or feeling the skin (crepitus) due to presence of air in the tissue beneath skin

Critical symptoms manifest within 4 to 5 days
- Septic shock
- Unconsciousness – the body weakens and is unable to fight infection
- Low blood pressure
- Changed mental behavior
- Respiratory failure
In most cases, necrotizing fasciitis develops swiftly but in certain cases, the disease gradually progresses. However, delayed treatment may result in confusion, dizziness, and weakness.
What are the Consequences of Necrotizing Fasciitis?
Necrotizing fasciitis can be lethal if not diagnosed and treated early. In fatal cases, kidney failure, respiratory failure, septic shock, and multiorgan failure cause death.
- Even in non-fatal cases, limb amputation may become necessary to save the patient’s life
How do you Diagnose Necrotizing Fasciitis?
Your family physician will conduct a medical examination based on the symptoms. The success rate for an accurate diagnosis is only 15% - 34%.
A high index of suspicion about the condition is necessary and diagnosis is often missed in the early stages. Most clinicians may not be familiar with the condition
It should be suspected when the patient presents with skin swelling, pain and redness especially if the patient has history of diabetes, alcoholism or chronic kidney disease.
Early referral for surgery is essential if there is any doubt. Investigations can be delayed if they could delay surgical intervention in a patient with suspected necrotizing fasciitis
During surgery, diagnosis is made based on the appearance which include greyish black dead tissue, lack of bleeding, thin ‘dishwater pus#$# unlike usual thick foul smelling pus, lack of resistance when the tissues are probed with the finger and muscle that does not contract in response to stimulus.
What are the Investigations of Necrotizing Fasciitis?
The following tests may help diagnose the presence of necrotizing infection but only surgery offers a definitive diagnosis.
Laboratory tests: The laboratory risk indicator for necrotizing fasciitis score is effective in confirming necrotizing fasciitis. The score is based on the concentration of creatinine, C-reactive protein, hemoglobin, sodium, and glucose as well as the whole blood cell (WBC) count.
Bedside Finger test: In the “finger test”, tissues show lack of resistance to the finger when they are touched. The test is performed under local anesthesia with a 2 cm cut extending to the below to the soft tissue under the skin
Imaging: CT scans, MRI, ultrasonography, and radiography are used to diagnose NF. However, radiography is not quite specific and only helps to identify gas formation within the layers of the skin.
Microbiological tests: Blood culture, and wound swabs will confirm the organism. Fungal culture should be performed in immunodeficient patients.
How can you Treat Necrotizing Fasciitis?
A combination of surgery, antibiotics, and oxygenation of infected regions is used to treat NF. It is important to diagnose and treat NF as soon as possible to avoid the condition from turning fatal.
- Surgical debridement is a procedure to remove dead tissue that may impair the immunity of the host. This is best performed after clearly marking the area of dead, desensitized tissue. This may be lifesaving for the patient and complete removal of dead tissue with adequate margin of healthy tissue is essential
- Antibiotic treatment – Antibiotics must be begun as soon as possible. It can be monotherapy or multidrug therapy. Initially, the antibiotics are prescribed that are effective against a broad range of bacteria. Once the infecting microorganism is confirmed, the exact antibiotic combinations are used. Initial antibiotic treatment involves either ampicillin/sulbactam, cefazolin-metronidazol, or penicillin-clindamycin-gentamicin.
- Hyperbaric oxygen therapy increases tissue oxygenation in necrotized and healthy tissues. This treatment is given after surgical removal of diseased tissue in Clostridium-infected tissues.
- Individualized pre- and postoperative pain control is conducted with antibiotics or topical agents, such as hydrogen peroxide.
- Nutritional support to compensate for excess protein and fluid loss from the wound. Nasogastric feeding may be needed in some cases
- Intravenous immunoglobulins help to treat type II NF.
Clostridium perfringens infection is treated with penicillin G with or without hyperbaric oxygen therapy.
For K pneumoniae infection, ticarcillin/clavulanate, piperacillin/tazobactam or carbapenems is used in combination with aminoglycosides as treatment.
How is Necrotizing Fasciitis Prevented?
The following precautions help to prevent necrotizing fasciitis:
- Take good care of your skin and avoid unnecessary cuts or scratches
- Make sure sore throat is promptly examined by the doctor
- Prompt medical attention (e.g. broad spectrum antibiotics, medical removal of dead tissue) should be given to fever and wounds
- Adequate nutritional support helps to reduce the mortality rate
- Always wash your hands to avoid the spread of group A Streptococcus during meals, coughing, cooking, and sneezing
- Wounds should be carefully monitored for signs of pain, swelling, or redness







