- About Neuroblastoma - (http://kidshealth.org/en/parents/neuroblastoma.html#)
- General Information About Neuroblastoma - (https://www.cancer.gov/types/neuroblastoma/patient/neuroblastoma-treatment-pdq)
- Pediatric neuroblastoma - (https://www.stjude.org/disease/neuroblastoma.html)
- Does aggressive surgical resection improve survival in advanced stage 3 and 4 neuroblastoma? A systematic review and meta-analysis - (https://www.ncbi.nlm.nih.gov/pubmedhealth/pmh0076211/)
- What Is Neuroblastoma? - (https://www.cancer.org/cancer/neuroblastoma/about/what-is-neuroblastoma.html)
- Neuroblastoma in children - (http://www.macmillan.org.uk/cancerinformation/cancertypes/childrenscancers/typesofchildrenscancers/neuroblastoma.aspx)
What is Neuroblastoma?
Neuroblastoma is a very rare type of childhood cancer that develops in immature nerve cells [neuroblasts] of the sympathetic nervous system. The term “neuro” refers to nerves, while “blastoma” refers to a cancer that affects immature cells. This type of cancer occurs most often in infants and young children. It is rarely found in children older than 10 years.
It develops in nerve tissue outside of the central nervous system. These immature nerve cells normally grow into functioning nerve cells; but in neuroblastoma, they become solid tumors made of cancer cells instead. Most scientists believe that neuroblastoma is an accidental growth that occurs during the development of the sympathetic nervous system.
Understanding our Nervous System and How it Functions
The nervous system is divided into the central nervous system (that consists of the brain and the spinal cord) and the peripheral nervous system. Nerves emanate from the latter, fan out and cover the entire body like cables. These nerves transmit information to and fro to all parts of the body.
The peripheral nervous system is further divided into –
Somatic nervous system that consists of voluntary nerves; as the name indicates it is associated with voluntary control of body movements through muscles of the upper and lower limbs and other areas.
Autonomic Nervous System (ANS) that consists of involuntary nerves; this division controls the functioning of all our internal organs (like the heart rate, breathing and digestion) that occur below the level of our consciousness.
The Autonomic Nervous System can be further subdivided into the parasympathetic nervous system (PSNS) and the sympathetic nervous system (SNS).
The sympathetic nervous system is often considered the ‘fight or flight’ system and has evolved over time to protect the body from dangers. By contrast, the parasympathetic nervous system is often considered the "rest and digest" or "feed and breed" system and works as an inhibitory or dampening system to counter the drive of the sympathetic nervous system.
Understanding Tumors of the Autonomic Nervous System
There are three tumors that arise from this system. These are collectively called neuroblastic tumors and named -
- Neuroblastoma
- Ganglioneuroblastoma
- Ganglioneuroma
They all arise from immature or primitive nerve tissue calledsympathogonia and commonly manifest in the -
- Neck
- In the chest behind the heart (Posterior mediastinum)
- Adrenal gland (the small triangular glands on top of the kidneys)
- Behind the abdominal organs (retroperitoneum)
- Pelvis
The three tumors differ in their degree of cellular and extracellular maturation of the nerve cells.
Immature tumor cells are more aggressive and malignant and generally occur in younger age group of patients (median age, just under 2 years). Mature tumor cells occur in older children (median age, approximately 7 years) and tend to behave in a benign fashion.
The most benign neuroblastic tumor is the ganglioneuroma and iscomposed of gangliocytes and mature stroma. Ganglioneuroblastoma has intermediate malignant potential as it is composed of both mature gangliocytes and immature neuroblasts. Neuroblastoma on the other hand is the most immature, undifferentiated, and malignant tumor of the three.
Neuroblastoma most commonly starts in the adrenal glands (the small triangular glands on top of the kidneys), but can also begin from neural tissue that runs along the spinal cord in the neck, chest, abdomen or pelvis. Interestingly, neuroblastoma can alsohave a relatively benign course, even when they have a tendency to spread and become metastatic.
The biologic behaviour of these neuroblastic tumors determines their prognosis to treatment and it varies widely and depends on their DNA content, chromosomal changes, and expression of certain master genes and catecholamine synthesis. It is these elements that divide neuroblastoma into high, intermediate, or low risk categories.
When they are cancerous, neuroblastoma can spread to different parts of the body such as the lymph nodes, bones, skin, and liver. Unfortunately, in about 70% of cases, the cancer has already spread to other parts of the body by the time it is diagnosed. Today, even with the use of high-dose therapy or stem cell transplant therapy more than half of the children cannot be cured.
Neuroblastoma may sometimes be caused by a gene mutation passed from the parent to the child. In such cases the cancer occurs at a younger age and there is a higher probability of multiple tumors forming in the adrenal glands.
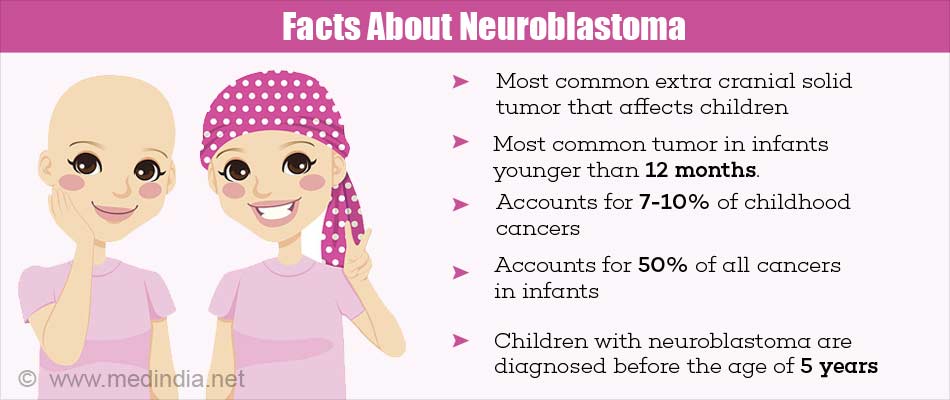
Key Facts about Neuroblastoma
- Neuroblastoma is not a brain tumor.
- Neuroblastoma is the most common extra cranial solid tumor that affects children.
- Neuroblastoma accounts for 7 to10 percent of childhood cancers.
- Neuroblastoma accounts for 50 percent of all cancers in infants, making it the most common tumor in infants younger than 12 months.
- The occurrence of neuroblastoma is the same worldwide (7-10 children / million).
- The occurrence of neuroblastoma in different locations is: adrenal glands (60-65%), abdomen (30%), neck (1%), chest (19%), and pelvis (1%).
- Most children with neuroblastoma are diagnosed before the age of 5 years.
- It occurs slightly more often in boys than in girls.
- Despite advances in therapy, about half of the children with aggressive neuroblastoma succumb to the disease.
What Causes Neuroblastoma?
The cause of most neuroblastomas (98-99%) is not known. Neuroblastomas develop when normal fetal neuroblasts fail to become mature nerve cells. Instead, they uncontrollably continue to grow and divide.
In 1-2 % cases, neuroblastoma seems to occur because of inherited gene changes in the ALK oncogene and PHOX2B, a gene that normally helps nerve cells mature.
Also, as of today there are no known lifestyle related or environmental causes of neuroblastomas. Hence no preventive action can be taken to prevent these cancers.
What are the Different Stages of Neuroblastoma?
Neuroblastoma is categorized into different stages based on the location and how far it has spread. A staging system is a standard way for the cancer care team to sum up the extent of the cancer. The stage of the neuroblastoma along with the age of the child and results of other tests will help in deciding the course of treatment.
Imaging tests are performed to stage the tumor and these include x-rays, CT, MRI scans, and bone scans.
Since the 1990s, the International Neuroblastoma Staging System (INSS) is used to stage a neuroblastoma.
- Stage 1: The cancer is still in the same area where it started. The visible tumor can be removed completely by surgery.
- Stage 2A: The cancer is still in the same area where it started and on one side of the body, but the entire tumor cannot be removed by surgery.
- Stage 2B: The cancer is on one side of the body; however, cancer cells are found in lymph nodes near the tumor.
- Stage 3: This is considered an advanced stage and cannot be entirely removed by surgery. The tumor may have reached a large size; nearby lymph nodes may or may not be involved. The cancer, however, has not spread to distant sites.
- Stage 4: The cancer cells have spread to distant parts of the body such as bone, liver, skin, distant lymph nodes, or other organs. It is divided into stages 4 and 4S.
Stage 4S: This is known as “special” neuroblastoma” as this stage of cancer does not fit into the other stages defined above. In this case the child is younger than 12 months, the cancer is on one side of the body, the neuroblastoma has spread to the liver, skin, or the bone marrow, only 10% of marrow cells are cancerous, and imaging tests do not show that the cancer has spread to the bones or the bone marrow.
Recently the International Neuroblastoma Risk Group Staging System (INRGSS) has been introduced. The INRGSS uses image-defined risk factors (IDRFs) seen on imaging tests.
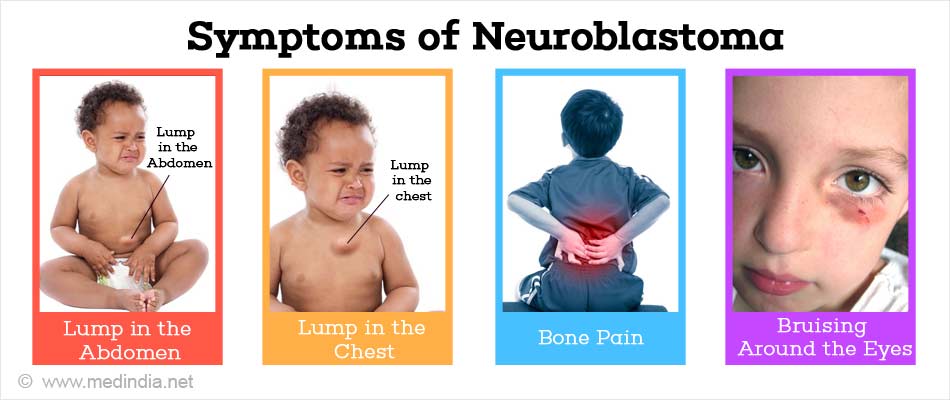
What are the Symptoms of Neuroblastoma?
About 75-80% of tumors have already spread to other parts of the body by the time they are diagnosed. Signs and symptoms of neuroblastoma vary depending on what part of the body is affected and the result of excess hormones secreted by the tumor (Paraneoplastic Syndrome).As many symptoms are similar to those of other common childhood diseases, many children aren’t diagnosed with neuroblastoma until after the cancer has already metastasized to other parts of the body.
- Lump in the abdomen is one of the most common signs of a neuroblastoma. It is usually painless and may cause loss of appetite resulting in weight loss. If it presses against the lymph vessels in the abdomen or pelvis it can cause swelling in the legs and the scrotum. In some cases the pressure from a growing tumor can affect the child’s bladder or bowel causing problems in urinating and changes in bowel habits.
- Lump in the neck or chest is felt as a hard, painless lump. If the tumor is in the chest, it might press on the superior vena cava (the large vein in the chest that returns blood from the head and neck to the heart) causing swelling in the face, neck, arms, and upper chest, headaches, dizziness, and unconsciousness. Pressure on the windpipe can cause coughing, breathing and swallowing difficulties.
- Bone pain may cause the child to limp or refusal to walk. If neuroblastoma spreads to the spine, the pressure on the spinal cord can cause weakness, numbness, or paralysis in the arms or legs.
- Opsoclonus myoclonus ataxia syndrome (dancing eyes, dancing feet) is characterized by an unsteady, trembling gait, myoclonus (brief, shock-like muscle spasms), and opsoclonus (irregular, rapid eye movements).
- Bruising around the eyes, dark circles under the eyes or bulging eyes if the cancer has spread to the bones around the eyes.
- Drooping eyelid due to pressure on certain nerves in the neck (Horner’s Syndrome).
- Frequent infections, excess bruising or bleeding from small cuts or scrapes, tiredness, irritability, and weakness if the cancer spreads to the bone marrow and causes shortages of blood cells.
- Painless, bluish swellings beneath the skin resembling blueberries. This occurs only during the first few months of life and indicates liver involvement.
How do you Diagnose Neuroblastoma?
- Medical history and physical exam - to rule out other health problems such as common infections in childhood or knowing whether there is any family history of cancer. If the history and exam raise a suspicion that a child might have a neuroblastoma other tests are done to confirm the diagnosis.
- Neurological examination - to check the brain, spinal cord, and nerve function. The examination is done to check a child’s ability to walk normally, the muscle tone, sensation, reflexes, mental status and coordination.
- Urine and blood tests - to detect the levels of hormones called catecholamines in blood and urine. Sympathetic nerve cells normally release hormones called catecholamines, such as epinephrine and norepinephrine, which enter the blood. These are then broken into metabolites which pass out of the body in the urine. Neuroblastoma cells also make these hormones which can be detected by blood or urine tests.The2 catecholamine metabolitesmost often measured areHomovanillic acid (HVA) and Vanillylmandelic acid (VMA).
- Additional blood tests - to check cell counts, liver and kidney function.
Various imaging tests are done to determine the location and extent of tumor, involvement of distant sites and to stage the disease and plan treatment.
- Ultrasound - to create pictures of organs or masses inside the body. Occasionally, neuroblastoma may be detected by ultrasound before birth.
- X-ray - may be performed as an early test if the symptoms are not clear and neuroblastoma diagnosis is doubtful.
- Computed tomography (CT) scan -is done to look for neuroblastoma in the abdomen, pelvis, and chest. A CT scan creates detailed images of the soft tissues in the body. CT scans can also be used to guide a biopsy needle into a tumor.
- Magnetic resonance imaging (MRI) scan- MRI scans provide detailed images of soft tissues in the body. These scans are very helpful in looking at the brain and spinal cord.
- MIBG scan - This scan uses meta-iodobenzylguanidine (MIBG) that contains a small amount of radioactive iodine. MIBG is similar to norepinephrine, a hormone made by sympathetic nerve cells. It is injected into a vein and it attaches to neuroblastoma cells in the body. This helps in knowing the location of neuroblastoma is and whether it has spread to other parts of the body.
- Positron emission tomography (PET) scan- uses a radioactive type of sugar known as FDG which is injected into the blood. Cancer cells in the body absorb large amounts of the radioactive sugar and can be detected.
- Bone scan -uses a small amount of low-level radioactive material (technetium-99) to detect areas of active bone changes or “hot spots” in the skeleton. Other bone diseases such as Paget’s disease (a disease of abnormal bone metabolism), arthritis, and bone infection can also cause the same pattern.
- Biopsy - of the tumor and microscopic examination of tissue is done to confirm the diagnosis.
- Bone marrow aspiration and biopsy - is done to help determine the extent of the disease.
How do you Treat Neuroblastoma?
Biologic and genetic characteristics are used along with classic clinical staging to assign patients to risk groups for planning treatment intensity. The following criteria are used to determine the risk.
- Age of the patient
- Extent of disease spread
- Tumor histology or microscopic appearance
- Tumor biology (genetic features)
The therapies also vary for the different risk categories.
- Low-risk neuroblastoma accounts for 37% of cases and requires only observation without any treatment at all or cured with surgery alone. They have an excellent prognosis with cure rates above 90%.
- Intermediate-risk neuroblastoma accounts for 18% of cases and is treated with surgery and chemotherapy. Prognosis is good with this group too with cure rates of 70 – 90%.
- High-risk neuroblastoma accounts for 45% of cases and may be hard to cure. It is treated with intensive chemotherapy, surgery, radiation therapy, stem cell transplantation, biological-based therapy with 13-cis-retinoic acid and antibody therapy. Cure rates for this group was about 30% for the last two decades; recently it was observed in a clinical trial that this number increased to about 66% two years after stem cell transplant in patients who received antibody with GM-CSF and IL-2. In fact these patients were alive and disease-free compared to 46% of the group who did not receive the antibody.
Children with neuroblastoma should have their treatment planned by a team of doctors comprised of the child’s pediatrician and other experts in treating childhood cancer, especially neuroblastoma.
The various treatment regimens include:
- Surgery is the first choice of treatment when the tumor is localized. Much of the tumor can be safely removed depending on the location. If it cannot be removed, a biopsy can be done instead. The role of surgery in advanced staged neuroblastoma is controversial. In tumors that cannot be removed entirely, the residual mass of cells is killed after surgery by chemotherapy or radiation.
- Chemotherapy is when anticancer drugs are used to kill cancer cells. Systemic chemotherapy is when drugs are taken orally or injected into a vein and enter the bloodstream and reach cancer throughout the body. In regional chemotherapy, the drugs inflict cancer cells pertaining to a particular region, like when they are given into the cerebrospinal fluid, an organ, or a body cavity like the abdomen.
Combination therapy that uses two or more anticancer drugs is found to be effective.
- Alkylating agents like Cyclophosphamide or Ifosfamide
- Platinum compounds like Cisplatin or Carboplatin
- Vinca alkaloids like Vincristine
- Anthracycline antibiotics like Doxorubicin
- Topoisomerase 2 inhibitor like Etoposide
- Topisomerase 1 inhibitor like Topotecan and Irinotecan
- Busulfan and Melphalan (sometimes used during stem cell transplant)
The most common combination of drugs includes carboplatin (or cisplatin), cyclophosphamide, doxorubicin, and etoposide, although others may be used. For children in the high-risk group, combinations are usually larger in size and higher in dose, which may be followed by a stem cell transplant.
- Radiation therapy uses where high energy rays to kill cancer cells. External radiation therapy uses a machine outside the body to send radiation toward the cancer and is used to treat neuroblastoma. Internal radiation therapy uses needles or wires that contain a radioactive substance which are placed directly into or near the cancer.
- Targeted therapy uses drugs or other substances to identify and attack cancer cells without trying to harm normal cells. Two kinds of targeted therapies are
- Tyrosine kinase inhibitors are small-molecule drugs that enter cancer cells to block signals that they need to grow and divide. An example is Crizotinib that is used to treat neuroblastoma that has recurred.
- Antibody-drug conjugates are made up of a monoclonal antibody attached to a drug. The monoclonal antibody binds to specific proteins or receptors found on cancer cells while the drug enters these cells and kills them without harming other cells. Lorvotuzumab mertansine is one such antibody-drug conjugate being studied to treat neuroblastoma that has recurred.
- Iodine-131 mIBG therapy treats the condition with radioactive iodine. The radioactive iodine is given intravenously and carries radiation directly to tumor cells where it collects and kills the cancer cells. Iodine 131-MIBG therapy is sometimes used to treat high-risk neuroblastoma that comes back after initial treatment.
- Stem cell rescue along with high-dose chemotherapy and radiation therapy Stem cells are immature blood cells that can mature into blood cells at a later date. This method removes them from the blood or bone marrow of the patient and freezes and stores them as an initial step. High doses of chemotherapy and radiation therapy are then given to the patient after which, the stored stem cells are thawed and infused back into the patient. These reinfused stem cells grow into healthy blood cells. This therapy is used for high-risk neuroblastomas. Another way of using stem cells are using them as maintenance therapy for 6 months after high-dose chemotherapy and radiation therapy to kill any cancer cells that may recur.
- Isotretinoin or a retinoid called 13-cis-retinoic acid is a vitamin -like drug that is taken orally to slows the cancer's ability to make more cancer cells and changes how these cells look and act. It is used in high-risk patients and given prevents cancer from recurring after treatment with high-dose chemotherapy and stem cell transplant.
- Immunotherapy is when the child’s immune system is stimulated to fight the disease. It is also known as biologic therapy. Substances that are made by the body or synthesized in a laboratory boost, direct or restore the body’s defences against cancer. Vaccines are a kind of immunotherapy that is being studies to treat recurring neuroblastomas.
- Dinutuximab is a type of targeted monoclonal antibody therapy is given by infusion that uses an antibody that identifies and attaches to a substance, called GD2, on the surface of neuroblastoma cells. The cells reciprocate by sending signals to the immune system that dinutuximab is a foreign substance and needs to be killed. Then the body's immune system kills the neuroblastoma cell. Dinutuximab can be given along with cytokines like:
- Granulocyte-macrophage colony-stimulating factor (GM-CSF), a cytokine that helps make more immune system cells, especially granulocytes and macrophages (white blood cells), which can attack and kill cancer cells.
- Interleukin-2 (IL-2), a type of immunotherapy that mainly boosts the growth and activity of lymphocytes (a type of white blood cell) that can attack and kill cancer cells.
Many of the standard treatments for cancer today are based on earlier clinical trials. If feasible, patients may want to think about taking part in a clinical trial as it might offer them the best treatment choice.
Children who are treated for neuroblastoma may have an increased risk of late effects like physical, psychological or second cancers that can sometimes be treated or controlled.
Follow-up tests or check-ups are repeat diagnostic tests to find out cancer staging, and are done either during treatment to find if it is working well and whether to continue or change it or taken post treatment to note the benefits of treatment.
How do you Prevent Neuroblastoma
As the definitive causes of neuroblastoma are still unknown it is not possible to prevent it.