- HIV and Opportunistic Infections, Coinfections, and Conditions - (https://aidsinfo.nih.gov/understanding-hiv-aids/fact-sheets/26/86/what-is-an-opportunistic-infection-)
- Learn More About Opportunistic Infections - (http://www.thewellproject.org/hiv-information/what-are-opportunistic-infections)
- AIDS - Signs and Symptoms - (https://www.ucsfhealth.org/conditions/aids/signs_and_symptoms.html)
- Opportunistic Infections - (https://www.cdc.gov/hiv/basics/livingwithhiv/opportunisticinfections.html)
What is an Opportunistic Infection (OI)?
Our body is constantly being exposed to numerous pathogens like bacteria, virus, fungi and protozoa. However, the immune system in our body prevents the pathogens from invading and causing illness. But when the immunity is weakened due to various causes such as HIV infection, during cancer chemotherapy or administration of immunosuppressive drugs post-transplant to prevent graft rejection, these organisms avail the opportunity to invade and to cause severe illness.
Opportunistic infections cause severe illness and more often among the immunocompromised than healthy people.
During the early period of the emergence of HIV, opportunistic infections were more frequent. But since the anti-retroviral therapy, the cases and deaths due to opportunistic infections have decreased. Nevertheless opportunistic infections are still encountered often, because many people with HIV are unaware of their condition. Sometimes diagnosis of an opportunistic infection would lead to testing for HIV and diagnosing the condition.
What are the types of Opportunistic Infections?
There are many types of OIs that are seen in HIV patients that can be caused by bacteria, fungi, viruses and protozoan organisms. The common infections and causative organisms are:

| Site of Infection | Clinical features | Causative organism |
| Lung | Pneumonia Tuberculosis | Pneumocystis jiroveci, cytomegalovirus Mycobacterium tuberculosis |
| Mouth | ThrushHairy leukoplakiaMouth ulcers | Candida albicans Epstein Barr virus Herpes simplex virus 1 (HSV-1), Histoplasma capsulatum |
| Esophagus | ThrushEsophagitis | Candida albicans Cytomegalovirus, herpes simplex virus 1 |
| Intestines | Diarrhea | Salmonella spp, Shigella spp, Cryptosporidium, Giardia lamblia, cytomegalovirus |
| Central nervous system | Meningitis Brain abscess Progressive multifocal leukoencephalopathy | Cryptococcus neoformansToxoplasma gondii JC virus |
| Eye | Retinitis | Cytomegalovirus |
| Skin | Kaposi sarcoma Herpes zoster Subcutaneous nodules | Human herpes virus 8 Varicella zoster virus Cryptococcus neoformans |
| Reticuloendothelial system | Lymph node enlargement, Liver and spleen enlargement | Mycobacterium avium complex, Epstein Barr virus |
- Tuberculosis: It is a chronic bacterial infection affecting mainly the lungs. In HIV patients it is the most commonly associated infection and can be very severe and spread to other sites as well.
- Candidiasis: It is a fungal infection caused by Candida. It frequently affects the skin and mucous membranes. In patients with HIV, it frequently causes oral and vaginal candidiasis. However, when it affects the oesophagus, trachea, bronchi or deep lung tissue it is considered as OI.
- Cytomegalovirus (CMV) Infection: It is caused by Cytomegalovirus. It can cause pneumonia, gastroenteritis, retinitis and encephalitis. CMV retinitis is an emergency which can lead to blindness if treatment is delayed. Retinitis due to CMV is mostly due to the immunocompromised state. Patients with HIV have an increased risk of CMV retinitis when the CD4 cell count falls below 100 cells per cu mm of blood. When CD4 count drops below 50 cells per cu mm, the HIV patients are more prone to CMV related diarrhea and abdominal pain.
- Cryptococcosis: It is a fungal infection caused by Cryptococcus neoformans. It infects the lung and brain. Patients with HIV are at an increased risk of Cryptococcal meningitis when the CD4 cell count drops below 100 cells per cu mm.
- Cryptosporidiosis: It is a protozoan infection caused by Cryptosporidium. It causes abdominal cramps and severe and chronic diarrhoea.
- Mycobacterium Avium Complex (MAC): It is caused by Mycobacterium avium, Mycobacterium kansasii or Mycobacterium intracellulare. These organisms normally don’t cause infection. But in immunocompromised patients, they can spread throughout the body and cause a life-threatening infection. Patients with HIV are at increased risk of MAC when the CD4 cell count drops below 50 cells per cu mm.
- Pneumocystis Carinii Pneumonia (PCP): It is a lung infection caused by Pneumocystis carinii (now referred to as pneumocystis jiroveci). It is seen more among the immunocompromised patients. Patients with HIV are at increased risk of PCP pneumonia when the CD4 cell count drops below 200 cells per cu mm.
- Toxoplasmosis: It is a parasitic infection by Toxoplasma gondii. It may cause lesions in the lung, brain and eye. Patients with HIV are at an increased risk of Toxoplasmosis when the CD4 cell count drops below 100 cells per cu mm.
- Herpes simplex virus (HSV) infection: Normally HSV infection does not cause major illness, however in immunocompromised persons, it can cause serious illness affecting the lungs and esophagus.
- Rare infections encountered in HIV infection include progressive multifocal leukoencephalopathy and Kaposi sarcoma
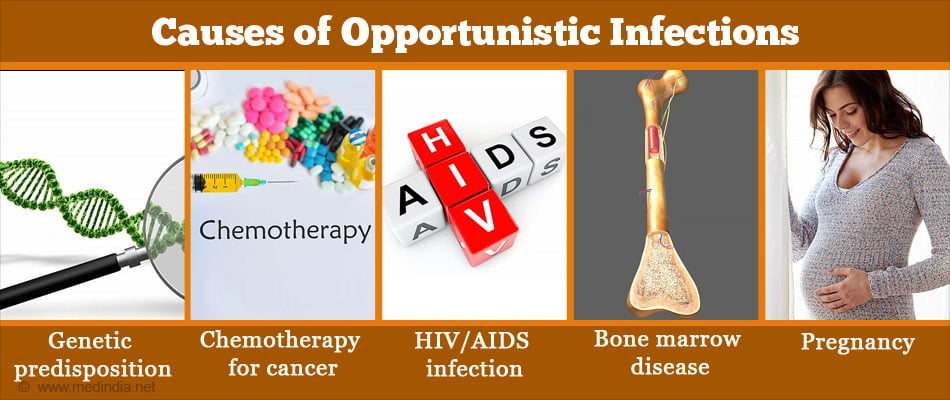
What are the Causes of Opportunistic Infections?
A weakened immune system is the cause of majority of opportunistic infections. The immune system is weakened due to HIV/AIDS, cancer chemotherapy and use of corticosteroids. Some people have defective immunity which is genetic and present since birth. Following are some of the causes of a weakened immune system:
- Genetic predisposition
- Chemotherapy for cancer
- Immunosuppressive drugs given to prevent transplant rejection post-transplant
- HIV/AIDS infection
- Severe malnutrition
- Prolonged antibiotic treatment – disrupts normal bacterial flora present in the body, which normally outnumbers pathogens and prevents them from establishing infection
- Infants and the elderly due to a naturally weak immune system
- Bone marrow disease causing decreases white cell production (neutropenia)
- Skin damage
- Pregnancy
What are the Symptoms and Signs of Opportunistic Infections?
The symptoms due to opportunistic infections in patients with HIV will depend on the organ involved and include:
- Fever
- Productive cough
- Breathlessness
- Painful blisters on skin and over the genital area (cold sores)
- Evidence of candidiasis – oral or vaginal thrush
- Skin infections and rashes
- Unexplained weight loss
- Loss of vision
- Severe headache
- Severe and chronic diarrhea
- Seizures
- Fatigue
- Dysphagia: Difficulty in swallowing
- Odynophagia: Pain while swallowing.
- Confusion

How do you Diagnose Opportunistic Infections?
To diagnose an underlying opportunistic infection, depending on the symptoms of the patient the following investigations may be done to establish the severity of the immunosuppression and to identify the cause of infection. A detailed description of the diagnosis of each infection is beyond the scope of this article. Commonly performed investigations based on clinical suspicion include the following:
- CD4 count: A decrease in the CD4 T-cell count can cause opportunistic infections. Therefore performing a CD4 cell count will be useful in establishing presence of impaired immunity and determining the severity of immunosuppression.
- Chest X-ray: When patients with HIV complain of cough and fever for over 4 weeks, it is necessary to do a chest x-ray. The chest x-ray helps to diagnose opportunistic infections like TB lung and PCP infection.
- Sputum smear: Examination of a stained smear of the sputum microscopically helps to detect TB bacilli, Pneumocystis carinii or other organisms causing opportunistic infections in the lung.
- Serology: Serological tests can detect the presence the microbial antigen or the antibody in the blood or other body fluids. Several tests such as ELISA, agglutination tests and immunofluorescence are widely available in most hospitals and diagnostic laboratories.
- CT/MRI Brain: It is an imaging study. It is recommended for patients with fever, headaches and seizures. It helps to detect lesions caused by Toxoplasma, a causative organism of Toxoplasmosis.
- Indian Ink Preparation of CSF: In patients with Cryptococcal meningitis, CSF fluid on Indian Ink preparation shows the Cryptococcus thus helps to find the causative organism.
- Stool examination: In patients with severe diarrhoea in the background of HIV, stool for ova and cysts may be recommended to look for cryptosporidium cysts and other organisms causing diarrheal illness.
- Microbial Culture of specimens such as sputum and CSF or other body fluids may be done to identify the causative organism
- Ophthalmoscopic examination: It may be required in patients with suspected CMV retinitis.
How do you Treat Opportunistic Infections?
Depending on the infection the patient the treatment varies. But the anti-retroviral therapy should be continued along with the antibiotics for the specific OI in the patient.
- Pneumocystis carinii pneumonia (PCP) Infection: Trimethoprim/Sulfamethoxazole is used both for the prophylaxis and treatment of PCP pneumonia. Dapsone, aerosolized Pentamidine or Atovaquone are also used in some patients.
- Toxoplasmosis: Trimethoprim/sulfadiazine are the antibiotics used for Toxoplasmosis.
- Cryptococcal Meningitis: Amphotericin B plus flucytosine for the initiation and later fluconazole are prescribed.
- Oesophageal candidiasis: Fluconazole an antifungal agent is used.
- Cryptosporidial Infection: Azithromycin and paromomycin for patients with Cryptosporidal infection
- Candidal Infection: Anti-fungal medications like fluconazole, itraconazole are useful in Candidal infection
- Tuberculosis – It is treated with antituberculous drugs such as rifampicin, ethambutol, isoniazid, streptomycin
- Mycobacterium avium intracellulare complex (MAC): antibiotics like Azithromycin, clarithromycin and ethambutol are useful in patients with MAC.
- CMV retinitis: Ganciclovir and foscarnet are antiviral agents for CMV infection.
How do you Prevent Opportunistic Infections?
The following are some preventive measures in HIV patients:

- Take HIV medications regularly.
- Take the suggested vaccines and prophylactic treatment.
- Wear gloves while handling cat faeces.
- Safe sex practice helps to avoid OIs.
- Wash your hands before handling food.
- Don’t consume raw unpasteurized milk, undercooked eggs and use bottled water to drink.
- Avoid sick contacts.
- Get the hospital checks and CD4 counts regularly. Because your health care provider will suggest you some prophylactic antibiotics when CD4 counts fall to prevent from OIs.
- When the CD4 count drops to less than 200 per cu mm of blood, to prevent PCP pneumonia antibiotics are given. Sulfamethoxazole and Trimethoprim are given.
- When the CD4 count drops to less than 100 per cu mm, Sulfamethoxazole and Trimethoprim are given to prevent Toxoplasma gondii
- When the CD4 count drops to less than 50 per cu mm, Azitromycin an antibiotic is recommended to prevent MAC.
- Good food, sleep, exercise and stress-free life as always are essential.
- In cases where immunosuppressive treatment is being given, the doses of these agents may have to be modified to reduce the risk of infections.