- Oropharyngeal Cancer Treatment - (https://www.cancer.gov/types/head-and-neck/patient/adult/oropharyngeal-treatment-pdq)
- Oral cancer: causes and symptoms - (https://www.nidcr.nih.gov/sites/default/files/2017-10/oral-cancer-causes-symptoms.pdf)
- Oropharyngeal Cancer Epidemic and Human Papillomavirus - (http://sbccp.org.br/arquivos/HN2015-07/hed.23697.pdf)
- HPV and oropharyngeal cancer - (https://www.cdc.gov/cancer/hpv/basic_info/hpv_oropharyngeal.htm)
- Current understanding of Oropharyngeal cancer and its management - (https://pdfs.semanticscholar.org/b06c/2f683dfd159d7493e71f5fbdf50149b17177.pdf)
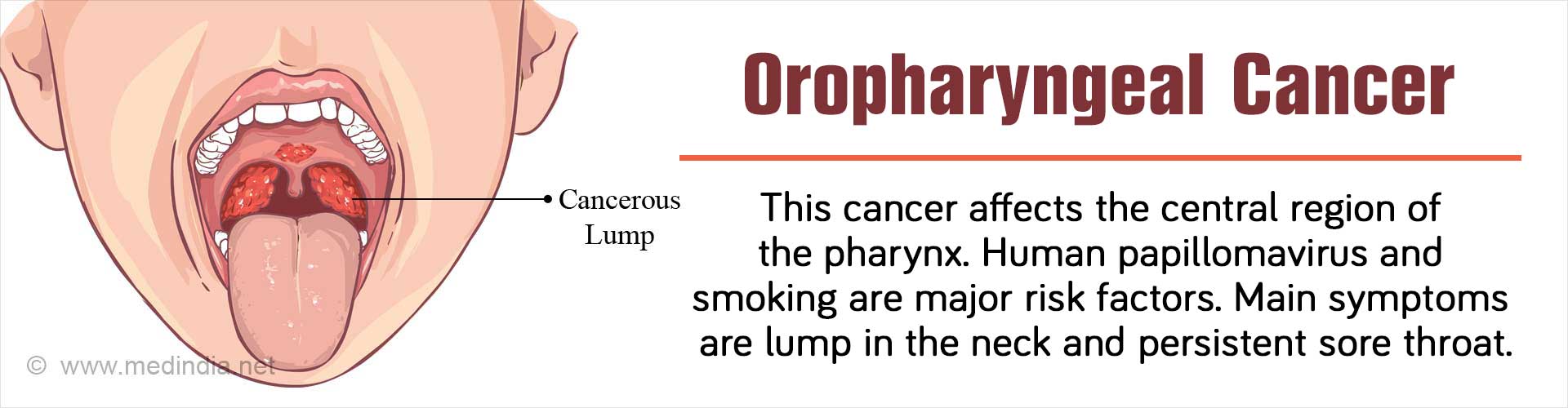
What is Oropharyngeal Cancer?
Oropharyngeal cancer affects the oropharynx or the central region of the throat (pharynx) located at the posterior of the mouth and the oral cavity. Being a malignant condition, the cells may undergo drastic changes and begin to spread to other parts of the body. Men are more often affected by oropharyngeal cancer compared with women.
Oropharyngeal squamous cell cancer (OSCC) is a type of head and neck cancer – a commonly observed cancer in India and South America, and to a lower degree in Europe and the United States. The overall 5-year survival rate is only about 25% for those suffering from OSCC. The most common types of OSCC are tongue and tonsillar cancers, which comprise 90% of OSCC. There is a steady increase in the number of OSCC cases induced by the Human papillomavirus (HPV).
Oropharyngeal cancer occurs in different parts of the oral cavity:
- Soft palate
- Posterior pharyngeal wall – Rare and diagnosed late
- Tonsillar complex
- Base of tongue
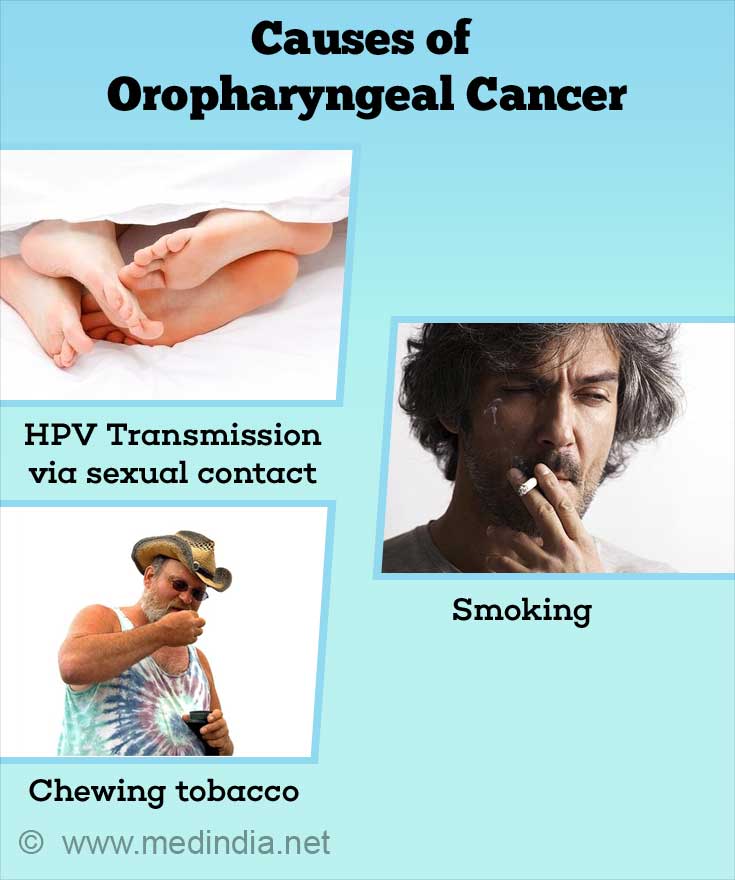
What are the Causes of Oropharyngeal Cancer?
There are many common risk factors that increase the chances of developing OSCC, such as:
- Family history of head and neck cancer
- Alcohol consumption
- Diet
- Human papillomavirus infection (specifically HPV type 16)
- Exposure to the sun
- Smoking (> 10 pack years)
- Chewing betel leaves
- Age (> 40 years)
- Malnutrition
Increasing evidence indicates that younger individuals (< 40) are now diagnosed with OSCC in Europe and the USA.
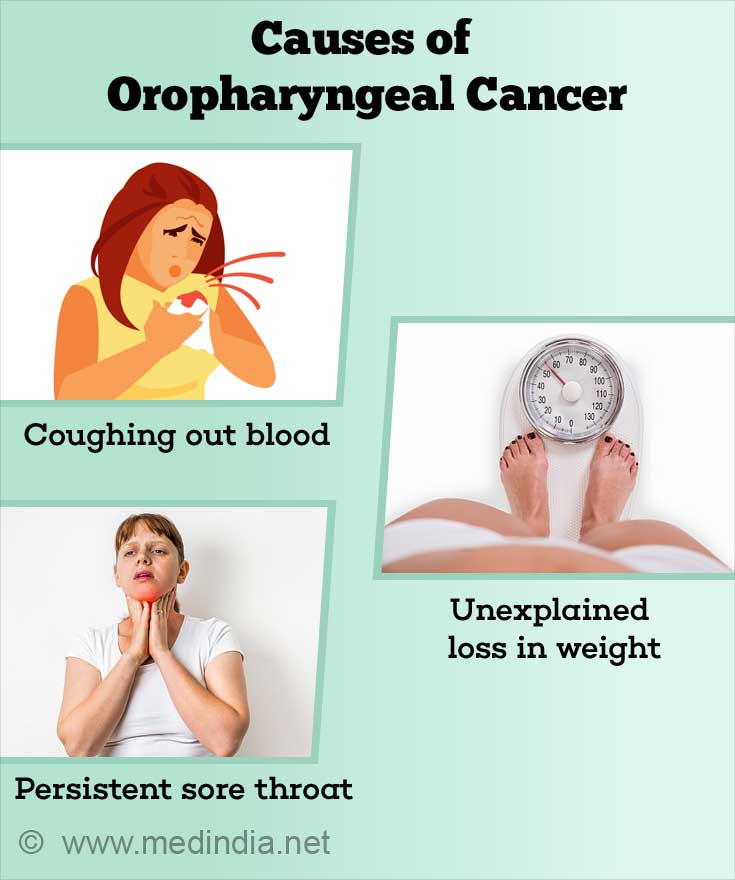
What are the Symptoms and Signs of Oropharyngeal Cancer?
The signs and symptoms of OSCC are not noticeable at the onset of the disease. Some symptoms may be associated with other conditions. It is best to consult your physician. The pertinent signs and symptoms of OSCC are listed below:
- Coughing out blood
- Presence of a lump or irritation in the recesses of the throat, neck, or mouth.
- Unexplained loss in weight
- Persistent sore throat – A common symptom of tongue base cancer
- Difficulty in swallowing
- Pain in the ears, which does not affect hearing
- Presence of a dull ache at the back of the breastbone
- Difficulty in moving the tongue or completely keeping the mouth open
- Lining of the mouth or the tongue has a persistent white patch
- Numbness in the oral cavity or tongue
How do you Diagnose Oropharyngeal Cancer?
In order to diagnose OSCC, the family doctor should take a complete medical examination and physical history of the patient. The doctor will look for lumps or swelling in the floor and roof of the mouth and in the neck. Your jaw will be checked for issues with movement. Ears and eyes will be checked. The doctor will also ask about your daily habits, including tobacco or alcohol use. You will also be asked about prior illnesses and family history of cancer. Following the initial examination, diagnostic procedures help to provide a clear picture of the condition.
Toluidine Blue: This dye is applied topically to identify premalignant (precancerous) lesions, such as lichen planus, leukoplakia, mixed red and white lesions, erythroplakia, and verrucous lesions.
Panendoscopy: Following a medical examination, your oropharynx and mouth will be examined with an endoscope. Panendoscopy is a combination of esophagoscopy (esophagus), laryngoscopy (larynx), and bronchoscopy (lung bronchii). Tissue samples are taken for further biopsy. Your doctor will look for other tumors that may coexist. You will be given a general anesthetic before the procedure, and you will be asked to avoid talking to give rest to your throat. You will not be able to consume food or drinks for one hour following panendoscopy.
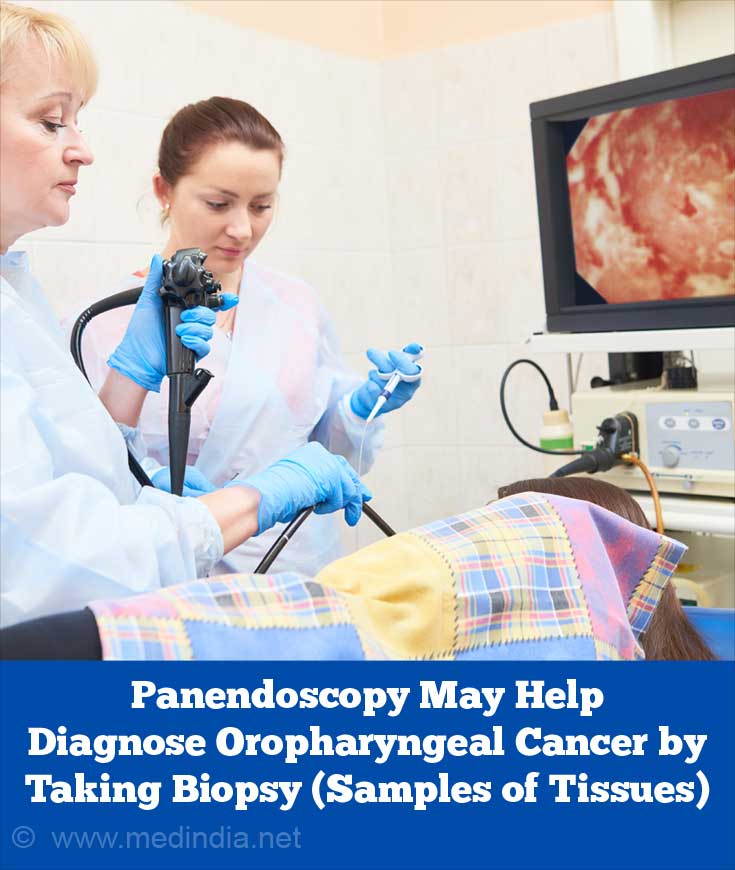
Biopsy:
Tumor tissue samples are collected for further analysis in different ways, such as:
- Punch biopsy: A special instrument is used to collect the tumor sample and some normal tissue along with it.
- Incisional biopsy: A small cut in the mucus membrane of the pharynx or the skin of the throat is made to collect a small portion of the tumor sample.
- Fine needle aspirate: A needle with a syringe is used to collect cells and fluid from the lymph nodes or a diagnosed lump in the neck.
- Excisional biopsy: The entire tumor along with some surrounding normal tissue is removed by making a cut in the pharynx.
- Endoscopic biopsy: The biopsy is performed during endoscopy.
MRI: Magnetic resonance imaging provides high quality images of the bone marrow and the soft tissues (e.g. tongue base) to identify the stage of cancer progression or if the cancer has relapsed. benign, metastatic, and inflammatory lesions can be clearly distinguished in MRI images that are superior to those obtained by computed tomography. However, MRI images are extremely sensitive slight movements that affect the image quality. With high costs and an extended time to acquire the image, the patient is put to a lot of inconvenience.
Computed Tomography: CT scans are often used to detect the presence, development, and the spread of cancer. The captured 3-D images of the internal tissues, blood vessels, and bones help the doctor to decide the treatment strategy. One can also determine the efficacy of treatment or the recurrence of a tumor with the help of CT images.
Positron Emission Tomography (PET) scans: These 3-D colour images of the lymph nodes and neck region provide details on the growth and spread of the cancer.
PET-CT scan: A combined image using both the techniques provides a complete picture of the localization and nature of the tumor as well as the extent of metastasis.
Laboratory tests: The OSCC tissue should be tested for HPV infection.
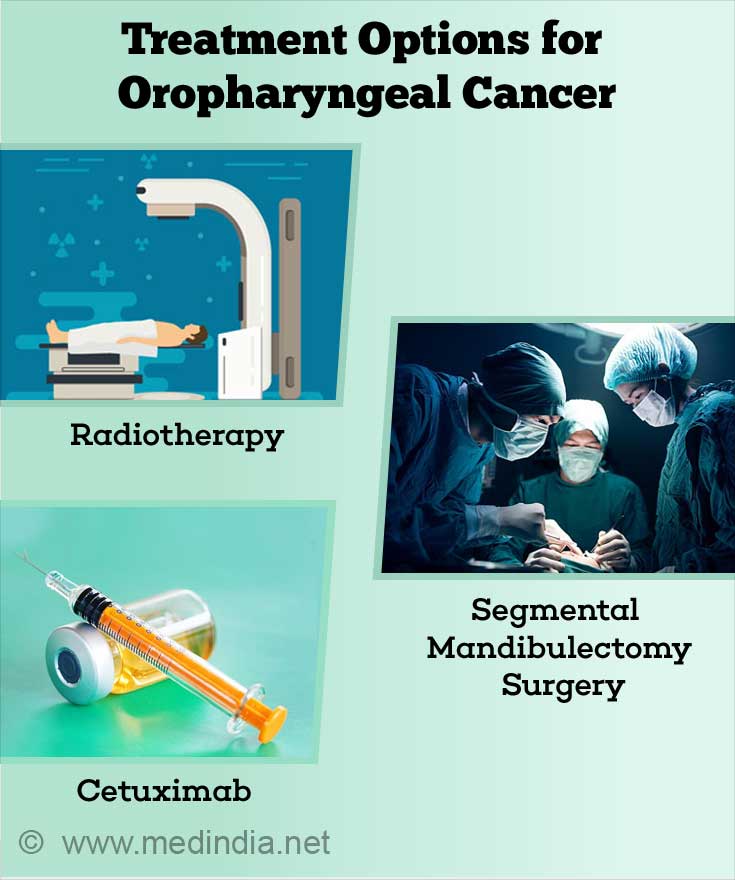
What are Treatment Options for Oropharyngeal Cancer?
Oropharyngeal cancer is classified, using the tumor-node-metastasis (TNM) staging, into different stages based on how much the disease has progressed. The 5-year survival rate for stage I is 56% and this progressively reduces to 43% for OSCC. The survival rate appears to be better if the tumors are HPV-positive. Irrespective of the treatment choice or the stage, HPV-positive oropharyngeal tumors show a positive 5-year survival rate and lower chances of relapse. Stage I and II OSCC are treated with either radiotherapy or surgery whereas advanced stage tumors are treated with combination therapies, such as chemoradiotherapy or surgery and postradiotherapy.
Radiotherapy: This procedure uses radiation or high-energy x-rays to target and kill cancer cells. In OSCC, treatment is performed with external radiotherapy. This form of treatment is used for small posterior pharyngeal wall tumors with no nodes and tongue base tumors.
- External radiation therapy uses a machine to send radiations to the affected area in the body.
- Stereotactic external-beam radiation therapy uses a number of equipment to maintain the exact position of your body when delivering the radiation. You are subjected to radiation once every day for many days. Maintaining the exact position will eliminate unnecessary radiation of surrounding areas and maintains reproducibility in data.
- Hyperfractionated radiation therapy breaks down the radiation dose into multiple small doses to treat advanced oropharyngeal cancer effectively.
- Intensity-modulated radiation therapy (IMRT) uses different intensity radiations to target the tumor from different angles and create 3-D images. The images give a clear picture of the shape and size of tumors.
Surgery: In early stages, surgery is one of the treatment options. In the advanced stages, a combination therapy may involve surgery as one of the treatment choices. A few examples are:
Segmental mandibulectomy: This surgical procedure is used in those people who suffer from bone invasion into the soft tissues of the oral cavity.
Transoral robotic surgery (TORS) is a minimally invasive surgery. The robotic camera provides a picture of the internal region of the oral cavity. With the help of these images, the surgeon is able to attach tools to the robotic arm and direct it to excise tumors in areas that are hard to reach. This procedure helps to avoid the use of other surgical procedures as well as postoperative radiotherapy or combined chemoradiotherapy.
Chemoradiotherapy: Advanced stages of tongue base tumors are treated with chemoradiotherapy to improve the effectiveness of subsequent surgery. Swallowing is greatly improved with chemoradiotherapy irrespective of the tumor stage or complication.
Targeted therapy: Monoclonal antibodies (medications), such as Cetuximab (Erbitux), target a specific protein on the cancer cell and prevent the cell from dividing and growing. Nivolumab is another drug that is currently under research, to target stage III and IV OSCC.
Chemotherapy: Oropharyngeal cancer is treated with systemic chemotherapy where chemotherapeutic drugs (e.g. Cisplatin – Platinol AQ) are given orally or injected into the bloodstream or the muscle.
What are the Complications of Oropharyngeal Cancer?
Complications observed post surgery in OSCC are due to the effects of radiation, surgery, or chemotherapy and are listed below:
- Reduced thyroid function
- Bone death (Osteoradionecrosis)
- Problems with hearing
- Issues with chewing
- Soreness and dryness of the mouth
- Reduced sex drive
- Decreased self esteem
- Changes in taste: leads to poor nutrition
- Problem moving the jaws
How can we Prevent of Oropharyngeal Cancer?
Following a proper diet and avoiding alcohol or tobacco could help to avoid the development of OSCC.
A large number of oropharyngeal cases are caused by HPV. Regular use of dental dams and condoms could help reduce the rate of HPV-associated oropharyngeal cancer.