- Treatments and drugs - (http://www.mayoclinic.org/diseases-conditions/peritonitis/basics/treatment/con-20032165)
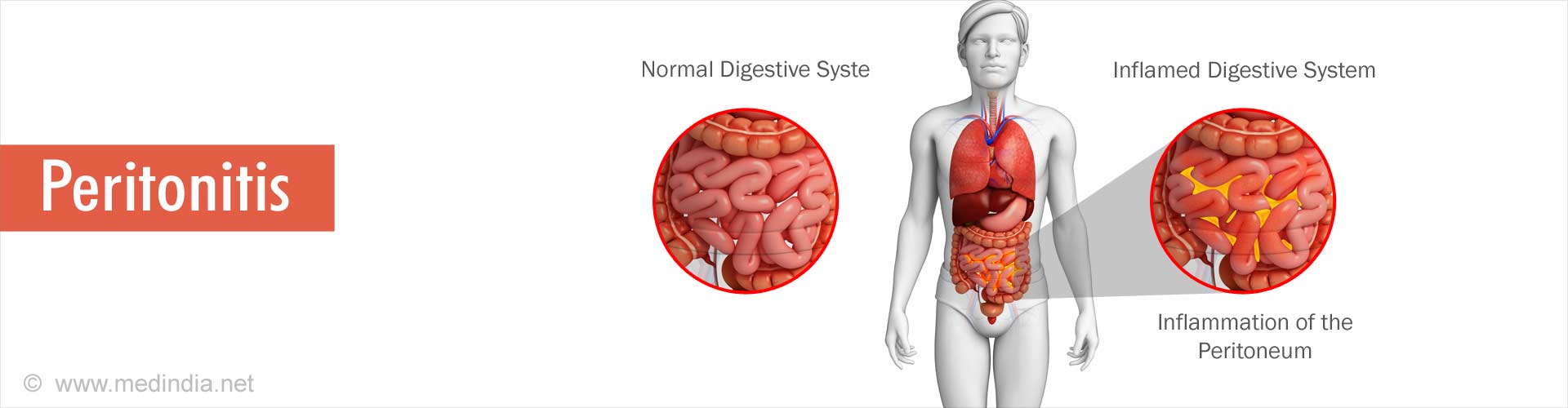
What is Peritonitis?
Peritonitis is the inflammation of the peritoneum, a silk-like membrane that lines the inner abdominal wall and covers the organs within the abdomen.
It is primarily caused due to bacterial or fungal infections that result from any perforation in the abdomen.
What are the Types of Peritonitis?
There are two major types of peritonitis, namely
- Primary peritonitis
- Secondary peritonitis
The former occurs when the infection spreads from the blood and lymph nodes to the peritoneum, which occurs rarely in less than 1% of all cases. The latter occurs when the infection comes into the peritoneum through a perforation in the abdominal wall.
Peritonitis in children is found to have a high mortality rate (78%). Though neonatal peritonitis might be bacterial or chemical in origin, the majority of bacterial peritonitis cases are due to intestinal perforations, ruptured omphaloceles, or ischemic intestinal necrosis.
The latter type of peritonitis is due to prenatal intestinal perforation with extrusion of sterile meconium into the peritoneal cavity.
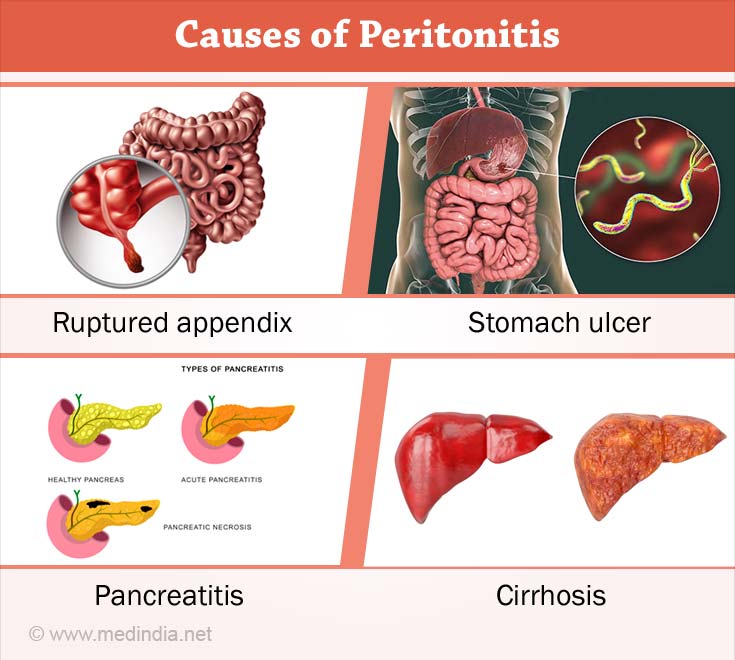
What are the Causes of Peritonitis?
Infection of the peritoneum happens due to various reasons. Some of the common causes are as follows:
- Peritoneal dialysis uses catheters that might cause infection due to unclean surroundings, poor hygiene, or contaminated equipment.
- Peritonitis also develops as a complication of gastrointestinal surgery, the use of feeding tubes, or paracentesis, and as a complication of endoscopy or colonoscopy.
- A ruptured appendix, stomach ulcer, or perforated colon allows bacteria to get into the peritoneum.
- Pancreatitis complicated by an infection might spread into the peritoneum.
- Rupture of diverticulitis causing spillage of intestinal waste into the abdominal cavity.
- Trauma can pave the way for entry of bacteria or chemicals from other parts of the body into the peritoneum.
Thus, it is evident that most cases occur due to a rupture in the abdominal wall.
- However, spontaneous peritonitis may develop without any abdominal rupture as a complication of cirrhosis. Advanced cirrhosis leads to build-up of large amount of fluid in the abdominal cavity (ascites) that is susceptible to bacterial infection.
What are the Symptoms and Signs of Peritonitis?
The symptoms of peritonitis are as follows:
- Abdominal pain or tenderness
- Fever
- Nausea and vomiting
- Fatigue
- Thirst
- Loss of appetite
- Diarrhea
- Low urine output
- Inability to pass stool or gas
- Bloating or a feeling of fullness in the abdomen

If peritoneal dialysis is being performed, then peritonitis symptoms include:
- Cloudy dialysis fluid
- White flecks or strands of fibrin in the dialysis fluid
What are the Complications of Peritonitis?
Complications from peritonitis can be serious and life threatening, and occur if infection extends beyond the peritoneum. They include:
- Bloodstream infection, namely bacteremia.
- Infection throughout the body, namely sepsis.
- Hepatic encephalopathy (occurrence of confusion, altered level of consciousness and coma as a result of liver failure)
- Hepatorenal syndrome, which is progressive kidney failure.
- Intra-abdominal abscess, which is a collection of pus gangrenous bowel.
- Intraperitoneal adhesions caused by bands of fibrous tissue leading to bowel blockage.
If peritonitis is suspected, immediate hospitalization and treatment are necessary to prevent complications.
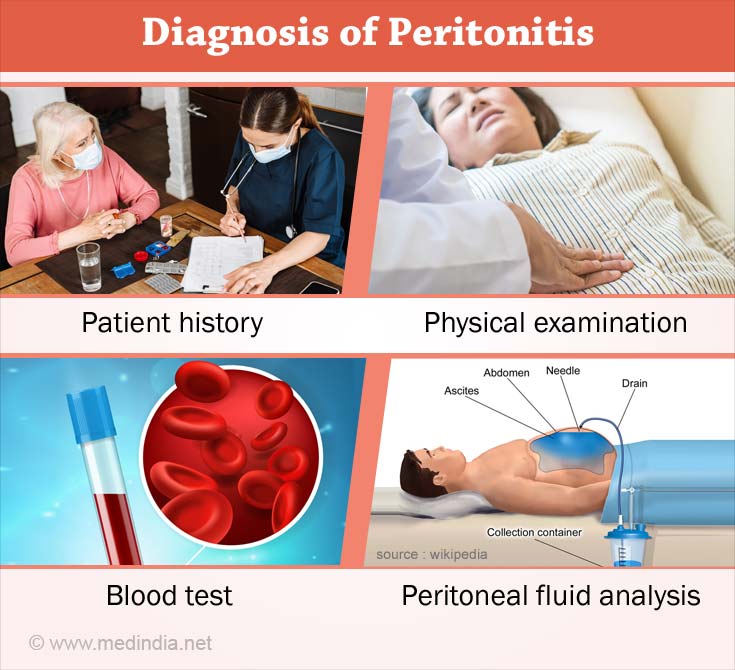
How do you Diagnose Peritonitis?
A diagnosis of peritonitis may be made from
Patient history – Patients may give history of recent abdominal pain and discomfort, or may be taking medications for previously diagnosed stomach or duodenal ulcer, or other abdominal conditions.
Physical examination – On physical examination, the abdomen (tummy) is usually tender to touch. It helps to rule out any other cause for abdominal pain such as hernia or an inflamed appendix. Associated fever and rapid pulse may be present.
If patient is undergoing peritoneal dialysis, the signs and symptoms including cloudy dialysis fluid makes it easier to diagnose the condition.
In cases of secondary peritonitis or spontaneous peritonitis the following tests are performed to confirm the diagnosis:
Blood test: A high WBC count in the blood sample is indicative of infection. A blood culture is also performed to determine whether there are bacteria in blood.
Imaging tests: An X-ray abdomen is performed to determine any holes or other perforations in the gastrointestinal tract. Ultrasound imaging is also used. Further a computerized tomography scan may be done instead of an X-ray is used for better resolution.
Peritoneal fluid analysis: A thin needle is used to withdraw a sample of the fluid from the peritoneum, especially if the patient is on peritoneal dialysis or if there is fluid in the abdomen from liver disease. In case of peritonitis, this test reveals an increased WBC count that typically indicates an infection or inflammation. A culture of the fluid also reveals the presence of bacteria, and appropriate treatment may be initiated.
How is Peritonitis Treated?
Treatment of peritonitis requires hospitalization to prevent risk of complications. Treatment includes
- Use of antibiotics - A course of antibiotic medications are prescribed to fight the infection and prevent it from spreading.
- Surgical treatment - is carried out to remove infected tissue, especially if peritonitis is due to a ruptured appendix, stomach or colon. If part of the tissue of the peritoneum is severely damaged by infection, it needs to be surgically removed.
- Drainage of pus collection within the peritoneal cavity - In some cases an abscess (pus-filled swellings) is developed in the peritoneum that needs to be drained with a needle. An ultrasound scanner is used to guide the needle to the abscess.
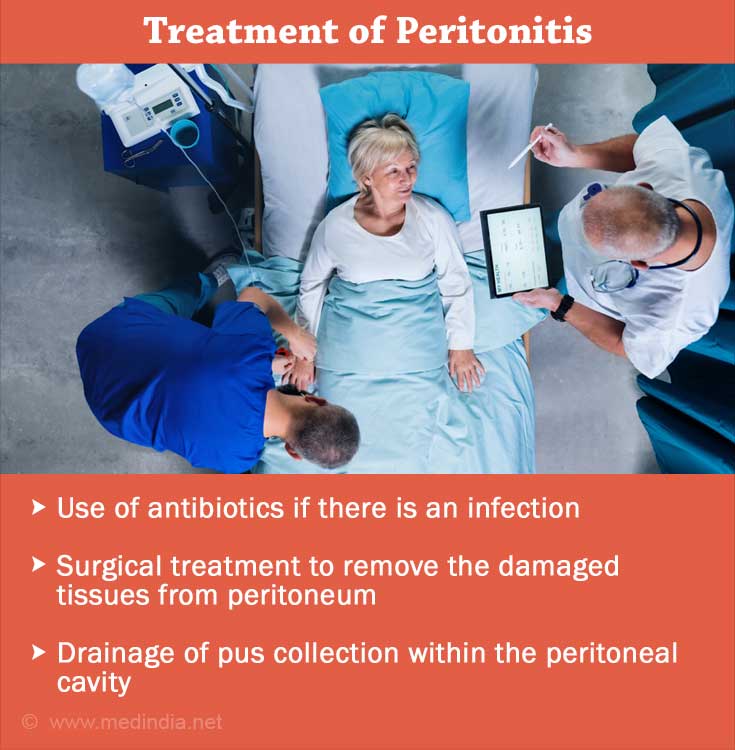
Further if the patient has peritonitis, it is recommended that they receive dialysis in another way for several days while the body heals from the infection. If peritonitis persists or recurs, peritoneal dialysis is stopped entirely and is switched to a different form of dialysis.