- Post-COVID Conditions - (https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html)
- What are the long-term side effects of COVID-19? - (https://blogs.bcm.edu/2021/02/09/what-are-the-long-term-side-effects-of-covid-19/)
- Coronavirus: Kidney Damage Caused by COVID-19 - (https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/coronavirus-kidney-damage-caused-by-covid19)
- Yellow Fungus Disease - Infection, Symptoms, Cause, Treatment - (https://www.mpnrc.org/yellow-fungus-disease-infection-symptoms-cause-treatment/)
- Fungal Diseases and COVID-19 - (https://www.cdc.gov/fungal/covid-fungal.html)
- COVID-19 and Imaging: Why CT Scans and X-Rays Have a Limited Role in Diagnosing Coronavirus - (https://blog.radiology.virginia.edu/covid-19-and-imaging/)
- COVID-19 Lung Damage - (https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/what-coronavirus-does-to-the-lungs)
- Inflammatory markers as predictors of mortality in COVID-19 infection - (https://ajlmonline.org/index.php/ajlm/article/view/1298/1808)
- Post-COVID-19 lifestyle tips to stay healthy as the pandemic eases - (https://news.llu.edu/health-wellness/post-covid-19-lifestyle-tips-stay-healthy-pandemic-eases)
- Post COVID management protocol - (https://www.mohfw.gov.in/pdf/PostCOVID13092020.pdf)
- Post-Traumatic Stress Disorder - (https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd/)
- Ventilator-associated Pneumonia (VAP) - (https://www.cdc.gov/hai/vap/vap.html)
- Hospital-acquired pneumonia - (https://medlineplus.gov/ency/article/000146.htm)
What is Post Covid Syndrome?
Post-COVID syndrome refers to the set of complications that persist even after the clinical recovery from COVID-19. Although many people recover completely from COVID-19, some people experience health issues after recovering from the initial phases of COVID-19. These post-COVID complications are of many different types and can persist for any different length of time.
Who all are at the Risk of Post-Covid Complications?
In general, anyone could experience post-covid complications. Even people who've got mild COVID-19 might experience post-COVID complications. These individuals are also referred to as "COVID long-haulers." Experts from all over the world are working on learning more about post-COVID effects.
People who seem to experience post-COVID complications are:
- Adults over the age of 50
- People who experienced a more severe case
- Individuals who have some associated chronic health conditions like diabetes, hypertension, or obesity
What are the Causes of Post Covid Syndrome?
SARS-CoV-2 can damage almost all major organs of the body, including the lungs, heart, nervous system, kidneys, and liver. Along with these, the people who got discharged after treatment in the intensive care unit (ICU) report fatigue and depression from post-traumatic stress disorder (PTSD).
While it is clear that the terrible inflammatory phases might be causing severe organ damage, especially in people who have other underlying conditions like heart disease, high blood pressure, cancer, diabetes, obesity, it is not clear why some people who have had mild COVID-19 also experienced the post-COVID effects.
Researchers worldwide are still working to find out the root cause of the post-COVID syndrome.
What are the Post Covid Long-term Symptoms and Complications?
COVID-19 can attack us from all sides, so chances of getting unexpected health problems are high. It is essential to be aware of post-COVID complications so that precautions and physiotherapy exercises can be started soon after recovering from COVID-19. Let usanalyse the significant Post-COVID issues one by one.
1. Lung or Pulmonary Issues
The primary organ affected by SARS-CoV-2 are the lungs. When the infection progresses, air sacs in the lungs become inflamed due to the accumulation of fluid. While some people recover from the SARS-CoV-2-induced deadly scars, others with even mild COVID can have lung injury that persists for a prolonged period. The conditions like pneumonia, Acute Respiratory Distress Syndrome (ARDS), or sepsis cause permanent scars in the lung tissues and result in long-lasting respiratory problems.
It has been seen that many of these badly damaged lungs require nothing short of a lung transplant.
2. Heart or Cardiac Issue
Heart damage after COVID infection can be due to many factors. As said for the lungs, SARS-CoV-2 can launch directly on the heart due to the presence of angiotensin-converting enzyme-2 (ACE-2) receptors.
The cardiovascular effects might also arise due to a solid inflammatory phase of the body due to heavy viral load leading to the inflammation of heart. This action by our immune system promotes viral clearance. However, it might unfortunately be powerful enough to damage healthy tissues, including the heart.Autopsies have shown that this infection can even affect endothelial cells and the inner surfaces of veins and arteries, resulting in compromised blood flow to the heart. These factors could cause debilitating conditions like shortness of breath, palpitations, and rapid heartbeat.
The inflammation of the heart and vessels maybe silent, and this is the reason that strenuous exercise should be avoided during the recovery phase of the disease.
3. Kidney Damage
Kidneys have the same set of receptors like lungs and heart that can launch SARS-CoV-2 directly on the tissues. People who experience a cytokine storm are more likely to develop kidney problems. Other possibilities for kidney damage are SARS-CoV-2 induced blood clots that clog the kidneys and a low oxygen level in the blood due to pneumonia. This can raise the need for dialysis in cases of severe kidney damage.
4. Neurological Problems
Neurological problems like brain fog, fatigue, headaches, insomnia, and dizziness are common among COVID survivors. Some people also experienced postural orthostatic tachycardia syndrome or POTS. This is a condition of concern as there is a possibility of a phase where the blood circulation is affected.
5. Post-COVID Diabetes
While diabetes itself is a predisposing factor for contracting severe COVID infections, some people reported developing type-2 diabetes after recovering from COVID-19.
6. Multi-organ Dysfunction
CDC defines Multisystem inflammatory syndrome in children (MIS-C) as "a condition where different body parts can become inflamed, including the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal organs." Although SARS-CoV-2 itself is deadly enough to damage multiple organs, autoimmune conditions either induced by the virus or already present can sometimes cause painful swelling of organs. This causes Multi-organ failure that could lead to chronic health conditions or mortality.
7. Secondary Infections
Like the other viral diseases, COVID-19 also induces the risk of secondary bacterial infections. The two most common bacterial respiratory and bloodstream infections are ventilator-associated bacterial pneumonia (VABP), hospital-acquired bacterial pneumonia (HABP).
When it comes to fungi, black fungus or mucormycosis, green fungus or aspergillosis, white fungus or invasive candidiasis, and yellow fungus infection are the four most common conditions that affect COVID survivors.
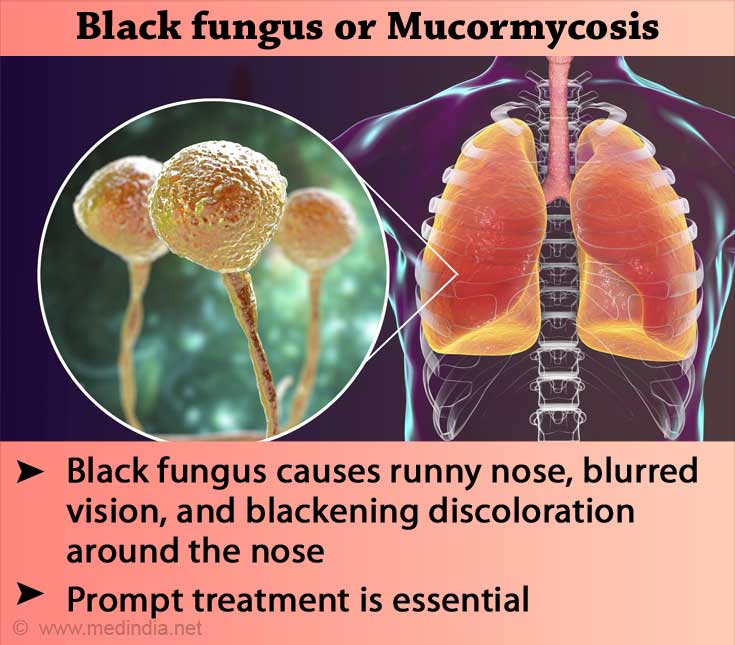
Mucormycosis or black fungus infection is a deadly fungus infection. It develops as a skin infection but disseminates fast, resulting in blurred vision, blackening, discoloration around the nose, breathing issues, and blood coughs. Aspergillosis is found to be occurring in patients who have got a severe COVID-19 infection. It can cause terrible illness and even death.
Mucormycosis or black fungus infection is a deadly fungus infection. It develops as a skin infection but disseminates fast, resulting in blurred vision, blackening, discoloration around the nose, breathing issues, and bloody coughs.
Green fungus or Aspergillosis is found to be occurring in patients who have got a severe COVID-19 infection. It can cause terrible illness and even death.
The white fungus candida can cause bloodstream infections. As some Candida species are multi-drug resistant, it would not be easy to treat them once they disseminate to the internal organs.
Yellow fungus infections can be deadlier than white and black fungi. Lack of appetite, tiredness, and even weight loss could be the symptoms of yellow fungus infections.
What causes these secondary infections in COVID?
Many factors, including lack of sanitation in healthcare settings, contaminated oxygen from cylinders, unnecessary use of antibiotics and steroids, diabetes, excess moisture in houses, are the critical causes of bacterial and fungal secondary infections.
Mental Health Issues
Mental health issues like anxiety, depression, hallucinations, and post-traumatic stress disorder (PTSD) are seen among the people who recovered from COVID-19. These disorders can occur due to various reasons.
Inflammation due to the viral attack, continuous intake of preventive medicines, physical weakness, isolation from family members, prolonged stay in the ICU are the significant causes. Other factors like the anxiety and fear of death, loss of career, financial difficulties, and death of loved ones could also increase the chances of developing psychological issues.
What are the Warning Signs of Post Covid Recovery?
Most of us note down all the symptoms during the period of COVID infection. Likewise, it is important to look out for changes in the body even after recovering from COVID-19.
Here are the common signs and symptoms to keep an eye out for after the recovery from COVID:
- Persistent cough
- Loss of taste and smell
- Persistent fever
- Breathing difficulties like shortness of breath
- Body pain, especially in joints and muscles
- Chest pain
- Heart palpitations, fast or pounding heartbeat
- Anxiety, depression, and hallucinations
- Inability to focus and concentrate
- Fatigue
- Dizziness
- Insomnia
- Worsened symptoms after physical activities
Remember that the symptoms of secondary infections include bloody cough, blurred vision, gastrointestinal issues, lack of appetite, and blood clots.
How do you Diagnose Post Covid Syndrome?
While COVID-19 is diagnosed predominantly using RT-PCR, post-COVID effects can be diagnosed using several different tests.
Although we cannot analyze each of the conditions, the results of some laboratory tests would be beneficial in detecting many post-COVID complications.
1. Diagnosis of Lung Conditions
Although not regularly suggested, chest X-rays and CT scans can confirm the diagnosis of lung disorders. COVID-19 can cause pneumonia, a condition in which the density of the lungs increases. Chest X-rays or CT-scans show these areas as white, opaque regions.
CT scans are also more sensitive in examining lung conditions. Minor issues in the lungs related to COVID-19 might heal along the end of the recovery phase. However, some people could develop scars in the lung tissues and chest CT scans can be used to examine these conditions. Observations like ground-glass opacity, vascular thickening, and pleural effusion reveal the presence of long-lasting post-covid lung problems.
2. Diagnosis of Other Important Issues
In case of suspecting any post-COVID inflammations and secondary infections, some serological tests could be helpful in the diagnosis.
Laboratory tests like Blood Count test and ESR can be preliminarily done to detect any underlying infections. Other than this, tests that determine the levels of inflammatory markers like:
- Interleukin-6,
- D-dimer,
- Neutrophil-to-lymphocyte ratio, and
- C-Reactive Protein
3. Diagnosis of Secondary Infections
The secondary infections that occur after COVID recovery can be specifically demonstrated with the help of some microbiological tests.
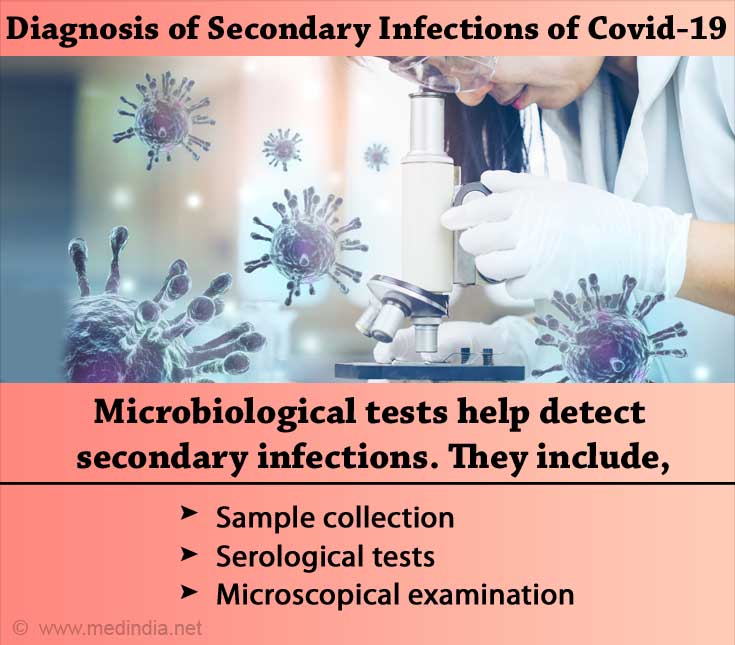
Bacterial infections can be detected using serological tests or sometimes using microscopy and culturing. Samples such as pus, exudates, lung fluid can help identify the pathogens. Serological tests require blood samples to test for specific antigens or antibodies produced against the pathogen. The blood cell counts are also considered as practical tools in identifying any underlying bacterial infections.
For fungal infections, specimens such as sputum or tissue sections are collected from the affected site. In general, microscopic examinations like potassium hydroxide mount preparation, calcofluor white staining, India ink preparation, and lactophenol cotton blue staining are used to demonstrate the fungal structures. In some cases where the infection is disseminated to the internal organs, blood samples are also collected, and appropriate serological tests are undertaken.
How can you Treat Post-COVID Syndrome?
Treatment of post-COVID complications focuses on treating the conditions developed. For example, people with underlying health conditions like diabetes or hypertension should be treated with appropriate medications to keep them under control. This can reduce the risk of many secondary health problems. Other therapies like physiotherapy and breathing therapies can help promote overall body health. A team of specialized healthcare professionals can provide comprehensive care to people suspected of developing organ damages.
Antifungal medications like amphotericin B, posaconazole, or isavuconazole can be used to treat fungal infections. In severe cases, surgical removal of the affected part is needed.
Antibiotics and steroids are double-edged swords. Using them wisely can prevent severe COVID infections and also secondary bacterial infections.
In post covid-syndrome judicious use of steroid medications and antibiotics may be required to suppress the hyperactive immune system and prevent co-infections, respectively. It should also be noted that unnecessary usage of antimicrobial drugs can increase antimicrobial resistance resulting in drug-resistant microbes.
What are the Precautions to take Post Covid Recovery?
As the post-COVID complications might be worse than the COVID-complications, taking some precautionary measures will help us escape from them. Let us see some important steps that help in the gradual healing of our body post-COVID.
1. Get Rest
The length and quality of sleep are linked to healing. Many doctors recommend that a sound sleep anywhere between 7 and 9 hours is optimal after recovering from COVID-19.
This promotes faster restoration of energy as the body gets more time to focus on healing.
2. Have a Nutritious Diet
A healthy diet can give numerous benefits, especially during the period of healing. A well-balanced diet with adequate proteins and vitamins is required to gain energy for healing. The muscle loss and weakness can also be reversed by diet. In addition to this, incorporating fruits and fluids would help in keeping us hydrated.
3. Watch out for the Warning Signs
Be aware of ‘long-COVID haul’. Any new chest pain or changes in heartbeat rate must be considered important. It is also essential to look out for the symptoms of secondary infections. Excessive sputum discharge, breathing difficulties, gastrointestinal disorders, blurred vision, blackening around the nose, skin allergies should be monitored and addressed to the healthcare professionals.
4. Do Some Exercises
You don't need to put too much load on your lungs. Practicing some simple exercises helps improve blood and oxygen circulation in the body. Regular light workouts and breathing exercises also promote detoxification and healing.
5. Care for your Mind
Patients who recovered from severe COVID infections might have anxiety and depression. To get back to normal, start boosting your confidence by practicing some mind games and puzzles and spending time with loved ones. Meditation and book-reading can also help in reducing stress and refreshing your mind.
What are the Important Ways to Slow the Spread of COVID 19?
Although post-COVID complications can be prevented or treated when diagnosed at an earlier stage, our focus should be on preventing infection with the coronavirus itself.
Here are the significant ways by which novel coronavirus disease can be controlled:
- Get vaccinated
- Stay masked
- Maintain physical distancing
- Use handwashes and sanitizers
- Stay isolated if Covid positive