- Ophthalmic Artery Chemosurgery for Intraocular Retinoblastoma - (https://www.aao.org/eyenet/article/ophthalmic-artery-chemosurgery-intraocular-retinob?july-2013)
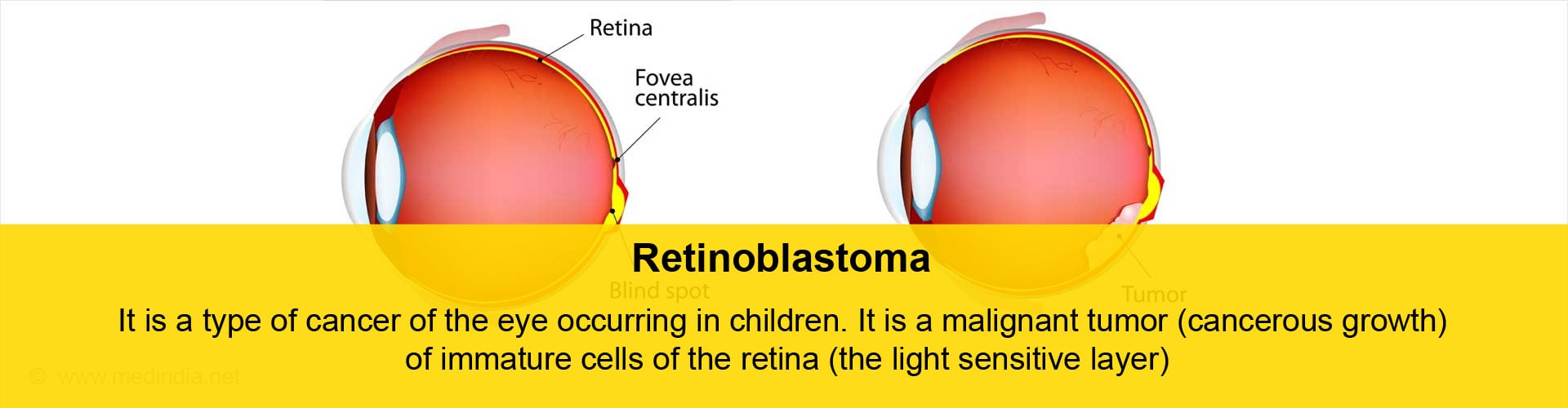
What is Retinoblastoma?
Retinoblastoma is a type of cancer of the eye occurring in children. It is a malignant tumor (cancerous growth ) of immature cells of the retina (the light sensitive layer at the back of the eye).
Facts & Statistics about Retinoblastoma
Retinoblastoma is the most common primary cancer of the eye occurring in childhood, with a frequency of 1:14,000 to 1:20,000 live births depending on the country, and accounts for 3% of all childhood cancers. It is more frequent in Africa and India. About 80 % of retinoblastoma cases are diagnosed before 3 years of age.
Untreated retinoblastoma can be fatal; in developed countries, advances in treatment have resulted in a 95 to 99% survival rate.
What are the Types of Retinoblastoma?
Retinoblastoma occurs in 2 forms – a heritable and a non-heritable (sporadic) form. Heritable retinoblastoma indicates that the tendency to develop retinoblastoma is transmitted from parents to offspring, and accounts for 40% of the cases. The differences between the two forms are listed below:
| Heritable retinoblastoma | Sporadic retinoblastoma | |
| Percentage of total retinoblastoma cases | 40 | 60 |
| Laterality | Bilateral in 85 % of cases | Unilateral |
| Average age at diagnosis | 12-15 months | 24 months |
| Transmissible to offspring | Yes | No |
| Predisposition to second nonocular cancers | Yes | No |
| Multifocal tumors(multiple growths in different parts of the retina ) | Yes | No |
| Family history of retinoblastoma | Present in 10-20% of cases | Absent |
| Associated with increased paternal age | Present in some cases | Absent |
Children with the heritable type of retinoblastoma are more at risk of developing cancer (second non-ocular cancers) in other organs of the body, the most common of which are osteogenic sarcoma (bone cancer), soft tissue sarcomas and melanomas (tumors of pigmentary cells). These second cancers are more common in patients who have received radiotherapy for their retinoblastoma, and even more so when this radiation has been given before 12 months of age. These second primary malignancies are the most common cause of death following retinoblastoma in developed countries.
Why does Retinoblastoma occur?
The development of most cases of retinoblastoma may be explained by Knudson’s two hit hypothesis.
Every individual has 23 pairs of chromosomes, one chromosome of every pair obtained from each parent. Genes (containing codes to synthesize proteins and thus determining various characteristics of an individual) are situated on these chromosomes. The retinoblastoma gene (or RB1) is situated on the 14th band of the long arm of chromosome 13 (13q14). This is a tumor suppressor gene. This means that presence of this gene in its normal form protects against retinoblastoma.
According to Knudson’s two hit hypothesis, the DNA has to suffer ‘two hits’ or two mutations for the cancer to occur.
In the heritable type of retinoblastoma, one mutation is inherited from the parent, and so all the cells in the body have this mutation (germline mutation). The second mutation occurs later after fertilization in the retinal cells, resulting in retinoblastoma (somatic mutation). In the sporadic variety, both mutations occur within a single retinal cell after fertilisation of the egg (both are somatic mutations).
Recently, another variety of retinoblastoma has been discovered, where the retinoblastoma gene was normal, but there was a high level of amplification of the MYCN gene only in the tumor cells. This does not result in heritable retinoblastoma, and these children do not have any of the characteristics of heritable retinoblastoma, including the risk of transmission to offspring.
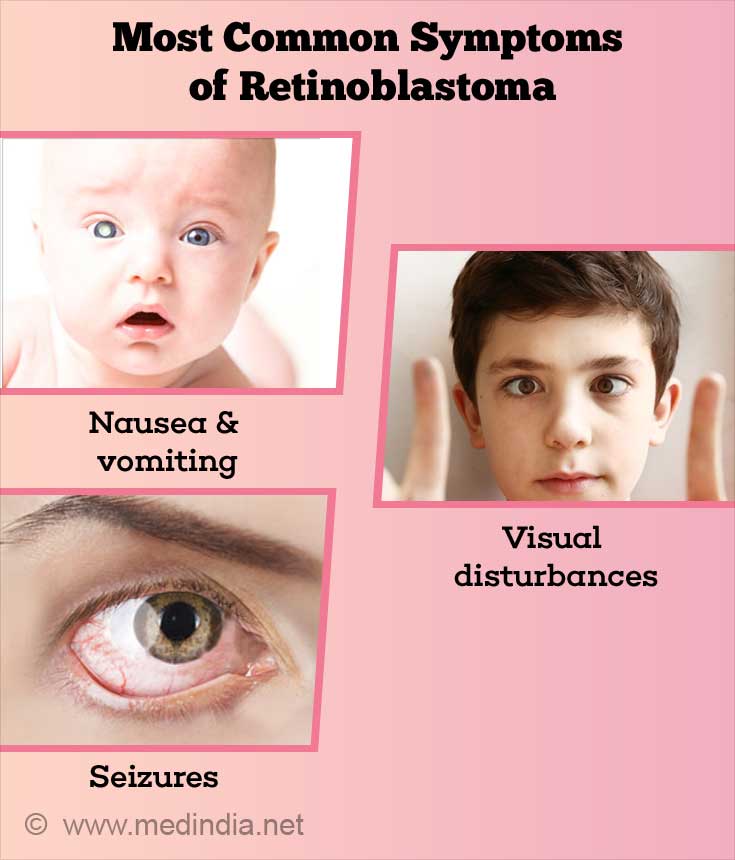
What are the Symptoms of Retinoblastoma?
Retinoblastoma may present in a variety of ways. However, the most common modes of presentation are -
| Most common modes of presentation of retinoblastoma | |
| Leucocoria (white reflex in pupil or amaurotic cat’s eye reflex) In 60% of cases | The pupil that normally appears dark, now appears whitish in color due to the tumor or detached retina showing through the pupil |
| Strabismus or squint In 20% of cases | Either an outward or inward deviation of the affected eye occurs |
| Ocular inflammation In 5% of cases | The eye is red and whitish pus like material may be seen behind the cornea |
Less common modes of presentation include blood in the anterior chamber (seen behind the cornea), cataract, increased pressure in the eye and inflammation of the tissues surrounding the eye. In neglected cases, spread outside the eyeball results in the eye being pushed forward (proptosis) and appearing very prominent.
Retinoblastoma most commonly spreads along the optic nerve and into the brain and skull bones. It spreads through the blood to the bone marrow. Other organs to which it can spread are bones of the arms and legs, spinal cord, lymph nodes and abdominal organs.
How do you Diagnose and Evaluate a Child with Retinoblastoma?
- The diagnosis of retinoblastoma is mainly clinical. The classical presentation of leucocoria or whitish appearance of the pupil should be considered to be retinoblastoma unless proved otherwise. The pupil is dilated and a detailed fundus (examination of the retina) is carried out, to determine if the tumor is monofocal or multifocal. If multifocal, all the tumors should be documented. Since most children in this age group are not very cooperative, an examination under anesthesia is required in all patients for a thorough assessment of ocular disease prior to treatment.
- Ultrasonography (ultrasound examination of the eye and orbit) measures the tumor size and shows the presence of heterogeneity (variations in the tumor) and calcification (accumulation of calcium in tissues)
- CT (computed tomography) scan of the eye may show calcification. However, CT scan is less preferred because it exposes the child to radiation.
- MRI (magnetic resonance imaging) of the eye, orbit and head is the preferred mode of imaging to evaluate the tumor in the eye and to detect possible extension into the orbit and brain. MRI can also detect if there an associated tumor of the pineal gland; this condition is referred to as trilateral retinoblastoma. MRI also helps in differentiating other conditions that simulate retinoblastoma.
- If extension into the optic nerve (the nerve at the back of the eye that transmits visual signals from the retina to the brain) is suspected, a lumbar puncture (placing a needle into the back and withdrawing cerebrospinal fluid which surrounds the spinal cord) may be done.
- If there is evidence of extension outside the eye, bone scans and bone marrow testing to detect the spread are required.
- Genetic studies to determine heritability and the type of genetic involvement are done to help in genetic counselling.
What are the Conditions that Simulate Retinoblastoma?
There are a number of conditions that simulate retinoblastoma as they also cause leucocoria or a whitish appearance of the pupil. Though all of these conditions (collectively referred to as pseudoglioma) should be kept in mind and the patient must be examined to rule out these conditions, leucocoria should be considered to be due to retinoblastoma unless proved otherwise, as this condition can be fatal.
| Conditions that simulate retinoblastoma | |
| Persistent hyperplastic primary vitreous ( PHPV) |
|
| Retinopathy of prematurity |
|
| Congenital cataract |
|
| Coat’s Disease |
|
| Cyclitic membrane |
|
| Fundus coloboma |
|
| Toxocara Endophthalmitis |
|
| Norrie’s Disease |
|
| Incontinentia Pigmenti |
|
| Familial Exudative Vitreoretinopathy |
|
How do You Treat Retinoblastoma?
The management of retinoblastoma involves a multidisciplinary approach and involves ophthalmologists, pediatric oncologists (doctors who specialise in cancer in children), pathologists, radiation oncologists (doctors who specialise in giving radiotherapy for cancers) and genetic counsellors. The primary focus of treatment in advanced disease is the preservation of life; however modern techniques have more precise goals like preservation of the eyeball and vision as far as possible.
The treatment of retinoblastoma involves strategically choosing among the various available modalities according to the individual case. This would depend on laterality, stage of the disease, age of the child and presence of spread at the time of diagnosis. In children who present with advanced disease contained in one eye with no visual potential in that eye, that eye is surgically removed , resulting in a 95- 99% cure rate. Where there is visual potential or in bilateral tumors, chemotherapy (treatment with anti-cancer drugs) is the treatment of choice. Chemotherapy is often used in conjunction with other modalities, especially in the concept of chemoreduction, wherein the size of the tumor is reduced with chemotherapy, thus rendering the tumor amenable to one of the local therapies.

The following table lists some of the important modalities of treating retinoblastoma.
| Various treatment modalities for retinoblastoma | ||
| Chemotherapy (use of anti-cancer drugs) | Intravenous (injection into the veins of the arms) |
|
| Intra-arterial (injection into the ophthalmic artery which supplies the main central artery of the retina) |
| |
| Periocular (injection into the tissue around the eyeball) |
| |
| Intravitreal |
| |
| Laser Photocoagulation | Laser application with argon or diode laser |
|
| Cryotherapy | Exposure of the tumor to very cold temperatures |
|
| Brachytherapy | Placement of a radioactive implant (Iodine-125 or Ruthenium-106) on the sclera near the base of the tumor |
|
| Enucleation | Surgical removal of the tumor containing eyeball |
|
| Transpupillary thermotherapy (with or without the aid of indoycanine green) | Application of heat through the pupil by infrared diode laser |
|
| External beam radiotherapy | Application of radiation to the eyeball region from outside |
|
What is the Prognosis (Outcome) of Retinoblastoma?
Retinoblastoma is fatal if untreated due to spread to the brain and various organs of the body. Since early diagnosis and treatment is optimal in industrialised countries, the prognosis for the eyes is very good. The latest techniques of intra-arterial chemotherapy (referred to as ophthalmic artery chemosurgery or OAC) and intravitreal injections have reduced the need for removal of the eyes, and for external beam irradiation. However, long term outcomes still depend on the development of secondary tumors, predominantly bone tumors. The risk of second tumors increases with radiation for the treatment of the original condition.
Adult survivors of retinoblastoma often have subnormal visual function.
What is the Protocol for Patients With Successfully Treated Retinoblastoma?
Children with unilateral retinoblastoma without a germline mutation have a very small risk of developing a tumor in the other eye. A regular clinical eye examination and ultrasound examination is recommended.
With treated bilateral retinoblastoma, clinical examinations are conducted every 3-6 months up to the age of 7 years, then annually, and later every 2 years for life not only for new retinal tumors, but also for other second non-ocular tumors.
Patients with heritable retinoblastoma should preferably avoid radiotherapy, tobacco and exposure to sunlight (agents that damage DNA and thus predispose to cancers) to reduce the risk of second non-ocular tumors.
Individuals with retinomas (non-cancerous retinal tumors) should undergo clinical examination and imaging every 1-2 years to detect malignant (cancerous) change.
Genetic Counselling
Genetic counselling forms an integral part of the management of a patient with retinoblastoma. The susceptibility to heritable retinoblastoma is inherited in an autosomal dominant manner. Unfortunately, genetic counselling is very complicated in retinoblastoma and depends on the type of retinoblastoma and genetic testing. The following table gives the risk of having children with retinoblastoma, and the risk for subsequent children if one child develops the disease.
| Parent has - | Risk of having a child with retinoblastoma | If one child has retinoblastoma, risk for subsequent children getting retinoblastoma |
| Bilateral retinoblastoma | 45-50 % | 45-50 % |
| Unilateral retinoblastoma | 7 – 15 % | 45-50 % |
| Unaffected | < 1% | 5% |
| Unaffected , but a carrier | 45-50 % | 45-50 % |
The above table is a simplified version, and actual risks should be determined after molecular genetic testing of the blood of at risk persons.
How Do You Prevent Retinoblastoma?
- Retinoblastoma can only be prevented by proper genetic counselling, wherein parents do not go in for more children if there is a high risk for developing retinoblastoma.
- Pre-implantation genetic diagnosis may be made by testing the embryo after in-vitro fertilisation (test tube baby). If found to have the retinoblastoma gene mutation, then implantation may be deferred, thus preventing a pregnancy in which the child is at risk.
- Prenatal genetic testing (during pregnancy) may be done by chorionic villus sampling (cells from placenta) before 12 weeks of pregnancy, or from amniotic fluid (after 12 weeks of pregnancy). If found to be positive for the mutant gene, then fetal ultrasound can be used for early detection of tumors, and an early delivery may be planned to start early treatment. However, non-continuation of pregnancy has certain medical and legal issues which need to be ascertained.
Screening of Family Members
- In the absence of a family history, the parents of a child with retinoblastoma should be examined for healed retinal scars or evidence of a retinoma (non-cancerous form of retina tumor). These directly support the heritable form of retinoblastoma.
- Siblings of a child with retinoblastoma should undergo molecular genetic testing, and if found to have a germline mutation, should undergo clinical examination every 3-4 weeks until the age of 1 year, and every 3-4 months until the age of 5 years. After that, annual screening and clinical examination of the entire body should be carried out for life.
- Any person with a retinoma should be screened with eye examination http://www.medindia.net/health-screening-test/routine-eye-examination.htm About Routine Eye Examination and ultrasound every one or two years for life.