- Trachoma - (http://www.mayoclinic.org/diseases-conditions/trachoma/basics/definition/con-20025935)
- Trachoma teaching set - (http://www.cehjournal.org/resources/trachoma-teaching-set-full-text/)
- Trachoma - Definition - (https://en.wikipedia.org/wiki/Trachoma)
- Review of Medical Microbiology and Immunology 13th Ed, Warren Levinson MD PhD - (http://www.cehjournal.org/resources/trachoma-teaching-set-full-text/)
- We Can Stop One of the World’s Leading Causes of Blindness by 2020 - (http://www.trachoma.org/about-trachoma)
- What Is Trachoma? - (https://www.aao.org/eye-health/diseases/what-is-trachoma)
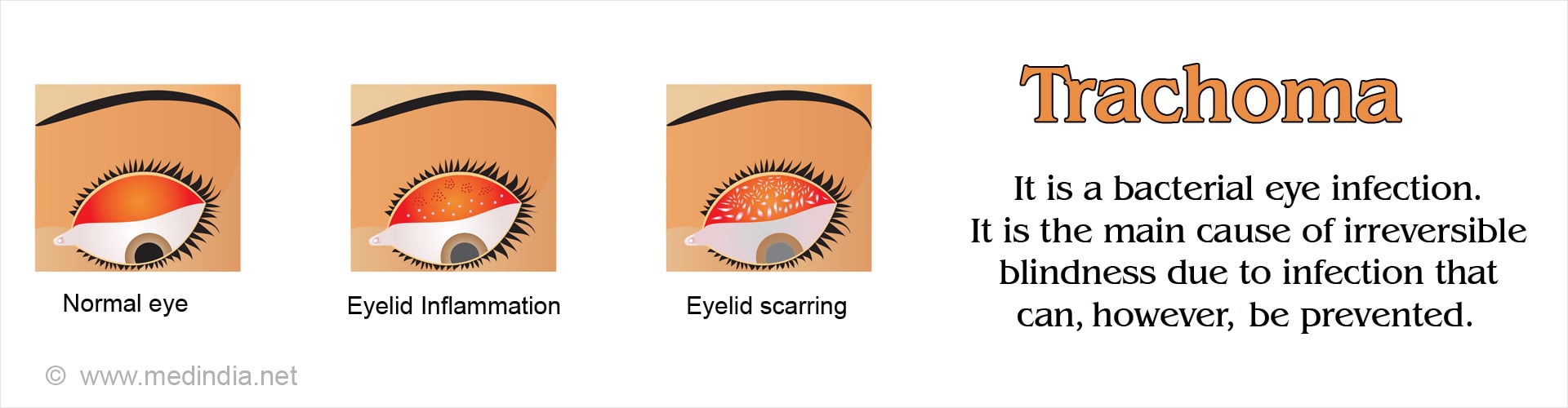
What is Trachoma?
Trachoma is one of the oldest diseases known to mankind and has occurred in many parts of the world including the United States and Europe as recently as the 20th century. With advancements in treatment and improvements in hygienic conditions, many countries have succeeded in eradicating trachoma but it still remains a serious health concern in nearly 42 countries worldwide.
Recognizing the seriousness of the problem, the World Health Organization (WHO) adopted a resolution in 1998 to eradicate trachoma as a public health problem by 2020.
How is Trachoma Caused?
Trachoma is caused by Chlamydia trachomatis, a bacterium found in the discharge from the eyes and nose of infected individuals. The infection is contagious and spreads from person to person via hands, clothes or shared bedding. It can also be spread by flies which have been in contact with the infected discharge.
In areas where the disease is endemic, it usually affects pre-school children and infection spreads from one child to the other in the family setting, usually in overcrowded and poor sanitary conditions.
What are the Risk Factors of Getting Trachoma?
The following are the risk factors of being infected with trachoma:
- Poor hygiene – Unclean hands and faces increases risk of spread of trachoma
- Poverty – The disease is endemic in developing countries amongst the very poor due to overcrowded and unhygienic living conditions, not to mention malnutrition
- Lack of sanitation – Absence of toilets increases the incidence of the disease
- Gender – In many populations, women are more susceptible, possibly because they are the primary caregivers for the affected children
- Age – The disease is most commonly seen in children between the ages of 4-6 years
- Flies – In places where there are many flies, the risk of transmission is much higher

Important Facts and Figures about Trachoma
- Trachoma is an endemic disease and a major public health concern in 42 countries globally. More than 200 million persons living in trachoma endemic areas are at risk. It has caused the blindness of nearly 2 million persons worldwide.
- The disease is highly endemic in the most backward and poorest regions of Africa, Asia and Middle East, South and Central America, and Australia. Africa remains the most affected continent.
- It is a common and preventable cause of blindness.
- The WHO adopted a resolution in 1998 to work towards global eradication of trachoma as a public health issue by the year 2020.
- The health cost due to trachoma and the economic impact due to loss of productivity following blindness and visual deficit caused by trachoma is estimated to be between US $ 3-5 billion annually.
- Blindness due to trachoma is irreversible, and can only be cured through corneal.
- In 2015 alone, approximately 56 million persons worldwide were treated with antibiotics and nearly 200,000 persons underwent surgery for advanced disease.
- The WHO theme for the elimination of trachoma encapsulates the acronym ‘SAFE’
- S – Surgery for advanced disease
- A – Antibiotics for C trachomatis infection
- F – Facial cleanliness
- E – Environmental improvement to decrease risk of spread.
What are the Symptoms and Signs of Trachoma?
Following infection, symptoms appear within a week or two. Initially the symptoms are mild and include mild irritation and pain in the eyes and the eyelids. Repeated attacks or untreated infection ultimately leads to scarring and visual impairment. Symptoms of trachoma include the following:
- Mild irritation and itchiness of eyelids
- Pain in the eyes
- Light sensitivity (photophobia)
- Swelling of the eyelids
- Mucoid or mucopurulent discharge from the eyes

What are the Complications of Trachoma Infection?
A single infection of trachoma is easily treated with antibiotics. Repeated and recurrent infections, as is bound to occur in highly endemic zones, can lead to long-term complications such as the following:
- Thickened eyelid and scar formation on the inner aspect of the eyelid. The upper eyelid is more commonly involved
- Indrawing of the eyelid (entropion) and ingrowing of the eyelashes (trichiasis)
- Opacity or clouding of the outer layer (cornea) of the eye
- Blindness or visual impairment
- Dryness of eyes
How do you Diagnose Trachoma?
In endemic areas, diagnosis is usually made based on physical examination. The Chlamydia trachomatis bacterium cannot be detected by routine laboratory tests that are employed for other bacterial agents. Confirmation of the diagnosis necessitates sending a sample of the eye discharge to specialized labs for tests which may not be available in these areas..
Recognizing the appearances and prompt treatment with antibiotics is essential to prevent complications. The WHO has identified 5 stages in the evolution of trachoma infection.
- Stage of follicular inflammation – Presence of tiny follicles (tiny bumps) 5 or more in number on the inner surface of the upper eyelid.
- Stage of intense inflammation – The eye becomes infectious and the upper eyelid becomes thickened and swollen.
- Scarring of eyelid – Repeated episodes of infection cause scarring of the upper eyelid which may become drawn inwards.
- Stage of ingrown eyelashes – The deformed and scarred eyelids cause the eyelashes to grow inwards and rub against the outer transparent surface of the eye, the cornea, through which light normally enters the eye.
- Clouding of the cornea – Due to repeated irritation by rubbing of the ingrown eyelashes, the cornea becomes clouded or opaque. This can lead to loss of vision.
With the evolution of the disease through the various stages, the cornea becomes opaque resulting in gradual loss of vision. Typically, the visual impairment occurs between 30-40 years of age but may occur earlier in highly endemic regions where the transmission is intense.
How do you Treat Trachoma?
The treatment of trachoma depends on the stage. In the initial stages, the disease is easily treated with antibiotics.
Medications
- The World Health Organization (WHO) recommends one of two antibiotics for trachoma treatment namely, oral azithromycin or local application of tetracycline as an ointment.
- The advantages of azithromycin are that it is administered as a single dose under the supervision of the health care authorities; therefore, the health care worker can be sure that the patient has taken the medication. It is highly effective and has very few side effects which may include nausea, vomiting, diarrhea and rash. It is also effective against incidental skin, respiratory or genital Chlamydia trachomatis infections that might be present.
- Tetracycline is a cheaper agent but its use by patients cannot be confirmed as it is not administered under the supervision of healthcare workers.
- The WHO recommends treating the entire population in communities where more than 10 percent of the children are affected. This measure is to reduce the spread of the disease.
Surgical treatment
Surgery is recommended in advanced disease with complications. The various surgical options include the following:
- Eyelid rotation surgery (bilamellar tarsal rotation) – A tiny cut is made on the scarred eyelid and it is rotated away from the cornea. This will prevent rubbing of the eyelashes against the cornea and reduce or prevent corneal scarring and opacities, thereby halting the progression of loss of vision.
- Corneal transplant – If the cornea has become severely opaque, corneal transplant is an option to restore the vision. Unfortunately, this procedure does not show good results in trachoma.
- Epilation – This procedure is done to pluck out the ingrowing eyelashes rubbing on the cornea; it will need to be repeated regularly.
- Placing an adhesive tape over your eyelashes to keep them from touching the corneal surface is a temporary option when surgery is not available.
How do you Prevent Trachoma?
The adage, ‘prevention is better than cure’ is very applicable to trachoma. The disease can be easily prevented and rate of transmission reduced by following the measures outlined below:
- Keeping face and hands clean to prevent re-infection.
- Access to clean water for bathing, washing and for use in toilets
- Proper disposal of human and animal waste to reduce spread through flies
- Fly control measures.
The WHO has adopted a resolution to prevent trachoma infection and eradicate it by 2020. It is actively implementing the SAFE strategy to make its goal a reality.
What is the Prognosis of Trachoma?
Trachoma is easily treatable with antibiotics, and complications such as blindness can be avoided. However, in the poorest population, lack of awareness, poor sanitary conditions and access to health care results in advanced disease with complications leading to blindness and visual impairment.