- Von Hippel-Lindau Disease - Genetic and Rare Diseases Information Center (GARD), National Center for Advancing Translational Sciences, National Institutes of Health (NIH), USA - (https://rarediseases.info.nih.gov/diseases/7855/von-hippel-lindau-disease)
- Von Hippel-Lindau Syndrome - Genetics Home Reference, National Institutes of Health (NIH), USA - (https://ghr.nlm.nih.gov/condition/von-hippel-lindau-syndrome#)
- Von Hippel-Lindau Disease - National Organization for Rare Disorders (NORD) - (https://rarediseases.org/rare-diseases/von-hippel-lindau-disease/)
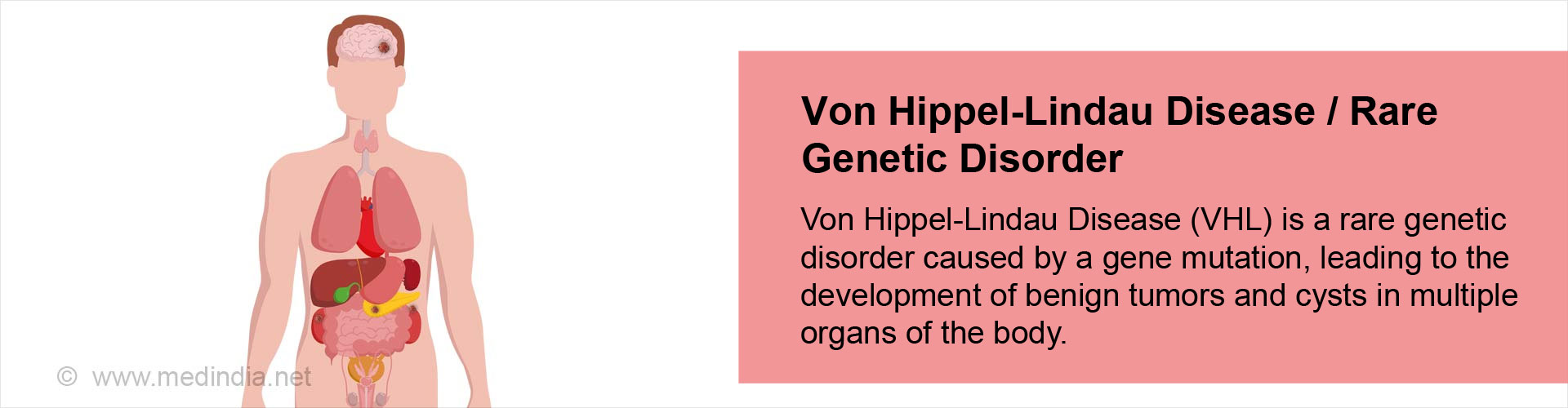
What is Von Hippel-Lindau Disease?
Von Hippel-Lindau Disease (VHL) is also known as Von Hippel-Lindau Syndrome / VHL Syndrome / Angiomatosis retinae / Familial cerebello-retinal angiomatosis. It is a rare genetic disorder that is characterized by formation of tumors and cysts (fluid filled sacs) in multiple organs of the body, which involve the ectodermal structures like the central nervous system (CNS), skin, and eyes. The tumors are generally benign (non-cancerous) but have the potential to become malignant (cancerous). The most common types of tumors are hemangioblastomas, which are tumors of the blood vessels of the brain, spinal cord, and eye. The symptoms of VHL generally occur in adolescents, although these can persist throughout life.
Epidemiology of Von Hippel-Lindau Disease
The prevalence of VHL is estimated to be 1 in 53,000 and an incidence of 1 in 36,000 individuals. The disease can be diagnosed starting from infancy to 70 years, with 26 years being the mean age at diagnosis. VHL affects men and women equally. Approximately 20% of VHL patients do not have a family history of the disease. In these cases, a mutation (alteration) in the VHL gene occurs de novo for the first time.
Origin of the Term “Von Hippel-Lindau Disease”
Von Hippel-Lindau disease is named after Eugen Von Hippel, a German ophthalmologist and Arvid Vilhelm Lindau, a Swedish pathologist. In 1904 Von Hippel first described angiomas in the eye, while Lindau described angiomas of the cerebellum and spine in 1927. As a result, the term “Von Hippel-Lindau Disease” was first used in 1936 and gained acceptance and became established in the medical literature from the 1970s.
What are the Causes of Von Hippel-Lindau Disease?
Von Hippel-Lindau disease is a genetic condition, which means that it can be passed on from generation to generation. It is caused by a mutation in the VHL gene located on chromosome 3p25.3. This gene is a tumor suppressor gene, which prevents uncontrolled cell division, thereby preventing tumor formation. The presence of the mutation knocks-out this gene so that there is no check, leading to uncontrolled cell proliferation, resulting in formation of the various types of tumors seen in VHL patients. VHL follows an autosomal dominant mode of inheritance, meaning that the presence of even a single mutation in the VHL gene can increase the risk of developing the disease.
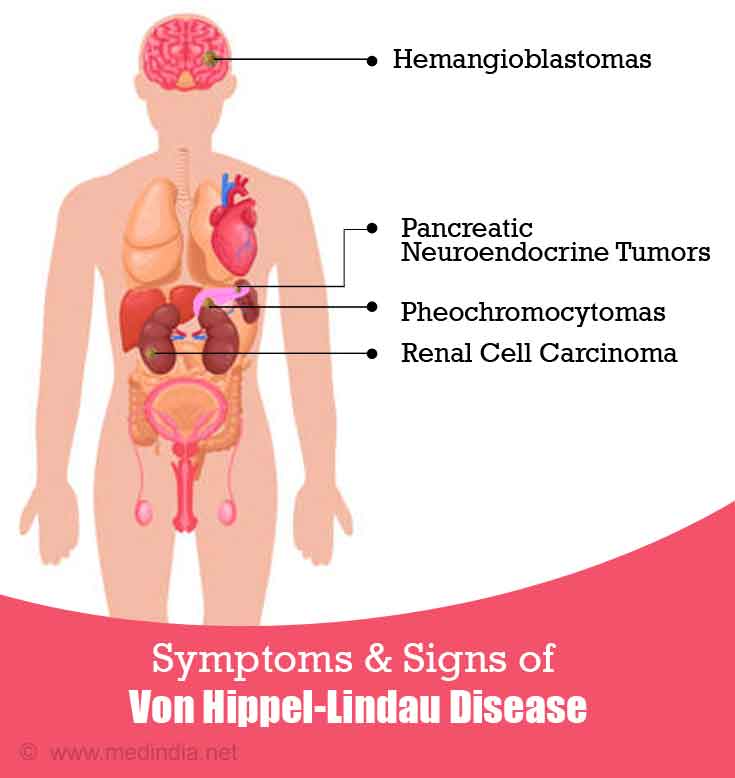
What are the Symptoms & Signs of Von Hippel-Lindau Disease?
The symptoms and signs of VHL that are observed are associated with the various types of tumors. These are briefly described below:
- Hemangioblastomas:
These types of tumors are often associated with the brain and spinal cord and bring about symptoms such as headaches, weakness, ataxia (loss of muscle coordination), nausea, and vomiting. Hemangioblastomas can also occur in the retina, which are termed as retinal angiomas and can result in blindness.
- Pheochromocytomas:
These are tumors of the adrenal glands, which are usually non-cancerous and generally do not produce any symptoms. However, sometimes, due to increased hormone secretion, an acute increase in blood pressure can occur, which does not respond to medications. Other symptoms include headache, panic attacks, and profuse sweating.
- Renal Cell Carcinoma:
Patients with VHL are at an increased risk of developing a special type of kidney cancer called renal cell carcinoma (RCC), which can occur in up to 70% of VHL patients by the age of 60 years. Some of the major symptoms of RCC include hematuria (blood in urine), lower back pain, anemia, loss of appetite, weight loss, fatigue, fever, and development of a lump on one side.
- Endolymphatic Sac Tumors:
These tumors are benign and occur in the inner ear. Approximately 10% of patients suffering from VHL develop these tumors. Some of the symptoms include hearing loss, tinnitus (ringing/buzzing in the ears), as well as problems with maintaining balance while standing and/or walking.
- Pancreatic Neuroendocrine Tumors:
These are also known as islet cell tumors and are a group of endocrine (hormonal) tumors arising in the pancreas and are among the most common neuroendocrine tumors. The symptoms depend on the hormones secreted by the tumors, which may include hypoglycemia (low blood sugar), stomach ulcers, gallstones, and severe diarrhea.
How do you Diagnose Von Hippel-Lindau Disease?
Diagnosis of Von Hippel-Lindau disease is based upon the clinical symptoms and signs. There is a need for periodic check-ups or screening for early diagnosis of the disorder. These are briefly highlighted below:
- Blood and Urine Tests: A yearly blood test and/or 24-hour urine test is recommended, which determine the levels of catecholamines and its metabolites. These tests should be started from the age of 5 years.
- Fundoscopy: This technique can be used to examine and visualize the fundus (interior surface of the eye opposite the lens and including the retina) of the eye using a device called fundoscope. Fundoscopy is useful for diagnosing angiomas of the eye at an early stage.
- Magnetic Resonance Imaging (MRI): An MRI of the brain and spine is recommended every 2 years, beginning in the teenage years to visualize any tumors that may be present.
- Ultrasonography (USG): A yearly USG of the abdomen is recommended to detect any abnormalities in the kidneys, pancreas, and adrenal glands. This should be started from the teenage years, and should be switched to either computed tomography (CT) scan or MRI after reaching adulthood.
- Audiometry: Periodic hearing check-up is recommended for early detection of signs of hearing loss.
- Genetic Testing: This is the definitive test for VHL. This molecular test uses the polymerase chain reaction (PCR) to amplify the VHL gene and is coupled with techniques such as Southern blotting and DNA sequencing to detect any mutation. The presence of a mutation in this gene indicates a positive test.
How do you Treat Von Hippel-Lindau Disease?
Although it is not possible to reverse the effects of mutations in the VHL gene, it is however, possible to treat the symptoms so that the patients can have a better quality of life. Some of the treatment options that are available are indicated below:
- Laser Photocoagulation: This is a surgical procedure that uses a laser beam to cauterize (close or seal off by burning) the minute blood vessels to the eye in order to bring about therapeutic benefits. This is used for treating retinal angiomas.
- Cryotherapy: This technique involves the use of freezing or near-freezing temperatures to treat a variety of benign and malignant lesions, including retinal angiomas.
- Partial Nephrectomy: This is also known as nephron sparing surgery and involves the surgical removal of only the damaged portion of the kidney.
- Radiofrequency Ablation: This procedure uses heat generated from medium frequency alternating current (AC) to ablate (surgically remove) the tumor.
- Radiation Therapy: Since even the benign tumors can potentially become cancerous, radiation therapy may be useful in these circumstances.
What are the Related Disorders of Von Hippel-Lindau Disease?
Some related disorders associated with VHL, which should be kept in the differential diagnosis include the following:
- Birt-Hogg-Dubé syndrome
- Neurofibromatosis
- Multiple endocrine neoplasia
- Polycystic kidney disease
- Tuberous sclerosis
- Hereditary paraganglioma-pheochromocytoma syndrome
What is the Prognosis for Von Hippel-Lindau Disease?
The outlook or prognosis for VHL depends on the type of tumor. Death is most common in case of RCC, followed by CNS hemangioblastomas. Previously, the average life expectancy was estimated to be 50 years. However, now the mortality and morbidity has decreased appreciably due to improved screening and early diagnosis and treatment.