- Postpartum psychosis - (https://www.nhs.uk/mental-health/conditions/post-partum-psychosis/)
- About Postpartum psychosis - (https://www.rcpsych.ac.uk/mental-health/problems-disorders/postpartum-psychosis)
- Postpartum Depression: Who is at Risk? - (https://womensmentalhealth.org/posts/postpartum-depression-who-is-at-risk/)
- About Postpartum depression - (https://www.womenshealth.gov/mental-health/mental-health-conditions/postpartum-depression)
- Psychological Distress in the Mother May Affect Levels of Immunoglobulins in Breast Milk - (https://womensmentalhealth.org/posts/psychological-distress-mother-may-affect-levels-immunoglobulins-breast-milk/)
- Postnatal Depression - (https://www.clinicbarcelona.org/en/assistance/diseases/postnatal-depression/progression-of-the-disease)
- Postpartum depression Diagnosis - (https://www.mayoclinic.org/diseases-conditions/postpartum-depression/diagnosis-treatment/drc-20376623)
- Know More About About Postpartum depression - (https://my.clevelandclinic.org/health/diseases/9312-postpartum-depression)
- Postpartum Depression (PPD) - (https://familydoctor.org/condition/postpartum-depression/)
- Treatment of Mild to Moderate Postpartum Depression during Breastfeeding. - (https://www.researchgate.net/figure/Treatment-of-Mild-to-Moderate-Postpartum-Depression-during-Breastfeeding_tbl2_305794987)
- Perinatal depression and psychosis: an update - (https://www.cambridge.org/core/journals/bjpsych-advances/article/perinatal-depression-and-psychosis-an-update/A6B207CDBC64D3D7A295D9E44B5F1C5A)
- Long-Term Outcomes of Postpartum Psychosis: What is the Risk of Recurrence? - (https://womensmentalhealth.org/posts/recurrence-of-postpartum-psychosis/)
- Long-term outcome of postpartum psychosis: a prospective clinical cohort study in 106 women - (https://journalbipolardisorders.springeropen.com/articles/10.1186/s40345-021-00236-2)
- Treatment of postpartum depression: clinical, psychological and pharmacological options - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3039003/)
- Management of postpartum psychosis - (https://www.cope.org.au/new-parents/postnatal-mental-health-conditions/postpatum-psychosis/management-postpartum-psychosis/)
- Postpartum Depression and the Baby Blues - (https://www.helpguide.org/articles/depression/postpartum-depression-and-the-baby-blues.htm)
- Postnatal depression and perinatal mental health - (https://www.mind.org.uk/information-support/types-of-mental-health-problems/postnatal-depression-and-perinatal-mental-health/postpartum-psychosis/)
What is Postpartum Psychosis?
Postpartum or postnatal or puerperal psychosis is a psychological disorder that is seen following the birth of a child, in a parent, typically the mother. This disorder is characterized by the following symptoms:
- Delusions — False beliefs that are held firmly. An example of this could be, “God wants me to sacrifice this baby.”
- Hallucinations — Experiencing through the senses stimuli that are not present in reality.
- Mood Lability — High extremes of moods ranging from mania to depression or fast changing moods. Mania is characterized by rapid speech, beliefs of grandiosity, and high energy levels. Depression involves sadness, fatigue, lack of energy, and disturbed sleep and appetite.
- Suspiciousness and tendency to be easily scared.
- Restlessness that may be seen in thoughts, speech, and behaviors such as pacing or fidgeting.
- Inappropriate or eccentric behavior that is not in character.
- Confusion
Postnatal psychosis is caused by several factors. Genetics and family history have been found to have a strong association. Hormonal imbalance and impaired sleep could also be causal factors.
What is Postpartum Depression (PPD)?
Postnatal depression is a postpartum mood disorder typically seen in mothers and rarely in fathers. This disorder has the following symptoms:
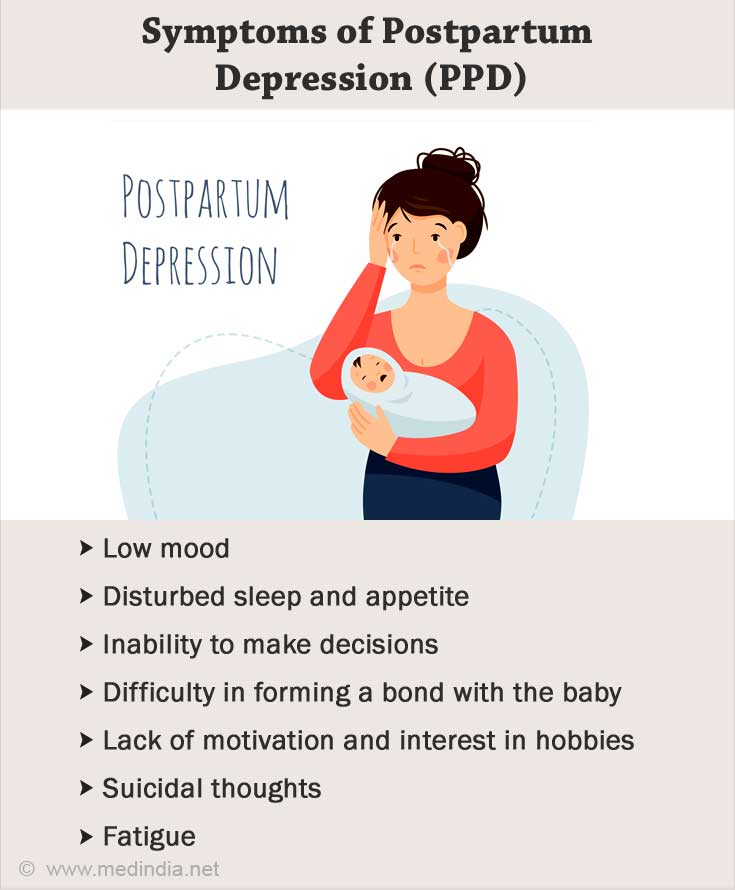
- Low mood — The individual feels sad, hopeless, and helpless. They also experience mood swings.
- Disturbed sleep and appetite — Either decreased or increased sleep and appetite are seen.
- Inability to make decisions and confusion
- Difficulty in forming a bond with the baby
- Lack of motivation and interest in hobbies
- Tendency to withdraw and isolate oneself
- Thoughts of causing harm to the baby or oneself
- Suicidal thoughts
- Fatigue
Postpartum depression may be due to the hormonal changes that happen during pregnancy in women. There is a rapid drop in hormones such as estrogen and progesterone. Other factors that play a role include social changes, marital stress, financial constraints, and other illnesses.
How Common are Postpartum Depression and Psychosis?
Postpartum depression has been found in around 1 out of 6 women and 4% men. Baby blues a less severe short-term condition is seen in 50% to 75% of women post childbirth.
Postpartum psychosis is seen in about 1to 2 out of 1,000 women. It is rare compared to postnatal depression. Despite the conditions being rare, they are very critical and have to be taken seriously.
What is the Difference between Postpartum Psychosis and Postpartum Depression?
Postpartum depression and postpartum psychosis can be differentiated in several respects.
|
Factor |
Postpartum Depression |
Postpartum Psychosis |
|
Statistics |
1 in 6 women. |
1 to 2 in 1,000 women. |
|
Onset and Duration |
Begins after 2 weeks up to 1 year after childbirth with a slow onset. |
Begins within first 2 weeks up to the first 3 months after childbirth with a dramatic onset. |
|
Main Symptoms |
Sadness, anxiety, crying, loss of interest, thoughts of harming the baby or self, isolation, suicidal thoughts. |
Delusions, hallucinations, mood lability including mania like symptoms, suspiciousness, odd behavior. |
|
Causes |
Rapid drop in hormones, prior or family history of depression or postnatal depression. |
Prior or family history of bipolar disorder or schizoaffective disorder, prior history of puerperal psychosis, sleep deprivation, giving birth for the first time. |
|
Treatment |
Antidepressants, hormone therapy, and psychotherapy such as cognitive behavioral therapy (CBT) and interpersonal psychotherapy (IPT). |
Antipsychotic medications, mood stabilizers, and inpatient hospitalization. |
|
Prognosis |
38% faced lifelong depressive symptoms. |
32% showed recurring episodes. |
What are the Risk Factors for Postpartum Psychosis and Depression?
The risk factors for postpartum psychosis are giving birth for the first time, history of schizoaffective or bipolar disorder, traumatic birth, hormonal changes, sleep deprivation, immune activation, and genetic or personal history of postpartum psychosis. Women are at a higher risk.
The risk factors for PPD are an abnormal response to hormonal changes, family history of a mood disorder, prior diagnosis of depression or PPD, young age at delivery, lack of social support, marital issues, and adverse events in the recent times. This disorder is seen more commonly among females.
How do you Treat Postpartum Psychosis and Postpartum Depression?
Treatment for postpartum depression includes:
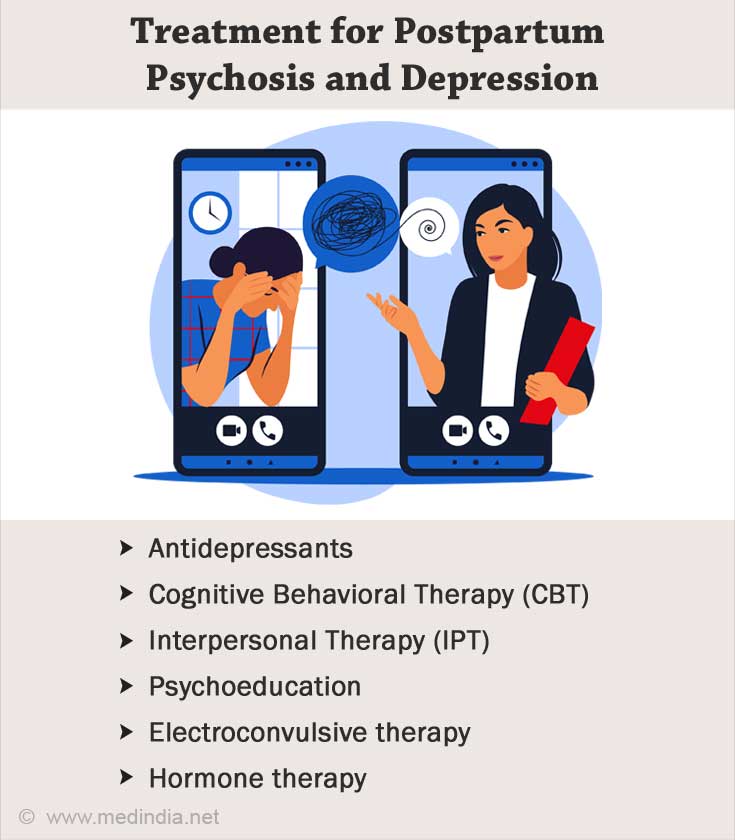
- Antidepressants such as SSRIs, medicines brexanolone, and esketamine, which are not safe to take while pregnant or feeding.
- Cognitive Behavioral Therapy (CBT) focuses on finding new ways of thinking that are more rational.
- Interpersonal Therapy (IPT) targets the link between interpersonal relationships and mood.
- Psychoeducation gives the patient and the family an idea about the illness.
- Electroconvulsive therapy is used in severe cases.
- Hormone therapy is used to replace estrogen.
Treatment for postpartum psychosis involves antipsychotics to handle delusions, hallucinations, and mania, mood stabilizers such as lithium and sodium valproate to handle mood and reduce relapse, antidepressants, electroconvulsive therapy, and inpatient hospitalization.
Tips to Cope with Postpartum Psychosis and Postpartum Depression for Patients and Family Members
Ways for the patient to cope with postpartum problems include:

- Focusing on bonding with the baby as this releases endorphin for the parent and fosters the baby’s development
- Connecting with family and friends
- Joining a support group
- Engaging in exercise, mindfulness, and getting sunlight
- Following a sleeping schedule
- Prioritizing meals with nutrition
- Engaging in hobbies and leisure activities
- Spending time with one’s partner
- Keeping a journal or mood diary
Ways for the family to cope with postpartum disorders include:
- Taking care of one’s mental health
- Recognizing boundaries and not feeling guilty
- Seeking support from close friends and family
- Reaching out to a support group
- Arranging for practical help for caregiving
- Setting aside time for oneself