- Self-Care and Self-Management Among Adolescent T2DM Patients: A Review - (https://www.frontiersin.org/articles/10.3389/fendo.2018.00489/full#B38)
- 4 Steps to Manage Your Diabetes for Life - (https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes/4-steps)
- Diabetes: An Overview - (https://my.clevelandclinic.org/health/diseases/7104-diabetes-mellitus-an-overview)
What is Diabetes Mellitus?
Diabetes mellitus (DM) is a chronic progressive metabolic disorder characterized by hyperglycemia due to impairments in insulin release, insulin actions or both.
There are three main types of diabetes:
- Type 1 diabetes - The body does not make insulin and needs to take the sugar (glucose) from the foods we eat and turn it into energy for our body.
- Type 2 diabetes - The body does not make or use insulin well. We need to take pills or insulin to help control your diabetes. It is the most common type of diabetes.
- Gestational diabetes - Some women get this kind of diabetes when they are pregnant. Though it goes away after pregnancy, they have a greater chance of getting diabetes later in life.
Diabetes mellitus was believed to be a disease occurring mainly in developed countries, but recent findings reveal a rise in number of new cases of type 2 DM in developing countries with an earlier onset and associated complications. Diabetes-associated complications can lead to chronic morbidities and mortality.
World Health Organization (WHO) estimates that more than 346 million people are affected with DM worldwide. This number is likely to double in number by 2030 without any intervention.
Need for Care
Diabetes self-care is an evolutionary process of improving knowledge or awareness in the social surroundings by figuring out how to cope with the complex nature of diabetes. It is important to have reliable and substantial measures for the self-management of diabetes because most of the day-to-day care in diabetes is handled by patients.
Taking care of diabetes can help you feel good today and in the future. When the blood sugar level is in control:
- You have more energy
- Be less tired and thirsty
- Need to pass urine often is less
- Heal better
- Have fewer skin or bladder infections
- Less chance of having health problems caused by diabetes such as heart attack or stroke; eye problems that can lead to trouble seeing or going blind; pain, tingling, or numbness in your hands and feet; kidney problems; and teeth and gum problems.
Routine Self-Care Practices
Major diabetic self-care practices include a healthy diet, being physically active, glucose monitoring, proper medication, checking cholesterol levels, taking care of kidneys and losing weight are associated with good glycaemic control, reducing long-term complication and improvement in quality of life.
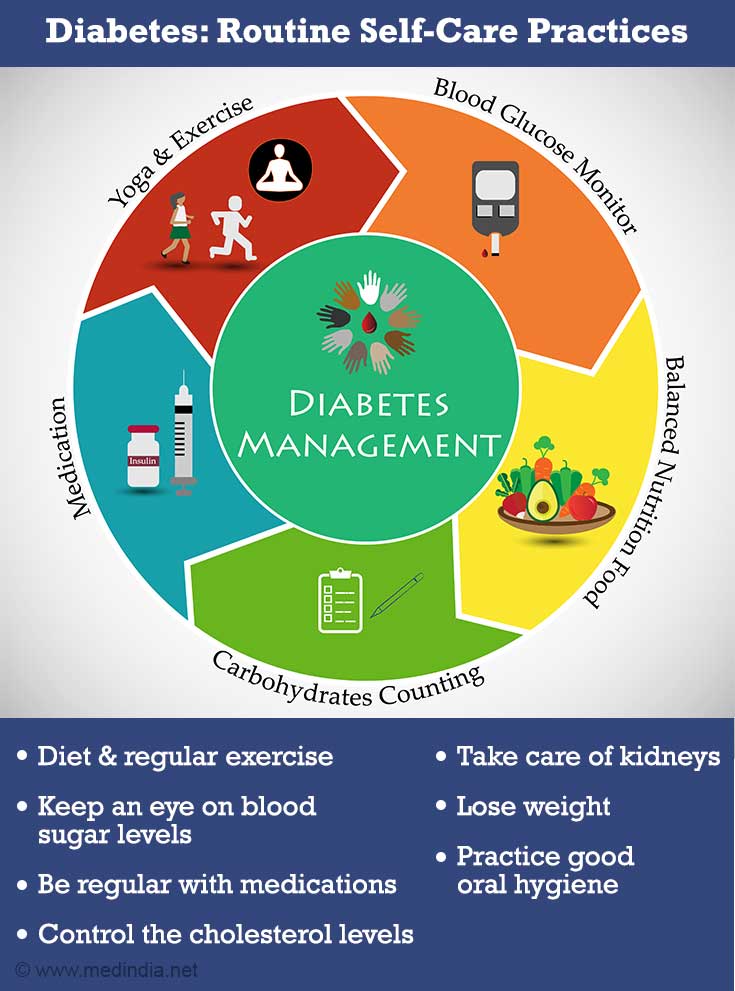
1. Diet and Regular Exercise
Dietary intervention is a vital element in the managing diabetes. Main meals interval should not be longer than four-five hours and consume some foods every 2½ to 3 hours to keep our blood glucose levels within the target range.
Include low-glycemic index (GI) foods like whole wheat, brown rice, oats, etc. in every meal and avoid refined cereal products like white bread, noodles, white rice, etc.
Diet formulated with special ingredients like complex carbohydrates, vitamins and anti-oxidants help to manage the steady release of glucose. It can be included in our breakfast, lunch or dinner as a partial meal replacement.
Exercise is the most overlooked self-care, but should be considered in relation with the drug regimen.
2. Keep an Eye on Blood Sugar Levels
Check the blood sugar levels at regular intervals at home using a glucometer.
HbA1C (Hemoglobin A1C) is a simple blood test to measure our average blood sugar levels that shows how diabetes is managed over time. It is important to get this test done either twice a year or once in three months, depending on how well your diabetes is controlled.
3. Be Regular with Medications
Adhering to the prescribed medication at the recommended amount and schedule is important for having good diabetic control. Missing medication can increase the risk of suffering from several diabetes-related health complications.
4. Control the cholesterol levels
Common complication of diabetes is known as diabetic dyslipidemia, where good cholesterol or HDL levels decrease and increase triglyceride and bad cholesterol or LDL levels. This increases the risk for heart disease and stroke. Therefore, avoid a diet high in saturated and trans fats such as fast food – burgers, pizza, fried snacks as these raise our LDL cholesterol level.
5. Take Care of Kidneys
Eat right and drink plenty of water to avoid the most serious consequences of diabetes, i.e., renal or kidney failure and chronic kidney disease (CKD).
6. Lose Weight
Obesity is the main problem for type 2 DM patients that escalates other complications. Dietary intervention and exercise are key elements for weight reduction in the management and treatment of obesity.
Set a goal to be more active most days of the week.
- Start slow - Take 10-minute walks 3 times a day
- Work twice a week to increase your muscle strength
- Use stretch bands, practice yoga, do heavy gardening (digging and planting with tools) or try push-ups
7. Practice Good Oral Hygiene
Maintaining dental health, like brushing and flossing right after eating, can minimize the effects of diabetes on gums. If gum diseases develop, they have the potential to contribute to blood glucose irregularity. Visiting a dentist twice a year can help catch early symptoms.
Support System
As there is no generally acknowledged definition for self-management, it is confused to utilize different ideas like the guidance of self-care and self-management, patient activities, and self-management education.

Self-management education conveyed as a short plea, enables the patient to recollect and have a better blend of information that enhances control of Type2 DM.
A multidisciplinary team involving educational supporters from hospitals and clinics, and the direct involvement of healthcare professionals is essential for the education program.
Self-care support system also includes family and friends to provide practical or emotional support. Family and friends play a crucial role in encouraging diabetic patients to adapt to the devastating situation, perform self-care activities and manage diabetes.
Peer and parental support can decrease the stress and encourage young people with Type2 DM to perform self-care practices and adapt according to the diabetes diagnosis.
Future
Although the diabetic management process in adolescents is almost the same as the adults, healthcare providers are usually uncertain about proper management guidelines to develop the knowledge and understanding for adolescent diabetic patients.
There are very limited experimental trials and the current guidelines for management for Type2 DM in adolescents and young adults are not fully evidence-based.
Successful outcomes have been noticed for both Type 1 and T2DM in all age groups through a supportive team that recognizes the importance of social support to encourage diabetes self-care behaviors to lessen the burden of long-term complications.