- WHO Coronavirus (COVID-19) Dashboard - (https://covid19.who.int/)
- Scientific Brief: SARS-CoV-2 Transmission - (https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html)
- Post-COVID Conditions - (https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html)
- Different COVID-19 Vaccines - (https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines.html)
- COVID-19, Stress, Vaccines, and Your Immune System - (https://www.pcf.org/c/covid-19-stress-vaccines-and-your-immune-system/)
- Symptoms of COVID-19 - (https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html)
- Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA - (https://www.thelancet.com/journals/lanpsy/article/PIIS2215-03662030462-4/fulltext)
- Stress Weakens the Immune System - (https://www.apa.org/research/action/immune)
- Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis - (https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-020-00589-w)
- The Implications of COVID-19 for Mental Health and Substance Use - (https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/)
- Managing stress during the Coronavirus (COVID-19) outbreak - (https://uichildrens.org/health-library/managing-stress-during-coronavirus-covid-19-outbreak)
- Coronavirus (COVID-19): managing stress and anxiety - (https://services.unimelb.edu.au/counsel/resources/wellbeing/coronavirus-covid-19-managing-stress-and-anxiety)
- Coping with Stress - (https://www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/index.html)
- Exercise Benefits Brain Function: The Monoamine Connection - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4061837/)
What is COVID-19?
COVID-19 the infectious respiratory illness has been doing the rounds since late 2019.
- The disease spreads from person-to-person by close-contact. Airborne transmission has also been studied as a possible means of transmission and is a possible factor in closed, poorly ventilated, crowded spaces. The growing predominance of diverse variants of COVID-19 contributes to a grave concern among millions. The aroused variants of COVID-19 include:
- Delta variant – first detected in India (most prevalent variant)
- Alpha variant – first detected in the UK
- Beta variant - first detected in South Africa
- Gamma variant – first detected in Brazil
- Lambda variant
- Mu variant
The common symptoms of COVID-19 include sore throat, fever, cough, loss of taste and smell, fatigue, muscle pain, and difficulty breathing. After recovery from the disease, people continue to face physical, mental, and neurological symptoms such as hair loss, muscle pain, fatigue, depression, anxiety, difficulty concentrating, and brain fog (dementia).
What Causes Stress during a Pandemic?
The causes of stress during COVID-19 include:
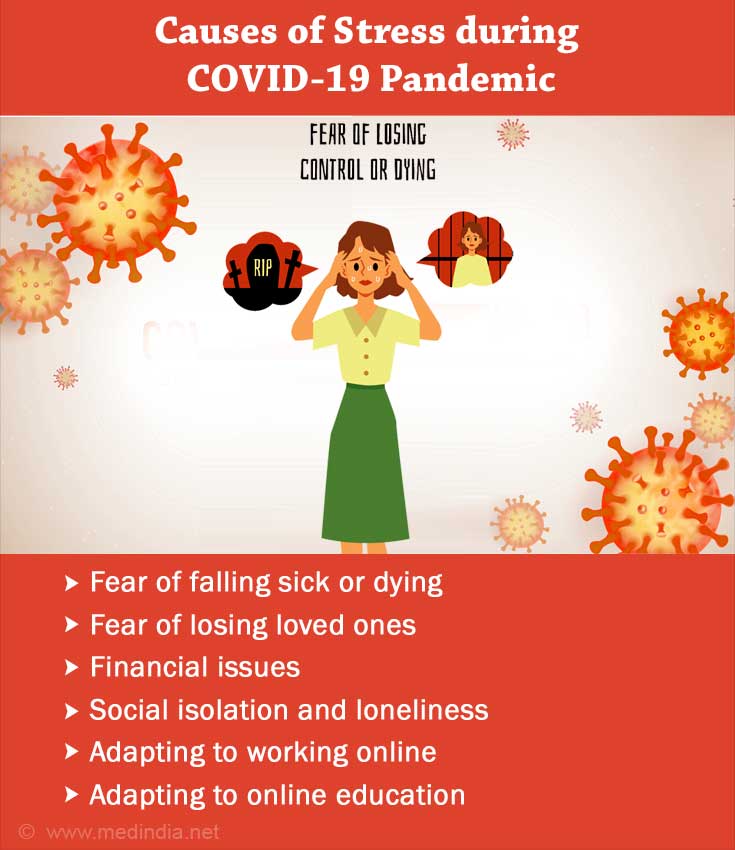
- Fear of falling sick or dying
- Fear of losing loved ones
- Financial issues
- Social isolation and loneliness
- Adapting to working online
- Adapting to online education and managing the child’s studies
- Being confined to the home with no outlets
- The uncertainty of the situation
What is the Link between Stress and COVID-19?
Research has shown that when we are stressed, our body responds by producing stress hormones such as cortisol. This in turn, leads to the release of cytokines that can cause inflammation which is implicated in other health conditions.
High levels of stress have been found to increase the risk of catching a respiratory illness. Recent data shows that high levels of cortisol are related to an increased severity of COVID-19. Hospitalized individuals with increased levels of cortisol had a higher possibility of death. Having a psychiatric illness in the past has been linked to a 65% chance of catching COVID-19.
Lack of support and loneliness (due to lockdowns) can aggravate stress which in turn hampers the immune system. Long-term stress can cause a worse impact on the immune system. Cortisol can suppress the immune system’s effectiveness in fighting off pathogens by reducing the number of lymphocytes present in the blood and interfering with normal white blood cell communication.
What are the COVID Stress Symptoms and their Implications?
Research shows that 29.6% of individuals experienced stress during the pandemic. COVID stress and anxiety have been associated with sleep issues (36%), difficulty eating (32%), worsening of long-term health issues (12%), and substance abuse (12%).
A study published in BMC Global Health Research and Policy has found that survivors of COVID-19 are more prone to post-traumatic stress disorder (PTSD).
This could be in a variety of scenarios:
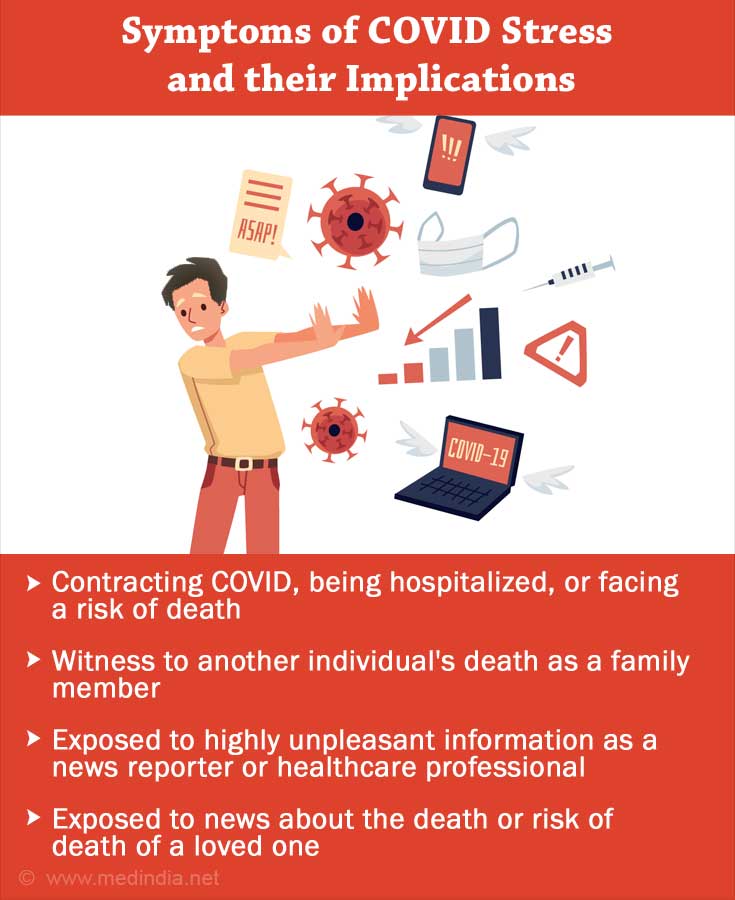
- Contracting COVID and having severe symptoms, being hospitalized, or facing a risk of death
- Being a witness to another individual's death as a family member or healthcare professional
- Being exposed to highly unpleasant information as a news reporter or healthcare professional
- Being exposed to news about the death or risk of death of a loved one
Studies show that 16.8% of nurses experienced PTSD with high symptoms of avoidance. Stress during COVID-19 quarantine is also an issue. Among home-quarantined youngsters, 12.8% displayed post-traumatic stress symptoms.
The pandemic itself has acted as a trauma for some (29.5%). Loneliness was found to be related to post-traumatic stress symptoms, depression, and anxiety.
Pregnant women also faced higher PTSD like symptoms in this period. Psychiatric patients are also at a higher risk of PTSD and other mental health issues during COVID-19, including suicidal thoughts.
Tips to Manage Stress during COVID-19
Stress is both a contributing factor and a result of COVID-19. COVID stress management involves a variety of techniques. It is important to differentiate between what is in one’s control and what isn’t, in these uncertain times. Practical steps to follow precautions can be taken.
Beyond this we need to recognize that things are not in our control. By stressing about them, we cannot change anything, and it can also worsen our immunity. 100% safety is not possible and trying to achieve it is anxiety-provoking.
It is advisable to stay connected virtually or in person if possible. This helps to have an outlet and a sense of support which is beneficial, as loneliness can contribute to stress. Staying physically active by engaging in exercise, dance or sports can also contribute to improved mood and act. Such activities release endorphins, dopamine and serotonin which help to reduce stress and improve mood.
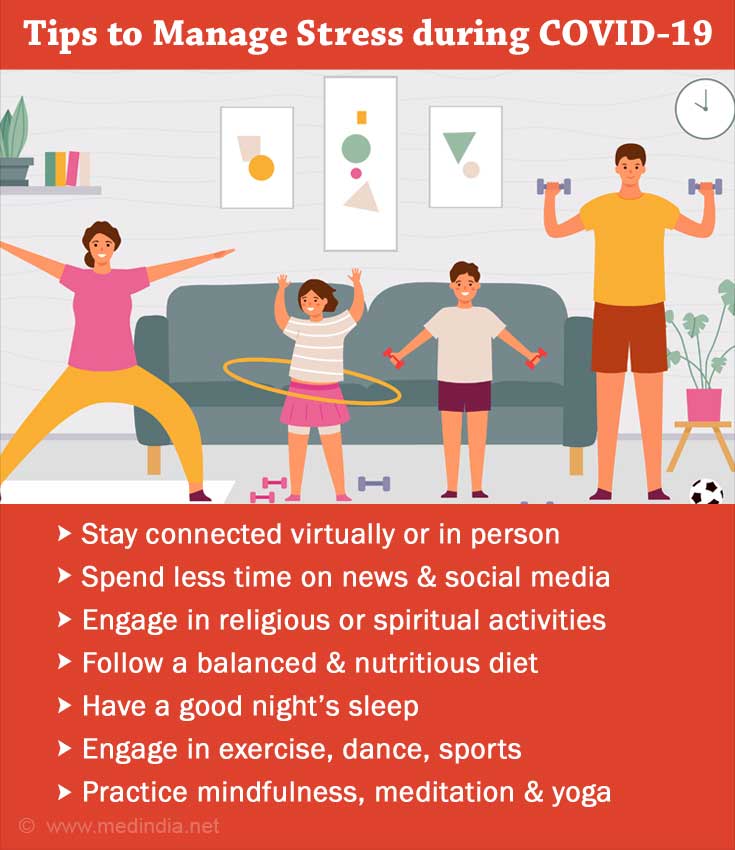
Having a schedule can also contribute to a sense of structure and control. In addition to this, limiting time on news and social media has also been found to be beneficial. Engaging in hobbies and leisure activities can act as a COVID stress buster. Mindfulness, meditation, and yoga reduce stress as well. Contributing and helping others can also give a sense of purpose and improve mood.
Maintaining a gratitude journal can help one focus more on the positive aspects of life. Religious or spiritual faith can act as a source of hope and reduce stress. Having a balanced nutritious diet, a healthy sleep schedule, and avoiding substances is also important and contributes to mental health.