We often hear of the intense pain associated with appendicitis. Appendicitis is a condition in which the appendix becomes inflamed. The pain due to this condition initially begins around the navel in most people and then disseminates from there. It has, however, been classically described to origin at the right lower quadrant of the abdomen. The pain increases as the degree of inflammation increases.
The appendix is an organ located at the end of the colon and has the shape of a finger. It can be found on the right side of the abdomen. The functional use of appendix is not known. Surgical removal of the appendix is the preferred treatment for appendicitis.
Appendicitis is frequently (70%) observed in those younger than 30 years. Males are more prone to appendicitis compared with females with a risk ratio of 1.4:1.

The first report of appendicitis was recorded in 1886 by Dr. Reginald Fitz. The condition is most often observed in Western countries and is rare in underdeveloped countries. The rate of incidence of acute appendicitis is 7%.
Appendicitis can be acute, recurrent, or chronic based on the symptoms.
Acute Appendicitis is prevalent in all age groups but is rare in infants or seniors. There is obstruction within the appendix in acute cases and is characterized by low-grade fever, mild pain in the upper abdominal region (epigastric) followed by severe pain that migrates to the lower right section of the abdomen, increased pressure within the lumen of the appendix, vomiting, anorexia, and nausea.
Chronic Appendicitis occurs at a 1% incidence rate. In chronic appendicitis, there is inflammation of the wall of the appendix and is associated with intense abdominal pain in the right lower section for approximately 3 weeks. Symptoms resolve once appendectomy is performed.
Recurrent Appendicitis occurs at a rate of 10%. As the name suggests, there are repeated bouts of severe abdominal pain due to an inflamed appendix, and this pain is resolved with an appendectomy.
Both chronic and recurrent appendicitis can be avoided if acute appendicitis is detected, diagnosed, and managed on time.
Appendicitis may also be classified as complicated and non-complicated appendicitis.
Complicated appendicitis is characterized by an abscess or ruptured appendix and gangrene. Delay in diagnosing and treating this condition can lead to fatal results and even death.
The causes of appendicitis are thought to be due to something blocking the entrance of the appendix. The blockage may be due to stool, a foreign body, a lymph node, or cancer. Infections can also lead to blockage of the appendix.
As mentioned earlier, appendicitis is associated with intense pain. This pain can begin quite suddenly around the navel and move outwards in the downward direction to the right lower section of the abdomen. The pain can be intolerable and can occur while coughing, breathing in deeply, or sneezing. The pain can manifest before the appearance of other symptoms. Migration of pain is one of the diagnostic features of appendicitis.
The other symptoms include:
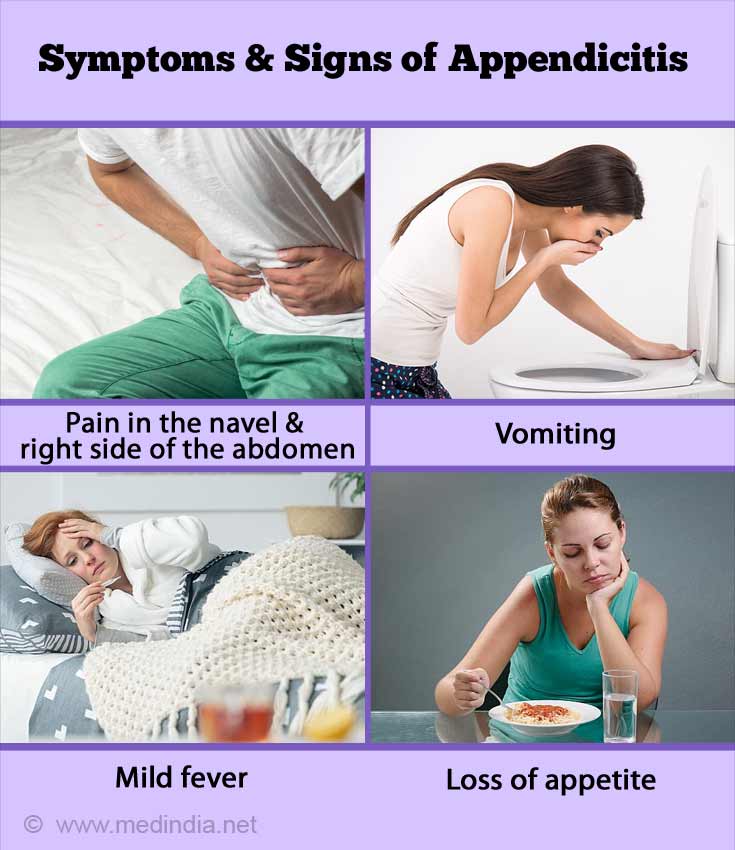
Individuals feel that letting out gas may provide relief while some are unable to let out gas. Fever and lack of an appetite are also seen in those with appendicitis. There may a high white blood cell count, and individuals usually suffer anorexia. Tenderness at the right lower part of the abdomen is an important sign of appendicitis. The usual defining symptoms of appendicitis differ in pregnant women, patients in their old age, or when the appendix is located in an unusual position.
Complicated Appendicitis
In the case of complicated appendicitis, a recent study has identified some potential risk factors of complicated appendicitis. Some of these risk factors, include:
A higher educational status places individuals at a lower risk of developing complicated appendicitis.
Appendicitis needs to be correctly and promptly diagnosed to avoid complications and possible mortality. Due to the wide range of clinical features, diagnosis can be difficult.
A fitting medical history, specific signs on physical examination and supportive imaging modalities (especially an ultrasound image) help to diagnose appendicitis. Rectal examinations are not very reliable in diagnosing appendicitis. In women, pelvic examinations are useful in confirming the diagnosis of appendicitis.
Medical History: The doctor initially takes the patient’s medical history. The doctor enquires about the details of the abdominal pain (e.g. where it is located, when it began, the observed symptoms), any other health conditions involved, and the use of any drugs or alcohol
Physical Exam: Following the medical history, the doctor carries out a physical exam by putting pressure on specific parts of the abdomen. Based on the appropriate responses, the physician can make the diagnosis of appendicitis.

Imaging Tests: These tests are performed to confirm the diagnosis of appendicitis. These tests can rule out or confirm the diagnosis of appendicitis. Any inflammation, an appendix that has burst, a block in the appendix, or any other cause of abdominal pain can be ascertained through these tests. There are different types of imaging tests that are elaborated below:
Magnetic Resonance Imaging (MRI): In brief, magnetic resonance imaging uses magnets and radio waves to provide an image. The images are analyzed by a radiologist. The technique can be performed in a hospital or as an outpatient procedure. There is no need to anesthetize a patient for the procedure. However, for those individuals with fear, a light sedative may be administered. The patient is made to lie down, and the body is moved into a tunnel that is either closed at one end or open at both ends, for imaging.
Ultrasound: Usually, this test is the first technique to be used to analyze children, pregnant women, infants, and teenagers. The technique can be performed in the clinic, a hospital, or an outpatient facility. There is no need for anesthesia. The technique utilizes sound waves to create an internal image of the organ (pelvis and abdomen) in question. A gel is applied on the abdomen, and a transducer is used to transmit sound waves that do not cause any pain. The sound waves bounce off the organ in question to provide an image. Color Doppler ultrasound is effective in detecting the blood flow through the appendix. This gives an idea of the level of obstruction within the appendix.
In women, endovaginal ultrasound is effective in detecting appendicitis. Graded compression ultrasound is effective in determining the region of inflammation with the aid of probes and pressure applied to the inflamed area of the appendix.
CT Scan: This technique can be performed in a hospital or an outpatient facility. The images are analyzed by a radiologist. The technique utilizes computer software and x-rays to develop the images. As in magnetic resonance imaging, the patient is slid into a tunnel-like apparatus that is either closed at one end or open at both ends. A mild sedative may be given to children who are scared. Pregnant women cannot go through this procedure as x-rays will harm the fetus.
Laboratory tests
Urinalysis: Abdominal pain can be due to kidney stones or a urine infection. Hence, to rule out these conditions, the patient’s urine is tested. Acetone is normally found in urine in the condition of appendicitis.
Blood Tests: Blood tests can indicate the signs of inflammation (high WBC count), imbalance in the electrolytes or fluid, or any sign of dehydration.
Pregnancy Tests: Women need to be checked to see if they are pregnant specially to avoid the use of harmful x-rays in a CT-scan.
Complicated Appendicitis
A research study has concluded that procalcitonin is a useful molecular marker to confirm the diagnosis of complicated appendicitis.
Despite the presence of numerous diagnostic techniques, the rate of misdiagnosis of appendicitis remains unchanged. According to 2 research studies, when the condition of appendicitis is not diagnosed or confirmed, it is termed as a misdiagnosis of appendicitis.
The main form of treating appendicitis is by surgically removing the appendix. The procedure known as appendectomy can be performed in 2 ways:
Laparotomy: An open surgery may be performed thro an incision in the lower area to the right of the abdomen to remove the appendix.
Laparoscopy: Laparoscopic surgeries are becoming more popular than open surgeries for appendicectomies. Smaller incisions, lesser post operative pain, faster recovery and earlier restoration of feed, and shorter duration of hospital stay are some of the benefits that laparoscopic procedures offer.
In the case of mild appendicitis, antibiotics may be administered to treat the condition. In general, antibiotics are prescribed even before surgery is carried out. If the patient heals before the surgery, then surgery is not required. In most cases (63%) appendicitis patients recover from treatment with antibiotics. In 20% of the appendicitis cases that were treated with antibiotics, there was a recurrence of appendicitis.

There are complications that arise when the appendix bursts. To tackle the complications, surgeons perform different procedures as outlined below:
When there is pus that is released due to a burst or ruptured appendix, the surgeon uses a tube to drain out the pus and treats the patient with antibiotics. Six to eight weeks later, when the infection is under control, and the pus has been removed, the surgeon removes the appendix.
In the case of peritonitis (inflammation of the peritoneum or the abdominal lining), laparotomy is done to clean the abdomen to avoid infection, and the appendix is removed.
In most cases, patients do not have complications following appendectomy. Complications include infections of the wound (most common), development of abscess, sepsis, recurring cases of appendicitis, blocked fallopian tube, inflamed lining of the abdomen.
Patients treated with antibiotics show a lower chance (39%) of complications following treatment of appendectomy.
There is no sure way to prevent appendicitis. A healthy diet that includes fresh vegetables and fruits may help to lower your risk.