- Homer MJ et al. Babesiosis. Clin. Microbiol.Rev. 2000;13(3):451-469.
- Babesiosis - (https://www.health.ny.gov/diseases/communicable/babesiosis/fact_sheet.htm)
- Babesiosis FAQs - (http://www.cdc.gov/parasites/babesiosis/gen_info/faqs.html)
- Vannier E, Gewurz BE, Krause PJ. Human Babesiosis. Infect Dis Clin North Am. 2008;22(3):469-488.
- Vannier E, Krause PJ. Babeisosis in China, an emerging threat. Lancet Infect Dis. 2014;15(2):137-139.
- Welc-Falęciak R et al. First report of two asymptomatic cases of human infection with Babesia microti (Franca, 1910) in Poland. Ann Agric Environ Med. 2015; 22(1): 51-54.
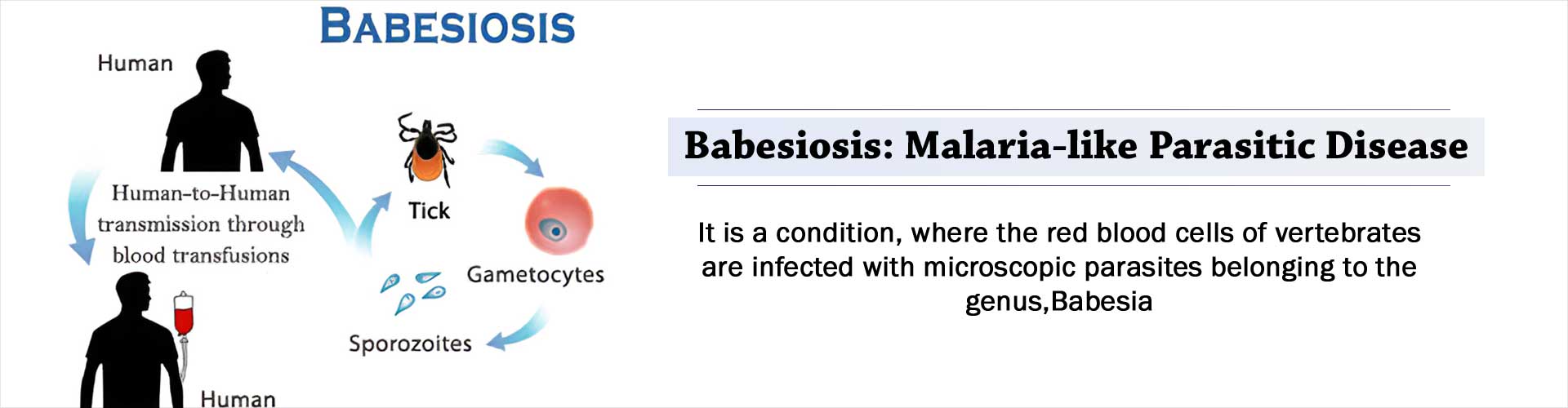
What is Babesiosis?
Babesiosis is a condition, where the red blood cells of vertebrates are infected with microscopic parasites belonging to the genus, Babesia. The parasites require a vertebrate and a non-vertebrate host to complete their life cycle. They’re transmitted to vertebrate hosts with the help of ixodid ticks that are in the nymph stage. Adult ticks may also participate in this transmission.
Babesiosis occurs in a large number of vertebrates with the number of identified Babesia species going beyond 100. Babesiosis is a zoonotic condition observed in humans and is caused by different parasites based on the region.
In Europe, the bovine parasite Babesia divergens causes a severe form of human babesiosis. In North America, the rodent (mice with white feet) parasite Babesia microti or a second species, the WA1 piroplasm, cause babesiosis in humans.
A recent study in China, identified Babesia venatorum as the cause for babesiosis in humans. There are diverse manifestations to this disease that range from an infection that goes unnoticed to malaria-type of symptoms that may result in death.
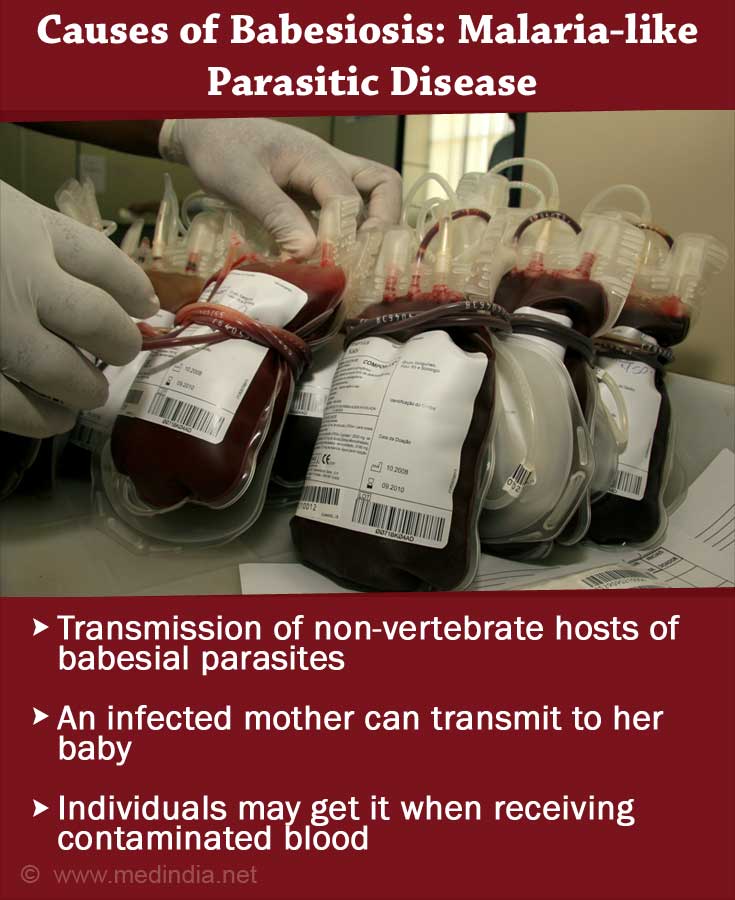
Causes of Babesiosis
- The non-vertebrate hosts of babesial parasites are ixodid ticks. The transmission occurs at the nymph stage of the ticks. In certain cases, the adult ticks may also participate in this transmission. These ticks are normally present in the warm months of spring and summer in grass, pastures, or in wooded areas. In North America, the deer ticks Ixodes scapularis transmit Babesia microti to human hosts. In China, the vector is Ixodes persulcatus for transmitting Babesia venatorum. In Europe, Ixodes ricinus ticks transmit babesial parasites.
- An infected mother can transmit babesial parasites to her unborn child during pregnancy.
- Individuals may also get infected with babesiosis when receiving contaminated blood.
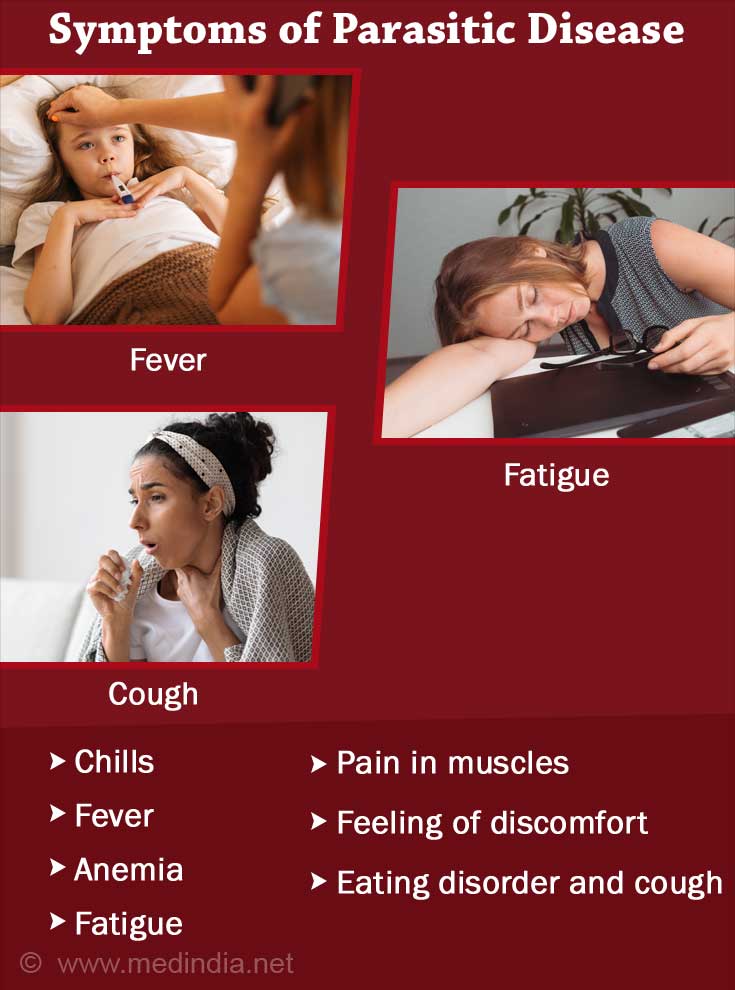
Symptoms of Babesiosis
In general, individuals affected by the babesial parasites do not show any major symptoms and feel fine. Such individuals may remain carriers for a period ranging from a few weeks to months, and even years. The symptoms of babesiosis manifest themselves on the basis of the life cycle of the parasite in the human red blood cells. The parasite’s life cycle ranges from one to six weeks or may last until three months. This is the incubation period of the parasite. When the parasites break out of the red blood cells, certain individuals demonstrate visible symptoms in the mild to moderate range as outlined below:
- Chills
- Fever
- Hemolytic anemia
- Fatigue
- Myalgia
- Malaise
- Anorexia
- Cough
Serious cases of parasite infection can result in nausea, night sweats, acute failure of the respiratory system, splenomegaly, congestive failure of the heart, and hepatomegaly. Immunocompromised individuals (lymphoma, AIDS, cancer) and the elderly suffer severe symptoms.
Splenectomized individuals suffer from jaundice, pulmonary edema, renal and liver failure. Leukopenia and thrombocytopenia are other manifestations of this condition.
Diagnosis of Babesiosis
The diagnosis of babesiosis may be classified into 2 categories:
- Laboratory tests: Babesial infection is confirmed by identifying the babesial parasites when a blood smear is stained. Immunological identification is another way of confirming the diagnosis of babesiosis. IgG and IgM antibodies against babesial parasites may be identified through an indirect immunofluorescence assay. If the titer shows up as ³1:1024, there is an active infection. If the titer is £1:64, there is no infection. In the event that the laboratory tests fail to confirm a babesial infection despite a strong suspicion, the patient’s blood is injected into hamsters. Hamsters are highly sensitive to infection with babesial parasites. Hence, when parasitemia develops in hamsters, babesial infection can be confirmed in humans. PCR testing is more sensitive than hamster testing, since it can identify low concentrations of babesial species in the blood. It is recommended to perform this test along with an immunological test due to the possibility of false positives in the PCR results.
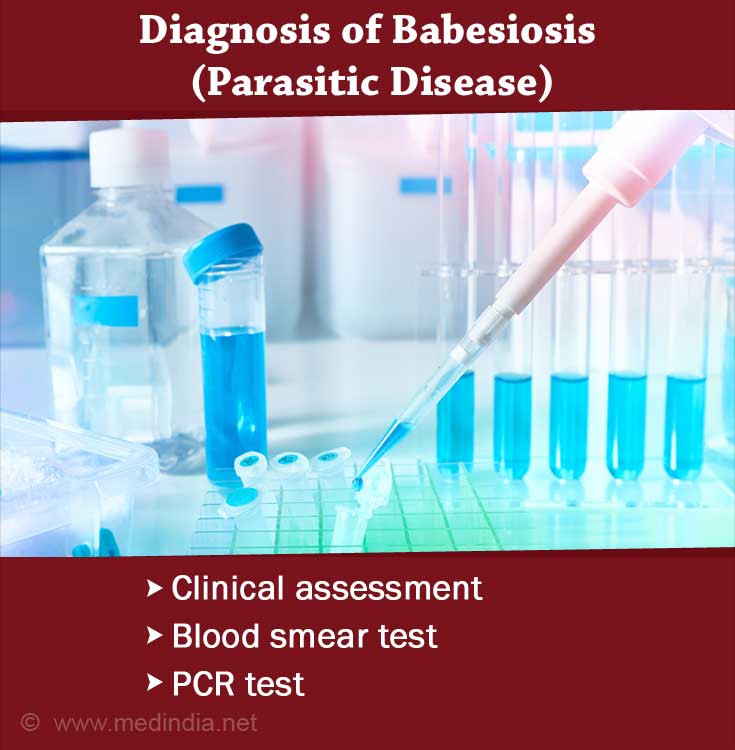
- Clinical assessment: There are no specific overt symptoms for babesiosis. Many of the symptoms are similar to those of other conditions. If the patient displays viral fever-associated symptoms following a blood transfusion, the individual needs to be assessed for babesiosis. Another way of identifying the condition is to compare the symptoms with recent activities of the patient. If the patient has spent time in outdoor activities in areas infested with babesial parasites, specially in the spring or the summer, then the chance of babesiosis is high.
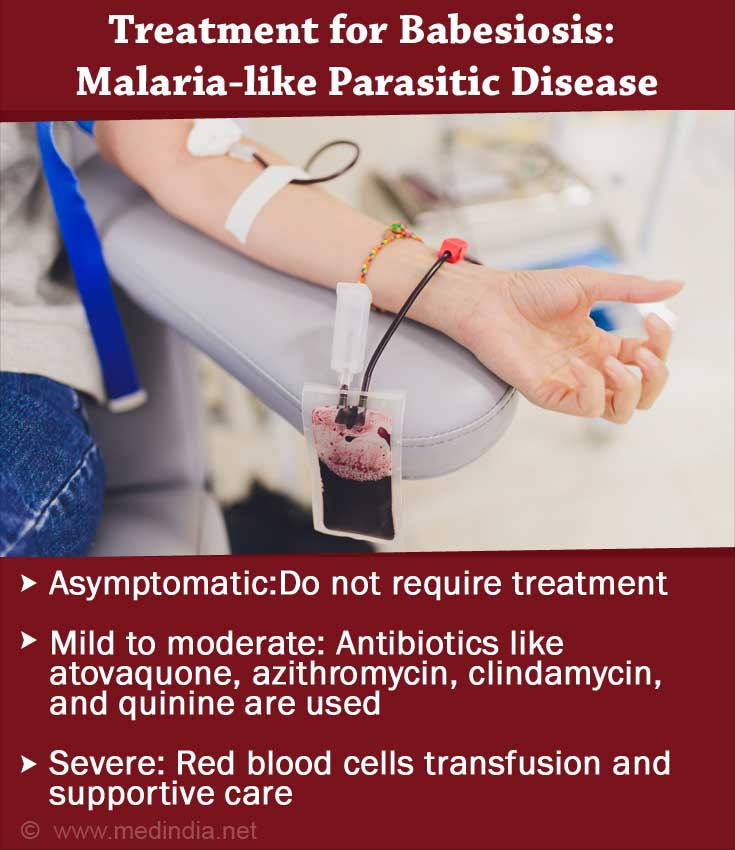
Treatment for Babesiosis
Treatment of individuals with babesiosis is dependent on the severity of the infection.
Asymptomatic: When the infection is asymptomatic, despite positive blood smears, treatment is not recommended. If the infection continues for more than three months, then treatment is provided. When there is parasitemia in immunocompromised patients, regular blood smears are recommended until the infection resolves on its own. If the immunological tests are positive but the blood smears are negative, regular monitoring of the blood is recommended.
Mild to moderate: Clindamycin and quinine are given in combination to treat the symptoms of babesiosis. However, this combination of drugs leads to severe side effects. Patients with gasteroenteritis and tinnitus are unable to tolerate this drug regimen. Azithromycin and atovaquone are milder and administered for 7 to 10 days to treat mild to moderate babesial infections. These drugs may be used in children.
Severe: In order to treat severe cases of babesial infections, quinine and clindamycin may be administered for seven to 10 days. Red blood cell transfusion is also recommended to dilute the toxic products of babesial infections or to treat renal and liver failure. Patients, who do not have a robust immune system are prone to babesial infections. Use of IFN-g to treat individuals with a compromised T-cell response, is being analyzed.