- Choriocarcinoma - (https://www.nlm.nih.gov/medlineplus/ency/article/001496.htm)
- Desai NR, Gupta S, Said R, et al. Choriocarcinoma in a 73-year-old woman: a case report and review of the literature. J Med Case Rep. 2010;4:379.
- LIU H, XIAO Y-D, PENG S-P, ZHOU S-K, LIU J. Pituitary metastasis of choriocarcinoma: A case report. Oncology Letters. 2016;11(2):1517-1520. doi:10.3892/ol.2016.4088.
- LI X-M, LIU X-Y, LIU Z-X. Choriocarcinoma with multiple lung, skull and skin metastases in a postmenopausal female: A case report. Oncology Letters. 2015;10(6):3837-3839. doi:10.3892/ol.2015.3750.
- Gestational Trophoblastic Disease Treatment (PDQ®)–Patient Version - - (http://www.cancer.gov/types/gestational-trophoblastic/patient/gtd-treatment-pdq)
- Goldstein DP, Berkowitz RS, Horowitz NS. Diagnosis and Management of Gestational Trophoblastic Neoplasia. In: de Mello AR, Tavares Ã, Mountzios G, eds. International Manual of Oncology Practice: (iMOP) - Principles of Medical Oncology. Cham: Springer International Publishing; 2015:501-517.
- Mohd Faizal, A., et al. "A Pure Nongestational Choriocarcinoma of Ovary: Sharing Experience in Sabah." Journal of Surgical Academia 5.1 (2015): 51-53.
- Seckl MJ, Sebire NJ, Fisher RA, et al. Gestational trophoblastic disease: ESMO clinical practice guidelines for diagnosis, treatment and follow-up.Ann Oncol (2013) 24 (suppl 6): vi39-vi50. doi: 10.1093/annonc/mdt345
- Stevens FT, Katzorke N, Tempfer C, et al. Gestational Trophoblastic Disorders: An Update in 2015. Geburtshilfe und Frauenheilkunde. 2015;75(10):1043-1050. doi:10.1055/s-0035-1558054.
- Rao KVLN, Konar S, Gangadharan J, Vikas V, Sampath S. A pure non-gestational ovarian choriocarcinoma with delayed solitary brain metastases: Case report and review of the literature. Journal of Neurosciences in Rural Practice. 2015;6(4):578-581. doi:10.4103/0976-3147.169869.
- Cyriac S, Sagar TG, Mahajan V. Choriocarcinoma with arterial and venous thrombosis. Neurol Ind. 2009;57(4):505-507.
What is Choriocarcinoma in Females?
Choriocarcinoma is a rare, rapid or fast-growing form of malignant cancer that occurs in the female uterus following impregnation. The tumor cells develop from cells that later should develop into the placenta.
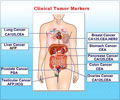
Choriocarcinoma is a type of gestational trophoblastic disease (GTD). Gestational trophoblastic diseases can be benign (hydatidiform moles or HM) and localized to the site of tumor development, or malignant (gestational trophoblastic neoplasia - GTN) and spread to other regions of the body. Choriocarcinoma is a malignant type of gestational trophoblastic disease. It can spread to other regions of the body, such as lungs, kidneys, vagina, liver, pelvis, intestines, brain, and pituitary gland, among others, through blood vessels (hematogenous spread).
Since choriocarcinoma occurs most often as a result of pregnancy, it is called gestational choriocarcinoma. There are non-gestational choriocarcinomas, that is, cancers that arise in non-pregnant females, as well. The cancers give rise to features similar to choriocarcinoma. Non-gestational ovarian choriocarcinoma is observed in pre-pubertal girls. It is rare for choriocarcinoma to develop following menopause although a case has been reported with metastases to the lymph nodes, skull, neck, and lungs.
What are the Causes of Choriocarcinoma in Females?
Gestational choriocarcinoma usually arises in women who have experienced one of the following conditions:
- Miscarriage (25%)
- Pregnancy in the fallopian tubes, or other locations beside the uterus (referred to as ectopic pregnancy)
- Normal pregnancy (22.5%)
- Following a hydatidiform mole
Note: What is a hydatidiform mole? It is another term for molar pregnancy. A tumor develops slowly in the cells form the placenta. It is the placenta that nourishes the fetus during pregnancy. The hydatidiform mole contains small sacs or cysts that are localized and benign. Sometimes, the hydatidiform mole spreads to surrounding tissues and becomes malignant, resulting in choriocarcinoma.
What are the Symptoms and Signs of Choriocarcinoma in Females?
The cells of the choriocarcinoma produce the hormone human chorionic gonadotrophin (hCG). The major symptom is irregular bleeding from the vagina following the occurrence of a hydatidiform mole or pregnancy. However, it can even occur after months or many years following pregnancy, making diagnosis difficult. The condition is also associated with very painful menstruation or cramps in the abdomen, also called dysmenorrhea. Coughing of blood or nausea tends to occur once the tumor has spread to other sites.
How to Diagnose Choriocarcinoma in Females?
Diagnosis of choriocarcinoma is made based on the history of the patient and certain tests. The levels of the hormone human chorionic gonadotrophin (hCG) are high in the blood of women with choriocarcinoma. It is important to measure hCG levels in women who develop metastasis in their child-bearing age. If the hCG levels are high and choriocarcinoma is suspected due to an earlier pregnancy, then other tests are conducted.
A lumbar puncture is performed to calculate the ratio of the hCG levels of cerebrospinal fluid to those of serum hCG. If the value exceeds 1:60, then there is a possibility of a central nervous system involvement.
Magnetic resonance imaging of the pelvis and brain; contrast enhanced computed tomography of the abdomen and chest; and a Doppler ultrasound are some of the other diagnostic techniques used for choriocarcinoma. The pelvic ultrasound gives an idea of the vascular condition (the number of blood vessels) and the extent of the choriocarcinoma.
One must be cautious while taking a biopsy of the choriocarcinoma due to the high chance of bleeding, as such tumors are high in blood vessels. When the biopsy is available, it provides useful tissue-specific and genetic information, which helps in conclusive diagnosis. In the genetic analysis, you will be able to understand the type of pregnancy that caused choriocarcinoma. For example, in the case of a partial hydatidiform mole or a term pregnancy, there is a mix of both paternal and maternal chromosomes. However, in the case of a complete hydatidiform mole, the pregnancy is due to only chromosomes from the father. In non-gestational ovarian tumors, a DNA polymorphism test is useful in differentiating them from gestational tumors.
How Do You Treat Choriocarcinoma in Females?
FIGO Scoring system
Physicians use the FIGO (International Federation of Gynecology and Obstetrics) scoring system to determine if choriocarcinoma patients can be treated with a single chemotherapeutic drug, such as actinomycin D (ActD) or methotrexate (MTX). A score greater than 7 indicates resistance to treatment. A score between 0 and 6 indicates low chances of treatment resistance. The scoring system is based on the number of metastases, the size of the tumor, the location of the metastatic tumor, the level of hCG, the duration of the condition following previous pregnancy, earlier resistance to chemotherapy, type of previous pregnancy and age of the woman.
Treatment of choriocarcinoma with a score of 0-6
In patients with low risk of treatment resistance and with a score in the range of 0-6, single drug chemotherapy is administered. Methotrexate is a commonly used drug. The regimen followed in the treatment of low risk patients involves:
Intramuscular administration of 50 mg methotrexate on days 1, 3, 5, 7. Thirty hours after administering methotrexate, 15 mg of folinic acid is given orally to nullify the side effects (inflammation of lung lining, ulcers in the mouth) of methotrexate.
When the hCG levels are below 300 IU/l, and if the patients are resistant to methotrexate, actinomycin is administered. After the first chemotherapy cycle, 2 to 3 consolidation cycles are repeated to prevent the relapse of the condition. The hCG levels return to normal following the first chemotherapy cycle.
Treatment of choriocarcinoma with a score of 7 or more
Combination chemotherapy is used to treat high-risk patients with a FIGO score of 7 or more. The main drug combination used to treat high-risk disease is methotrexate D, etoposide, and actinomycin D (ActD) and alternates with a combination of vincristine and cyclophosphamide (EMA-CO). The EMA-CO regimen should be administered 2 to 3 times to prevent a relapse. Approximately, 30% to 40% of the patients may continue to progress or show relapse. Such patients require platinum-based chemotherapy. Additionally, When the cancer spreads to the brain, the organ is treated either with combination chemotherapy, radiation, or with intrathecal chemotherapy. Intrathecal chemotherapy is where the drug is administered into the membrane lining the brain and spinal cord.
Recurrent tumors that may be resistant are treated with either chemotherapy, combination therapy when the tumors are resistant to single drug chemotherapy, or surgery to remove the chemotherapy-resistant tumor.
Prevention of Choriocarcinoma in Females
The hCG levels should be monitored frequently in the first year following chemotherapy since the risk of relapse is ~3%. Women should avoid getting pregnant during this period.
Following choriocarcinoma, fertility is not affected. The chances of developing congenital abnormalities in future babies are not increased.
Health Tips
The patient is advised not to get pregnant during the one-year period of chemotherapy.