- Hepatocellular carcinoma: a global view - (http://www.nature.com/nrgastro/journal/v7/n8/full/nrgastro.2010.100.html)
- Liver Transplantation for the Treatment of Small Hepatocellular Carcinomas in Patients with Cirrhosis - (http://www.nejm.org/doi/full/10.1056/nejm199603143341104)
- Sorafenib in Advanced Hepatocellular Carcinoma - (http://www.nejm.org/doi/full/10.1056/nejmoa0708857)
About
Current treatments for
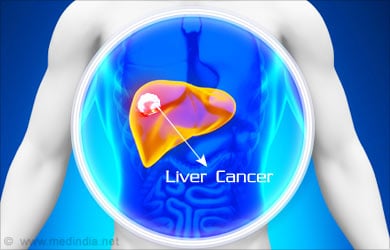
The major curative treatment for liver cancer is liver transpantation, but this is only possible when the tumor is not too large, has not spread outside the liver or into its major blood vessels, and when the underlying liver function is relatively intact. Since the majority of cases are detected too late, only 20% of all liver cancer cases can potentially be cured.
Causes of Liver Cancer
Like most cancers, there is no definitive “cause” of liver cancer. Rather, a combination of certain environmental risk factors and genetic predisposition can ultimately lead to cancer development.
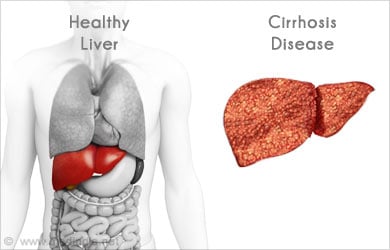
For example, any disease that results in cirrhosis, for example, viral hepatitis, alcoholism, fatty liver disease, autoimmune biliary disease, etc., increases one’s chances of developing a liver cancer. Certain liver diseases, such as hepatitis B or C, hemachromatosis, and fatty liver disease, are particularly prone towards causing liver cancer because of chronic inflammatory states and oncogenic properties of certain viral proteins.
Liver cancer can also occur in the absence of cirrhosis, especially in the case of chronic hepatitis B or C virus infection, or exposure to toxins such as aflotoxin or vinyl chloride. Other risk factors include obesity, diabetes, and smoking.
Symptoms of Liver Cancer
Early liver cancers are usually asymptomatic. In fact, liver tumors can become significantly large and still go unnoticed. The most common presenting symptom, if present at all, is right upper quadrant pain or dull ache.
If the patient has underlying liver disease, then symptoms of cirrhosis and portal hypertension will be apparent: jaundice, abdominal fluid accumulation, malaise, dark urine, clay colored stools, nausea, and confusion—just to name a few.
Diagnosis of Liver Cancer
Liver cancer is primarily diagnosed with imaging techniques. While an ultrasound can show masses within the liver and is a good screening test in combination with checking the serum alpha fetoprotein (AFP) level, CT and MRI provide definitive diagnoses. Biopsy of a liver tumor is usually deferred if the patient has underlying liver disease and the tumor displays classic characteristics using standard CT and MRI imaging techniques. This is because liver biopsy is invasive and carries complication risks (i.e., bleeding), especially in the cirrhotic patient with a deficiency of clotting factors and a low patelet count. Also, histopathologic examination of a liver biopsy does not help to direct specific therapies (at least not at this time), so if the tumor looks like a liver cancer and the patient has known liver disease, it is safer to accept the diagnosis and proceed with treatment. If there is any uncertainty in the diagnosis based on imaging, then a biopsy needs to be performed.

The serum AFP level can be elevated in patients with liver cancer, but only in about 60% of cases. Also, the absolute AFP level does not correlate with the extent of disease. AFP is therefore helpful as a screening tool and as a post-treatment test to detect cancer recurrence (only if the AFP level was elevated prior to treatment).
Upon diagnosis of a liver cancer, it is important to rule out spread of the cancer before proceeding with treatment. The three most common places for a liver cancer to spread are lung, bone, and brain. A lung CT should always be ordered and bone scans or head CTs are usually reserved for patients with symptoms suggesting bone or brain involvement.
Treatment of Liver Cancer
There is a vast array of treatment options for liver cancer, including surgical resection, arterial injections of chemotherapy (TACE or transarterial chemoembolization) or radioactive beads (TARE or transarterial radioembolization) into the tumor, radiofrequency ablation (RFA), irreversible electroporation (IRE), and microwave ablation, chemotherapy, radiation, and
Surgical resection, when performed on patients whose underlying cirrhosis is not too severe, results in 5-year survival rates of up to 80%, but unfortunately, the tumor recurrence rate is over 50% and recurrent liver cancers are invariably fatal. Liver transplantation, however, results in 80% 5-year survival rates and only 15-20% tumor recurrence rates (because the diseased liver predisposed to forming tumors is entirely removed). Liver transplant should only be attempted in patients with small cancers that have not spread outside of the liver or into the liver’s major blood vessels, otherwise the success rates fall dramatically.

Minimally invasive techniques such as TACE (transarterial chemoembolization), TARE (transarterial radioembolization), and RFA (radiofrequency ablation) are generally not considered to be curative, but can greatly prolong survival and rarely even result in complete cure. These procedures are especially helpful in keeping a tumor from growing while patients are awaiting liver transplant.
Chemotherapy and external beam radiation are currently ineffective in curing liver cancer, but promising new drugs are emerging and improved results with radiation are being reported. Sorafanib is an oral chemotherapeutic that inhibits angiogenesis (blood vessel formation) and is widely used to treat liver cancer. It is not curative, but second generation chemotherapeutics promise to be more effective.








