- Vulvodynia - (https://pubmed.ncbi.nlm.nih.gov/32355269/)
- Vulvar vestibulitis syndrome: a critical review - (https://pubmed.ncbi.nlm.nih.gov/9084950/)
- Cytolytic vaginosis: a common cause of cyclic vulvovaginitis - (https://pubmed.ncbi.nlm.nih.gov/1472886/)
- Vestibulodynia - a subset of vulvar vestibulitis or a novel syndrome? - (https://pubmed.ncbi.nlm.nih.gov/9423748/)
- Aetiology, diagnosis, and clinical management of vulvodynia - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7258372/)
- Menstrual Cycle Characteristics and Vulvodynia - (https://pubmed.ncbi.nlm.nih.gov/35041490/)
- Provoked vestibulodynia: current perspectives - (https://pubmed.ncbi.nlm.nih.gov/28979166/)
- Vulvodynia - (https://www.ncbi.nlm.nih.gov/books/NBK430792/)
- Vulvodynia: a dermatologist's perspective with emphasis on an irritant contact dermatitis component - (https://pubmed.ncbi.nlm.nih.gov/10883949/)
- Vulvodynia: case report and review of literature - (https://pubmed.ncbi.nlm.nih.gov/17998784/)
- Chronic Vulvar and Gynecologic Pain: Prevalence and Characteristics in a Self-Reported Survey - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1388073/)
- Vulvodynia: a consideration of clinical and methodological research challenges and recommended solutions - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5640408/)
- A Population-Based Study of Pregnancy and Delivery Characteristics Among Women with Vulvodynia - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4107863/)
- Generalized unprovoked vulvodynia; A retrospective study on the efficacy of treatment with amitriptyline, gabapentin or pregabalin - (https://pubmed.ncbi.nlm.nih.gov/29202395/)
- [Use of transcutaneous electrical stimulation and biofeedback for the treatment of vulvodynia (vulvar vestibular syndrome): result of 3 years of experience] - (https://pubmed.ncbi.nlm.nih.gov/18981976/)
- Measuring Treatment Outcomes in Women With Vulvodynia - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3140924/)
- Effect of Vestibulectomy for Intractable Vulvodynia - (https://pubmed.ncbi.nlm.nih.gov/27568225/)
- New topical treatment of vulvodynia based on the pathogenetic role of cross talk between nociceptors, immunocompetent cells, and epithelial cells - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5055105/)
- Safety and efficacy of topical nitroglycerin for treatment of vulvar pain in women with vulvodynia: a pilot study - (https://pubmed.ncbi.nlm.nih.gov/12192883/)
- Vulvodynia - Diagnosis & Treatment - (https://www.mayoclinic.org/diseases-conditions/vulvodynia/diagnosis-treatment/drc-20353427)
About
Vulvodynia can affect women of any age group, including girls in their teens. Estimates reveal that a total of up to six million women of all races may be suffering from this condition. The signs and symptoms occur suddenly and may last for months or a few years.
Vulvodynia affects the vulva, the external genitalia in females, which include the labia, clitoris, and the opening of the vagina. Individuals suffering from vulvodynia may experience pain, burning, or irritation, which makes them extremely uncomfortable while having sex or while having to sit for long periods of time(1✔ ✔Trusted Source
Vulvodynia
Go to source).
The condition can be divided into two subtypes-
- Generalized vulvodynia is pain occurring in different areas of the vulva at different times. It may be constant or recurrent and may be worsened upon application of pressure or even touch.
- Vulvar vestibulitis syndrome is characterized by pain or a burning sensation localized to the vestibule, which is the entrance to the vagina. This pain is most likely to occur during intercourse(2✔ ✔Trusted Source
Vulvar vestibulitis syndrome: a critical review
Go to source).
Women experiencing vulvodynia may find it difficult to discuss the problem and are often embarrassed by their condition. Although a proper diagnosis may not come about, women must seek medical help for the condition as good treatment options are available to reduce the symptoms and alleviate the discomfort associated with vulvodynia.
Cytolytic vaginosis(3✔ ✔Trusted Source
Cytolytic vaginosis: a common cause of cyclic vulvovaginitis
Go to source) (CV) infection is a little recognized but common cause of cyclic vulvovaginal complaints in women of reproductive age. Cyclic vulvovaginitis is a descriptive term referring to recurrent burning and itching of the vulva and/or vagina that recurs at the same phase of the menstrual cycle. Vaginal discharge can be minimal in cyclic vulvovaginitis.
Vestibulodynia is a unique syndrome in that it affects women who are older than those who have vestibulitis alone, and it is associated with
Vestibulodynia - a subset of vulvar vestibulitis or a novel syndrome?
Go to source).
The vulvar pain may be caused by a specific disease or may be idiopathic. Idiopathic vulvar pain is classified as vulvodynia(5✔ ✔Trusted Source
Aetiology, diagnosis, and clinical management of vulvodynia
Go to source).
The menstrual cycle may influence vulvodynia through hormonal pathways or vulvar irritation due to menstruation or menstrual hygiene(6✔ ✔Trusted Source
Menstrual Cycle Characteristics and Vulvodynia
Go to source).
Provoked vestibulodynia (PVD) refers to vulvar pain of at least 3 months duration, localized to the vestibule, provoked by touch and sexual activity and occurring in the absence of a clear identifiable cause. The clinical spectrum ranges from mild with distressing discomfort through to severe and disabling pain(7✔ ✔Trusted Source
Provoked vestibulodynia: current perspectives
Go to source).
What are the Causes of Vulvodynia?
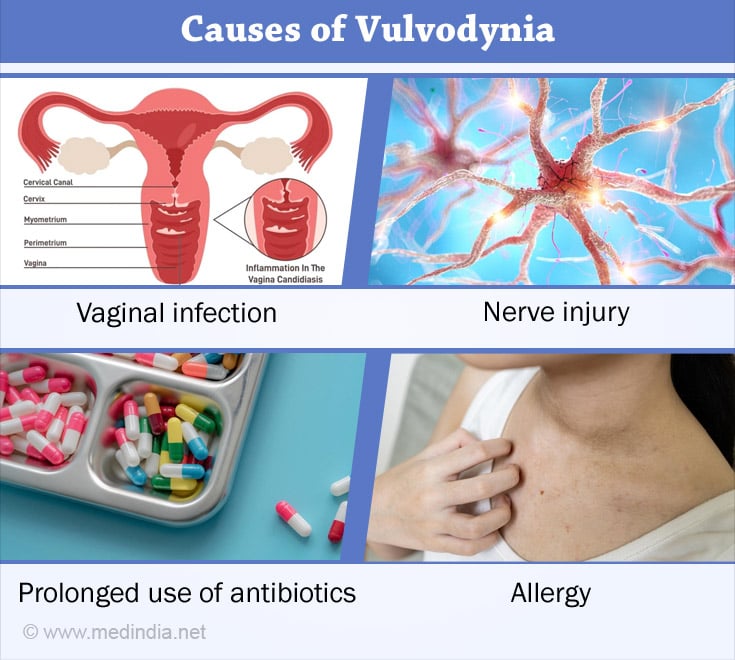
The exact cause of vulvodynia is not known. Possible causes include-
- Injury / irritation of the nerves around the vulvar region
- History of vaginal infections and the abnormal reaction of the vulvular cells to those infections
- Genetic factors contributing to the abnormal reaction of vulvular cells to inflammation
- Allergies / localized hypersensitivity of skin to chemical substances
- Muscle spasms
- Frequent use of antibiotics
- Hormonal changes
Those experiencing the disease must find it reassuring that vulvodynia is not a sign of cancer, neither is it a sexually transmitted condition.
Many women who experience vulvodynia have a history of recurrent vaginitis or vaginal yeast infections and of being treated for the same. Some even have a history of sexual abuse. But for majority of sufferers, no cause is known, although a lot of research is being done to find out the causes(8✔ ✔Trusted Source
Vulvodynia
Go to source).
What are the Symptoms and Signs of Vulvodynia?
Vulvodynia may occur in a specific region of the vulva or all over. The pain may be felt all the time or on occasions such as exercising, walking, bicycling, inserting tampons or during intercourse. It may be experienced while at rest too. Vulvodynia (vulvar burning and itching) is a symptom complex with a number of potential triggering/exacerbating factors(9✔ ✔Trusted Source
Vulvodynia: a dermatologist's perspective with emphasis on an irritant contact dermatitis component
Go to source).
In most women, burning pain, stabbing vulvar pain are the most common symptoms of vulvodynia. Many describe the pain as sharp as a knife stab, while some liken it to acid being poured on the skin. Sometimes the vulva looks swollen and inflamed too.
Other symptoms include(10✔ ✔Trusted Source
Vulvodynia: case report and review of literature
Go to source) -
- Itching
- Rawness
- Stinging
- Soreness
- Throbbing
Although the vulva usually appears normal, it may look a bit inflamed or swollen in some people.
Chronic vulvar pain characterized by sensations of stinging, burning, and rawness has been termed vulvodynia(11✔ ✔Trusted Source
Chronic Vulvar and Gynecologic Pain: Prevalence and Characteristics in a Self-Reported Survey
Go to source).
Complications of Vulvodynia
Vulvodynia can be frustrating and embarrassing to those experiencing the condition and therefore it can impair a person’s ability to work, exercise, have sex or socialize. This can lead to emotional problems like(12✔ ✔Trusted Source
Vulvodynia: a consideration of clinical and methodological research challenges and recommended solutions
Go to source) -
Anxiety /depression - Sleep disturbances
- Fear of having sex leading to muscle spasms around the vagina (vaginismus)
- Sexual dysfunction
- Relationship issues
- Altered body image
- Reduced quality of life
Women with vulvodynia may be as likely as other women to carry their pregnancy to birth; however, they may experience higher rates of Cesarean section delivery and could reflect a selection towards those women with vulvodynia who have inconsistent pain(13✔ ✔Trusted Source
A Population-Based Study of Pregnancy and Delivery Characteristics Among Women with Vulvodynia
Go to source).
It is important for these women to find a gynecologist who is willing to understand their issue and find a solution for it.
Diagnosis and Treatment of Vulvodynia
Prior to a physical exam, the doctor is likely to ask you several questions to understand your medical history. The doctor is likely to do a pelvic exam which consists of physically examining the vaginal area for infection or inflammation. Even if symptoms are visibly absent, the doctor might take a swab of cells from the vagina to be examined microscopically for yeast or bacterial infections.
A cotton swab test, carried out gently using a moistened cotton swab, might help in identifying localized areas of pain in the vulvar region(1✔ ✔Trusted Source
Vulvodynia
Go to source).
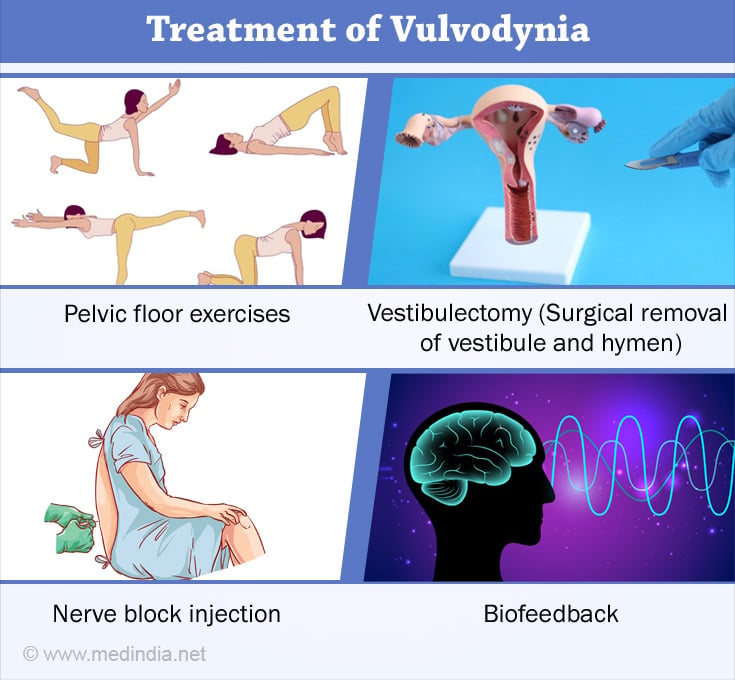
Vulvodynia treatment mostly concentrates on alleviating pain and other symptoms. Some of the options include -
- Medications - Tricyclic antidepressants or anticonvulsants may be administered to control chronic pain while antihistamines may reduce itching. Medications, such as lidocaine ointment, if applied 30 minutes before sexual intercourse, can reduce your discomfort and provide a temporary relief. However, your partner might experience numbness, temporarily, after sexual contact. Amitriptyline, gabapentin and pregabalin produced long lasting pain relief in most of the women with generalized unprovoked vulvodynia (GUV)(14✔ ✔Trusted Source
Generalized unprovoked vulvodynia; A retrospective study on the efficacy of treatment with amitriptyline, gabapentin or pregabalin
Go to source). - Biofeedback therapy - In those with vulvodynia, the pelvic muscles contract in anticipation of pain and this can result in chronic pain. Biofeedback therapy helps the person to relax, especially the pelvic muscles, and to control specific body responses, thereby decreasing pain(15✔ ✔Trusted Source
[Use of transcutaneous electrical stimulation and biofeedback for the treatment of vulvodynia (vulvar vestibular syndrome): result of 3 years of experience]
Go to source). - Nerve block injections - May be administered to women who have chronic pain that that does not easily respond to other treatments(16✔ ✔Trusted Source
Measuring Treatment Outcomes in Women With Vulvodynia
Go to source). - Pelvic floor therapy (Physical therapy) - Women with vulvodynia would benefit from pelvic floor exercises as many of them have poorly-toned pelvic floor muscles which incidentally, lend support to the uterus, bladder and the bowel.
- Surgery - In cases where the pain is confined to the hymeneal ring (localized vulvodynia/ vulvar vestibulitis), surgery may be performed (vestibulectomy) to relieve pain, by removing the affected skin and tissues(17✔ ✔Trusted Source
Effect of Vestibulectomy for Intractable Vulvodynia
Go to source). - New topical treatment - Vulvodynia was successfully treated with an analgesic cream consisting of baclofen 5% together with the autacoid palmitoylethanolamide 1%, an endogenous anti-inflammatory compound. Topical treatments that have been reported as beneficial in multiple studies include topical gel anesthetics and estrogen cream particularly in perimenopausal women(18✔ ✔Trusted Source
New topical treatment of vulvodynia based on the pathogenetic role of cross talk between nociceptors, immunocompetent cells, and epithelial cells
Go to source).
Topical nitroglycerin is safe and effective in providing temporary relief of introital dyspareunia and vulvar pain in women with vulvodynia(19✔ ✔Trusted Source
Safety and efficacy of topical nitroglycerin for treatment of vulvar pain in women with vulvodynia: a pilot study
Go to source).
Most often, a single treatment may not suffice and you may have to opt for a combination of suitable methods to manage vulvodynia. It may take several days, weeks or even months for symptoms to improve.
Home Remedies for Vulvodynia
- Avoid all potential vulva irritants such as strong soaps, shampoos, medications, detergents, fabric softeners and douches
- Use unscented toilet paper
- Avoid panty hose
- Try soaking in lukewarm water for a few minutes each day. Avoid hot water tubs
- Avoid foods that make the urine more irritating such as berries, greens, chocolates, beans or nuts
- Rinse vulva with cool water after urination
- During sex, make use of a water-soluble lubricant
- Avoid activities that exert pressure on the vulva, such as bicycling
- Applying cold compress or heat can relive pain in some individuals
- Keep vaginal area dry and clean
- Always wear cotton underwear. Avoid nylon
- Take an antihistamine at night time to reduce itching(20✔ ✔Trusted Source
Vulvodynia - Diagnosis & Treatment
Go to source)