- Vaginal Candidiasis - (http://www.cdc.gov/fungal/diseases/candidiasis/genital/)
- How is vaginitis treated? - (https://www.nichd.nih.gov/health/topics/vaginitis/conditioninfo/pages/treatments.aspx)
What is Vaginal Health?
Many women feel awkward discussing vaginal issues even with their doctor. Vaginal health care is a crucial part of a woman’s overall health. So you should never ignore a problem in the hope that it will just disappear in time. Vaginal infections that are left untreated can spread to the fallopian tubes and uterus and cause infertility. A certain amount of vaginal secretion is normal and it helps to cleanse the vagina and prevent infection. It is important to make a note of any changes in vaginal secretion as well as any other changes as they could be symptoms of an underlying problem.
Causes of Vaginal Problems
Infections are the most common vaginal problem and they can be caused by bacteria, fungi or viruses. The 5 most common types of vaginal infections are:
- Bacterial Vaginosis: A healthy vagina contains a wide variety of bacteria including several types of healthy bacteria. These healthy bacteria keep the unhealthy bacteria levels in check and prevent an infection. If the level of healthy bacteria falls, unhealthy bacteria start to thrive and this results in an infection. This infection is known as Bacterial Vaginosis and it is the most common vaginal infection among women of childbearing age.
- Candida or yeast infection: The correct medical term for this type of infection is Candidal Vulvovaginitis but it is more commonly known as yeast infection or vaginal thrush. The Candida yeast is normally present within the vagina but in very small numbers. When the number of this unicellular yeast increases, the person comes down with a yeast infection. Antibiotic medications, pregnancy and poorly controlled diabetes increase an individual’s risk of this infection.
- Chlamydia Vaginitis: Chlamydia is caused by the bacterium Chlamydia trachomatis and it is one of the most common sexually transmitted infections worldwide. The infection can be transmitted through vaginal, anal or oral sex and there may be no symptoms at all in 70–80% of all female cases. An infection that remains undetected and untreated for a prolonged period is likely to result in pelvic inflammatory disease (PID) which causes scarring inside the reproductive organs and decreases fertility while increasing the risk of an ectopic pregnancy. Multiple sexual partners, a history of sexually transmitted infections and having unprotected sex (without a condom) increase a woman’s risk of getting Chlamydia. Chlamydia is one the most common vaginal health problems.
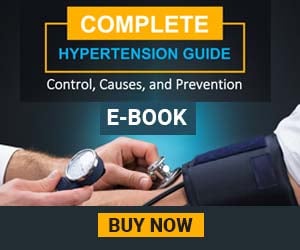
- Trichomoniasis Vaginitis: Trichomonas vaginalis is a parasitic protozoan that causes trichomoniasis in men and women. Trichomoniasis in women is known as trichomoniasis vaginitis as it causes inflammation of the vagina, cervix and urethra. Trichomoniasis is a common sexually transmitted infection and it is estimated that over 160 million people worldwide are affected by this infection annually.
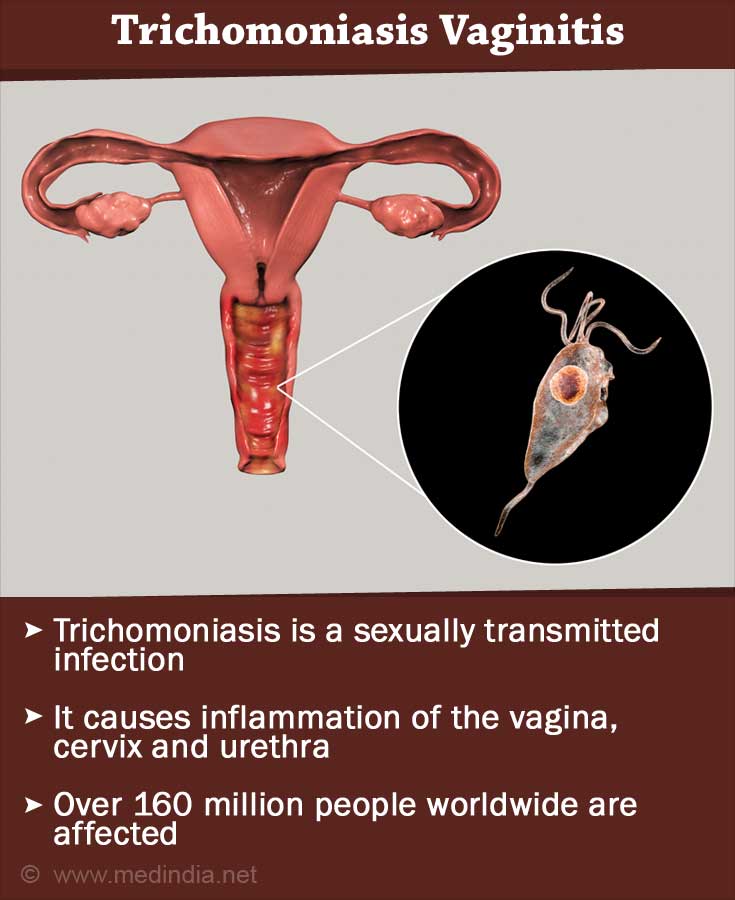
- Viral Vaginitis: There are two main types of virus that can cause Viral Vaginitis – the herpes simplex virus (HSV) and the human papillomavirus (HPV) virus. Both these viruses are spread through sexual contact and so a barrier contraceptive such as a condom can help to reduce the risk of transmission but it cannot offer complete protection from these viruses. Women have a higher risk of getting infected by the HSV virus and since there is no cure for herpes, they will continue to suffer from outbreaks for the rest of their life. The HPV virus results in the growth of genital warts in and around the vagina. Genital warts can be transmitted during sexual intercourse.
Symptoms of Vaginal Problems
The symptoms of vaginal problems can vary greatly depending on the underlying cause of the problem. In most cases, you would notice a change in vaginal discharge along with discomfort such as burning or itching. You may also experience pain while urinating or during intercourse. Here are the symptoms for the most common vaginal problems:
- Bacterial Vaginosis: The most common symptom of Bacterial Vaginosis is increased vaginal discharge that has a distinctive fishy odour. This discharge can be white or even grey in colour and it coats the inside of the vagina. There is little or no pain but there is often mild itching along with a burning sensation while urinating.
- Candida or yeast infection: The change in vaginal discharge is one of the most prominent symptoms of a yeast infection. Most women notice a chunky “cottage-cheese” discharge while a few women experience a white but watery vaginal discharge that is odourless. Itching of the vulva is also a common symptom along with inflammation of the vulva and vagina.
- Chlamydia Vaginitis: Chlamydia is one of the few vaginal health problems that can cause no symptoms at all. In cases where there are symptoms, they are so mild, that they are often overlooked which is why this infection can go undiagnosed for months or even years. Some of the possible side effects of Chlamydia include pain during intercourse, bleeding or spotting between periods, heavier periods, a change in vaginal discharge, pain in the lower abdomen and fever. Some women get the urge to urinate more frequently than usual.
- Trichomoniasis Vaginitis: Up to half of all infected individuals experience no symptoms but women are more likely to experience symptoms than men. The changes in vaginal discharge are very obvious – while healthy vaginal secretions are clear or slightly milky, the vaginal discharge in a woman suffering from Trichomoniasis vaginitis will have a strong odour, it will be frothy and it will be yellow or even green in colour. Vaginal irritation and itching are also possible symptoms along with pain while urinating. A woman who has contracted this sexually transmitted infection will generally notice symptoms between 5 to 28 days from exposure.
- Viral Vaginitis: The symptoms of the two main viruses that cause Viral Vaginitis differ greatly and so it is easy to differentiate between the two types of viral infections. The herpes virus causes lesions on or around the clitoris and other parts of the vulva as well as the rectal region. Pain, itching and burning are also common symptoms and some women may also notice swelling in their lymph nodes. Herpes lesions take approximately 2 weeks to turn into ulcers before they crust and heal. Once the lesions have healed, the virus becomes dormant but it becomes active from time to time which is what causes repeated herpes outbreaks. The symptoms are most likely to return during times of illness or mental stress as the body’s immune system is vulnerable at these times.
The HPV virus is very common and there are several types of HPV viruses – some cause genital warts while others cause cervical and anal cancer. Only 10% of those who contract HPV will develop genital warts and in most cases, the warts are the only symptom of this infection. Those who do not develop genital warts can still transmit the virus to their partners. In most cases, the warts develop in clusters with each wart as small as 1 mm in diameter; however, in severe cases, they can grow or spread into large masses that can even spread to the inside of the vagina.
Diagnosis of Vaginal Problems
In order to detect the cause of a vaginal problem, the doctor will require the individual’s precise and complete medical history. The doctor would also need to carry out a vaginal examination along with clinical and laboratory tests. Vaginal swab tests, urine tests and even blood tests may be necessary in order to obtain a definite diagnosis. Here are some of the tests for vaginal problems:
- Bacterial Vaginosis: The vagina is normally slightly acidic with a pH level between 3.8 and 4.2. A swab of the vaginal discharge is smeared onto a litmus paper to check its acidity level. If the pH level is 4.5 or more, it means that the woman’s vaginal secretions are not acidic enough which would indicate that she has a high risk of bacterial vaginosis. The second test is called the whiff test where a solution of 10% potassium hydroxide is added to a slide containing the vaginal discharge. If the woman has bacterial vaginosis, there will be an immediate release of a characteristic fishy odour. In the third test, the doctor will place a small amount of the vaginal discharge on a slide. A drop of sodium chloride is added to the sample so that the bacteria-coated cells are easily visible.
- Candida or yeast infection: There are 3 main tests to detect the presence of a yeast infection: a microbial culture, an antigen test and a vaginal wet mount microscopy test. In a microbial culture test, the doctor will send a sample of the vaginal discharge to a laboratory where the microorganism causing the infection is allowed to propagate so that it can be easily identified. In an antigen test, the individual’s blood is tested for antigens that are specific to the candida yeast. It generally takes a day to get the results of this test. In a vaginal wet mount microscopy test, a sample of the vaginal discharge is mixed with a salt solution and placed under a microscope so that the doctor can look for yeast cells which would indicate the presence of a yeast infection.
- Chlamydia Vaginitis: Earlier the main test for Chlamydia was the cell culture test but in the last decade, the Nucleic acid amplification tests (NAAT) has become the gold standard. The NAATs are very sensitive tests that have a high accuracy rate. Vaginal swabs are the optimal specimen to detect chlamydia in women using these tests.
- Trichomoniasis Vaginitis: There are three main tests for Trichomoniasis with varying degrees of accuracy. The saline microscopy test is the cheapest test for this infection but it has a sensitivity level of just 60 - 70%. The culture test is a little more expensive and it has a 70 - 90% sensitive level. The nucleic acid amplification tests (NAATs) are the rather costly but they are 80 - 90% sensitive.
- Viral Vaginitis: The Polymerase chain reaction (PCR) is one of the most common tests to check for genital herpes. This blood test is very accurate and can help diagnose the infection even if the individual does not have any lesions. A cell culture test can also be used to detect the presence of the herpes simplex virus under a microscope. Antibody tests are also used to diagnose genital herpes.
Treatment for Vaginal Problems
- Bacterial Vaginosis: Doctors often prescribe a one week course of the antibiotics metronidazole or clindamycin to treat bacterial vaginosis. Antibiotic creams might also be prescribed for topical application. The role of probiotics (healthy bacteria) in the treatment of bacterial vaginosis is currently the subject of several studies. Preliminary research indicates that probiotics can offer an 88-90% cure rate in a period of just 30 days.
- Candida or yeast infection: Doctors prescribe either intravaginal or oral medications or a combination of both, depending on the severity of the infection. Topical azole drugs are very effective and have an 80-90% cure rate.
- Chlamydia Vaginitis: Chlamydia can be effectively cured with antibiotics. Some of the commonly prescribed drugs include azithromycin, doxycycline and ofloxacin. Pregnant women may be prescribed medications that contain amoxicillin.
- Trichomoniasis Vaginitis: The treatment for trichomoniasis vaginitis is pretty standard and consists of a single dose of metronidazole (2000 mg). 95-97% of all cases are resolved with this single dose but there are a few cases where the infection proves to be resistant to metronidazole in which case, the infection returns and requires follow-up treatment.
- Viral Vaginitis: Genital herpes cannot be cured but there are certain drugs that can be used to shorten the duration of the outbreaks as well as reduce the frequency of outbreaks. Acyclovir and Valacyclovir are the most commonly prescribed antiviral drugs that are used to control herpes. These drugs also reduce the number of lesions and the pain. There is no cure for genital herpes but in approximately 80% of all HPV cases, the warts eventually clear even without treatment. Your doctor may suggest ablative or topical treatments depending on the size, number and location of the warts.
Health Tips
- There are a number of steps that you can take to ensure good vaginal health care. Your personal hygiene, diet and sexual practises play a large role and should not be ignored.
- Personal hygiene: In addition to your daily shower, wash the outer portions of your vagina with warm water and a mild soap at least once a week. Avoid scented feminine hygiene products as far as possible as these chemicals might cause itching and discomfort. Avoid douching, as this is one of the main causes of yeast infections in women.
- Diet: Follow a meal plan that is low in processed sugar and flour and instead include plenty of fruits and vegetables in your diet. Have yogurt and yogurt-based products such as buttermilk as this will increase the levels of healthy bacteria in your body. You can also discuss vaginal health supplements such as probiotic tablets with your doctor as this could help to prevent recurrent infections.
- Sexual practises: Always practise safe sex and make sure that your partner uses a condom correctly to reduce the risk of tearing. Make regular appointments for a female health check-up and always be completely honest with your gynaecologist regarding your sexual practises.