- Extrapulmonary Tuberculosis. A review - (https://www.ncbi.nlm.nih.gov/pubmed/1341593)
- What is Extrapulmonary Tuberculosis? - (https://www.ncbi.nlm.nih.gov/pubmed/15520485)
- Diagnosis and Treatment of Extrapulmonary Tuberculosis - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc4388900/)
- Extra pulmonary TB - (http://www.tbonline.info/posts/2016/3/31/extrapulmonary-tb/ )
- TB Risk Factors - (https://www.cdc.gov/tb/topic/basics/risk.htm )
- Pulmonary Tuberculosis - (https://medlineplus.gov/ency/article/000077.htm)
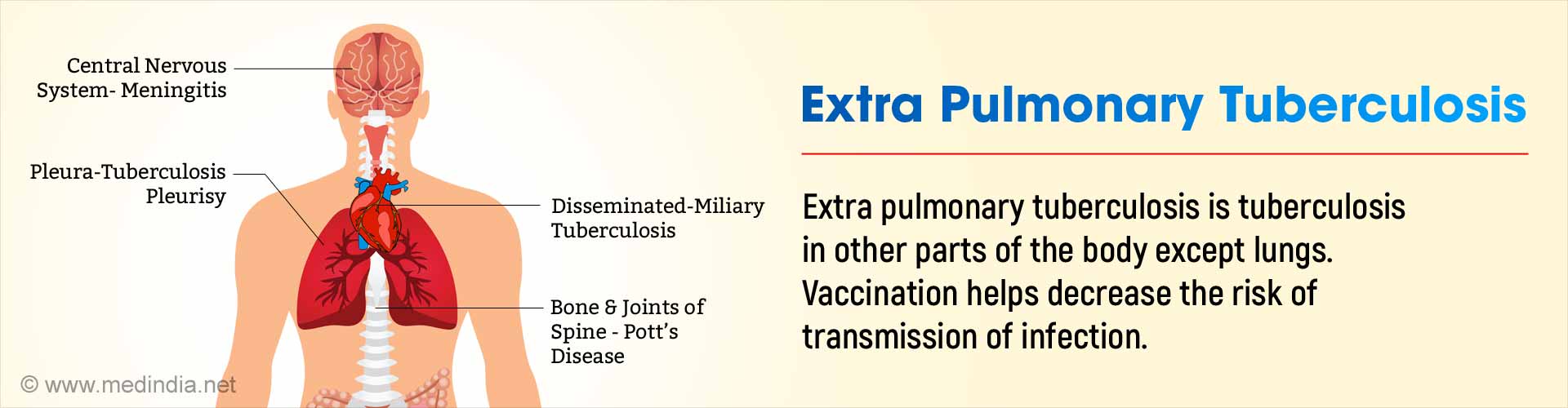
What is Extra Pulmonary Tuberculosis?
Extra pulmonary tuberculosis is the infection of tissues and organs other than the lungs by Mycobacterium tuberculosis and a few related organisms. It is most commonly a sequel of lung infection by the same organism.(1✔ ✔Trusted Source
Extrapulmonary Tuberculosis. A review
Go to source) Pulmonary tuberculosis is one of the most common and prevalent infections in India, because of multiple reasons. There are many risk factors for tuberculosis, which include immunocompromised states, overcrowding, and smoking among others. The classical symptoms of pulmonary tuberculosis include persistent low grade fever, cough with expectoration loss of appetite and weight.
The symptoms of extra pulmonary tuberculosis are more varied, but fever and weight loss are present in the majority of cases. The treatment of tuberculosis in general, is standardized by various bodies in the world, and is effective in curing the disease. In India, the RNTCP protocol is the preferred model of diagnosis and treatment. As with any preventable disease, though, prevention is definitely better than cure, and simple methods such as universal vaccination help to decrease the risk of transmission of infection.
What is Pulmonary Tuberculosis?
Pulmonary tuberculosis is a disease caused due to infection of the lungs by Mycobacterium tuberculosis and other related bacteria. Although quite a few bacteria of the mycobacterium genus can cause tuberculosis, Mycobacterium tuberculosis is by far the predominant threat. Pulmonary tuberculosis is spread by infection via airborne droplets which are created by sneezing or coughing. People who inhale these droplets are called contacts.(2✔ ✔Trusted Source
Pulmonary Tuberculosis
Go to source) Once the bacteria inside these droplets reach the lungs, three things can happen depending on the immunity of the person inhaling them:
- The person with good immunity is able to fight the bacteria and kill them, thus preventing the infection.
- Some people may be able to halt the bacteria and prevent it from causing disease, but the bacteria may still be alive inside, unable to break out. This is called Latent TB. It is estimated that one third of all the people in the world have latent TB.
- In people with poor immunity, which can be because of various reasons, full blown tuberculosis occurs. This is called active TB. Sometimes, people with latent TB infection can progress to active TB if there is some interference with their immunity.
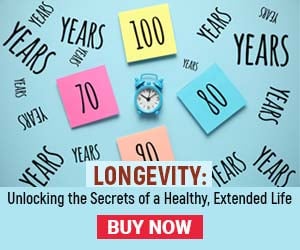
The symptoms of active pulmonary tuberculosis include:
- Fever, which is usually persistent and low grade, but may also sometimes be high grade and spiking
- Prolonged cough for three weeks or more
- Coughing of blood
- Loss of weight
- Loss of appetite
- Fatigue
- Night sweats
What is Extrapulmonary TB?
The infection of any organ in the body other than the lungs by Mycobacterium tuberculosis is called extrapulmonary tuberculosis. The most common sites of extrapulmonary tuberculosis are lymph nodes, pleura, abdomen, bone and joint, spinal cord and the brain and its coverings.(3✔ ✔Trusted Source
What is Extrapulmonary Tuberculosis?
Go to source)
Lymph Node Tuberculosis
This is the most common form of extra pulmonary TB. Lymph nodes are the draining stations of lymph in the body. Lymph from the lungs goes through the lymph nodes situated near the neck and above the collar bones. These lymph nodes are the most common nodes in the body affected by TB. When the tuberculosis bacteria reach these lymph nodes, the immune material inside the nodes launches an attack against the bacteria. This causes inflammation and swelling, which may not be warm or tender. This is called a cold abscess. Sometimes, the node may burst and may form a fistula, which is a communicating tract, to the skin. Sometimes, the node may be so big as to exert pressure on the surrounding structures and cause problems because of that. Some nodes near the windpipe may compress on it and cause breathing difficulty and stridor. Tuberculous lymph nodes may be excised and studied by pathologists to give a definitive diagnosis of the disease.
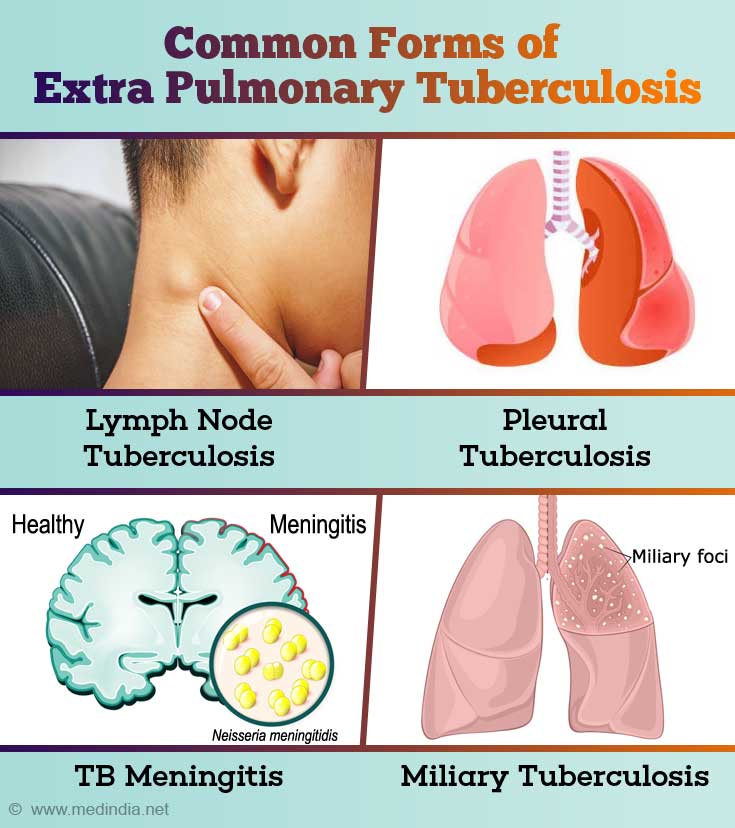
Pleural Tuberculosis
Pleura are the coverings of the lungs. There are two layers of the pleura, called the parietal layer and visceral layer. The visceral layer is closely applied to the lung surface, while the parietal layer is near the chest wall per se. There is usually a small space between these layers, which has a thin layer of fluid, which enables lubrication.
In many patients with pulmonary tuberculosis, the pleura may get inflamed because of immune reaction even without the TB bacteria actually reaching the pleura. But sometimes, the bacteria can get nestled in the space between the two layers of the pleura and cause pleural TB. The presence of bacteria in the pleura will cause inflammation and excessive fluid accumulation in the pleural space. This is called pleural effusion. Involvement of the pleura will cause breathing difficulty and pain in inspiring air. Diagnosis of pleural TB can be done by simple aspiration of the pleural fluid and testing for the presence of bacteria by microscopy, genetic tests or by culture. Definitive proof of bacterial involvement of the pleura can be done by pleural biopsy.
TB Meningitis and TB of the Nervous System
The brain and the spinal cord have three layers of tissue covering it, called the meninges. The three layers, from inside to outside are the pia mater, arachnoid mater and dura mater. These meninges perform several important functions, including shielding the precious neural tissue from injury, as well as secreting and absorbing a fluid called the Cerebro Spinal Fluid (CSF), which is present between the arachnoid and the pia mater. Inflammation of the meninges is called meningitis.
TB can cause blockage of the small arteries of the brain, leading to loss of blood supply to that part of the brain, causing stroke. TB bacteria can involve the meninges by spread from the lungs via blood. This often happens in patients who lack sufficient immunity. Involvement of the meninges or the brain itself may cause many symptoms and signs, including headache, nausea, vomiting, stiff neck, confusion, delirium, seizures etc. Analysis of the CSF by lumbar puncture is essential in diagnosing this situation
Tuberculosis of the Bone and Joints
TB bacteria can cause infection of bones and joints anywhere in the body, but usually have a predilection to involve the spine. Infection of the vertebral column (spine) by TB can cause collapse and fracture of the bones and/or abscess formation, which may lead to compression of the spinal cord, with drastic consequences. Infection of joints anywhere may cause swelling and pain of the joints. As with TB anywhere else in the body, the best method of diagnosis is to obtain a sample of the tissue and test for the presence of bacteria. But many other modes of investigations, such as X rays and CT scans may be needed.
Abdominal Tuberculosis
Tuberculosis of the abdomen can result from direct seeding of the abdominal cavity or by blood spread from the lungs. Sometimes, the bacteria can enter the food pipe and can get to the intestines. TB bacteria can cause infection of any part of the abdomen and pelvis, including the intestines, liver, kidney, spleen, urinary system and the uterus and its associated structures. Each form of abdominal tuberculosis has its own specific set of symptoms and signs. Diagnosis of each of these requires different modalities. Some of the methods used are:
- Endoscopy for intestinal tuberculosis
- Liver and kidney function tests
- Biopsy of the suspected organ
- Ultrasound of the abdomen
- CT/MRI scans
- Cystoscopy of the urinary bladder and biopsy
- Hysteroscopy etc. for uterus and fallopian tube
Miliary Tuberculosis
Miliary TB is a widely disseminated form of tuberculosis from a focus in the body that is rich in the TB bacteria. The dissemination occurs via both the blood and the lymph. Miliary TB derives its name from the many millet seed shaped nodules that occur in many parts of the body due to this condition.(4Extra pulmonary TB
Go to source)
Other Forms Of Extra Pulmonary Tuberculosis
TB can affect many other organs and parts of the body, including the skin, eyes, heart and its coverings, large and small arteries, the male genital system etc. Some of the conditions that can be caused by TB include:
- Skin - TB verruca cutis, lupus vulgaris, warts, scrofuloderma, tuberculids
- Eyes – Phlyctenular conjunctivitis, uveitis
- Heart – Pericarditis, myocarditis
- Arteries – aneurysms, endarteritis
- Genital system – Genitourinary tuberculosis (TB of the uterus, fallopian tubes etc), adrenal insufficiency
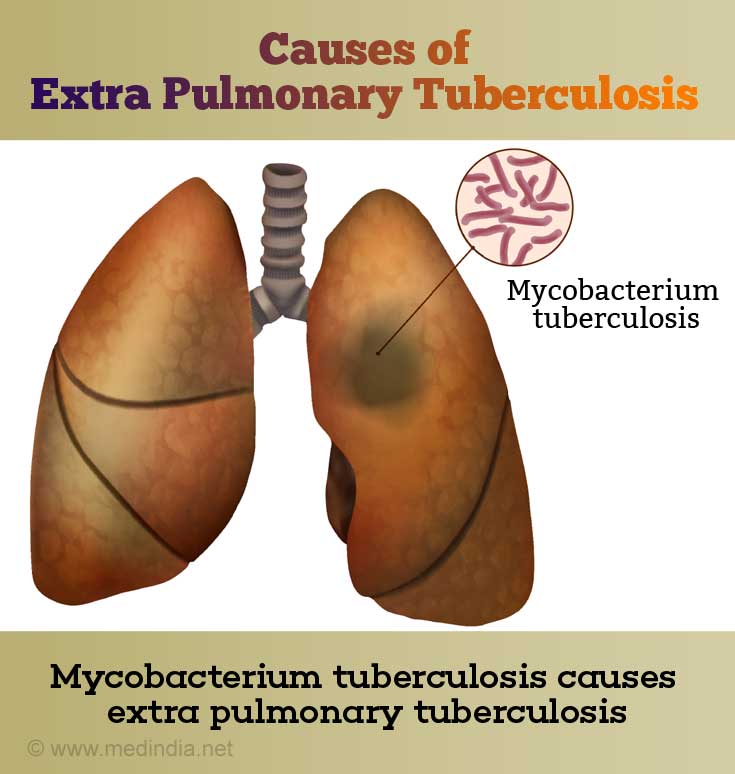
Causes Of Extra Pulmonary Tuberculosis
Tuberculosis in general is caused by the group of organisms that are collectively called the Mycobacterium tuberculosis complex. Most of the human cases of TB are caused by Mycobacterium tuberculosis. On some rare occasions, other bacteria of the same family, called atypical mycobacteria or Non-Tuberculous Mycobacteria can also cause illnesses that mimic TB. For example, some cases of abdominal tuberculosis in India are caused by Mycobacterium bovis, which is because of ingestion of raw milk. Some skin ulcers such as fishtank ulcer and Buruli ulcer are caused by Mycobacterium marinum and Mycobacterium kansasii.
Signs and Symptoms of Extra Pulmonary Tuberculosis
The signs and symptoms of Extra Pulmonary Tuberculosis depend on the organ system involved by the disease. But in general, the findings of decreased appetite, loss of weight and low grade fever for many days are common in all forms of Extra Pulmonary Tuberculosis.
| Type of Extra Pulmonary TB | Symptoms | Signs |
| Lymph Node Tuberculosis | Fever Swelling near the armpit or groin Oozing from the swelling in later stages | Firm, non-tender lymph node enlargement, which may be matted Fistula and sinus tract formation |
| Pleural Tuberculosis | Fever Non-productive cough Breathing difficulty Pain on deep breathing | Decreased air entry in the chest over where the fluid has accumulated Hypoxia Tachypnea |
| Tuberculosis of the Nervous System | Fever Headache, nausea, vomiting Altered Mental Status Convulsions Weakness of muscles | Signs of raised intracranial tension such as papilledema (fluid accumulation in the retina of the eye), seizures, low consciousness etc TB can involve the small vessels of the brain, called TB endarteritis, causing stroke |
| Tuberculosis of the bone and joints | Pain Difficulty in daily activities Inability to maintain posture | Pott’s spine, kyphosis, scoliosis Dactylitis Signs of arthritis |
| Abdominal Tuberculosis | Pain in the abdomen Fever Decreased appetite, loss of weight Nausea, vomiting Constipation | Tenderness Abdominal distension Ascites Signs of intestinal obstruction Anemia Sterile pyuria |
Risk Factors of Tuberculosis
- Age – Extremes of age. Young children and elderly adults are both at increased risk
- Immunodeficiency because of diseases such as HIV
- Immunosuppression because of medications
- Overcrowding
- Contact with a person who has active or latent TB
- Alcohol intake
- Diabetes Mellitus
- Kidney failure(5✔ ✔Trusted Source
TB Risk Factors
Go to source)
Treatment Guidelines for Extra Pulmonary Tuberculosis
India follows the RNTCP (Revised National Tuberculosis Control Program) guidelines for the management of Tuberculosis.
The cornerstone of successful management of any disease is correct diagnosis. The diagnosis of Tuberculosis is unfortunately difficult, even though new tests are available to aid the physician. The principles of diagnosis of TB are:
- See the bacterium – Using microscopes and special stains
- Grow the bacterium – Using culture methods
- PCR – This test, called GeneXpert MTB/RIF, amplifies the genetic material of the bacterium and also detects resistance to one of the first line drugs
- Imaging – Imaging tests specific to the organ involved can help identify TB.
- Chest X-ray is mandatory for all patients to rule out pulmonary tuberculosis, which may have reactivated.
- Ultrasound of the abdomen
- CT of the abdomen/brain/pelvis depending on the site of involvement
- Histopathology – Biopsy of the affected part and examination by a pathologist is necessary
- Other tests – Other ancillary tests such as ADA levels for active TB and Interferon Gamma Release Assay for latent TB may be used(6✔ ✔Trusted Source
Diagnosis and Treatment of Extrapulmonary Tuberculosis
Go to source)
The RNTCP guidelines divide Extra Pulmonary TB into two categories: Seriously ill and Not seriously ill.
Seriously Ill:
- TB meningitis
- Disseminated TB
- TB pericarditis
- TB peritonitis & intestinal TB
- Bilateral or extensive pleurisy
- Spinal TB with neurological complications
- Genito-urinary tract
Not Seriously Ill:
- Lymph Node TB
- pleural effusion (unilateral)
- Bone (excluding joints)
- Peripheral joints
Patients with TB are broadly divided into two categories, and treatment is standardized for each particular category
| Category | Type of Patient | Regimen |
| Category I | New sputumsmear-positive or smear-negative pulmonary TB (PTB) New Extra Pulmonary TB | 2H3 R3Z3 E3 + 4H3 R3 |
| Category II | Sputum smear-positiverelapse Sputum smear-positivefailure Sputum smear-positivetreatment after default Others | 2S3H3R3Z3E3+ 1H3R3Z3E3 +5H3R3E3 |
| H- Isoniazid, R- Rifampicin, Z- Pyrazinamide, E-Ethambutol | ||
The prefix number implies the number of months the treatment is to be given and the suffix (subscript 3) denotes the number of doses of each drug to be given in a week.
There are also separate guidelines for management of Drug-resistant Tuberculosis.
Some special cases of TB, such as TB meningitis and TB pericarditis may need steroids to prevent further complications.