- Russotto V, Cortegiani A, Fasciana T, Iozzo P, Raineri SM, Gregoretti C, et al. What healthcare workers should know about environmental bacterial contamination in the intensive care unit. Biomed Res Int. 2017; 2017: 6905450. DOI - (10.1155/2017/6905450. PMID: 29214175.)
- Doll M, Stevens M, Bearman G. Environmental cleaning and disinfection of patient areas. Int J Infect Dis. 2018 Feb; 67: 52-57. DOI - (10.1016/j.ijid.2017.10.014. PMID: 29102556.)
- Mogyoródi B, Dunai E, Gál J, Iványi Z. Ventilator-associated pneumonia and the importance of education of ICU nurses on prevention - preliminary results. Interv Med Appl Sci. 2016 Dec; 8(4): 147-151. DOI - (10.1556/1646.8.2016.4.9. PMID: 28180003.)
- Mulu W, Kibru G, Beyene G, Damtie M. Postoperative nosocomial infections and antimicrobial resistance pattern of bacteria isolates among patients admitted at Felege Hiwot Referral Hospital, Bahirdar, Ethiopia. Ethiop J Health Sci. 2012 Mar; 22(1): 7-18. PMCID: PMC3437975. - (10.1556/1646.8.2016.4.9. PMID: 28180003.)
- Agarwal M, Shiau S, Larson EL. Repeat gram-negative hospital-acquired infections and antibiotic susceptibility: a systematic review. J Infect Public Health. 2017 Oct 20. pii: S1876-0341(17)30259-9. DOI - (10.1016/j.jiph.2017.09.024. PMID: 29066020.)
- Khan HA, Baig FK, Mehboob R. Nosocomial infections: epidemiology, prevention, control and surveillance. Asian Pac J Trop Biomed. 2017 May; 7(5): 478-82. - (https://doi.org/10.1016/j.apjtb.2017.01.019)
- Mehta Y, Gupta A, Todi S, Myatra SN, Samaddar DP, Patil V, et al. Guidelines for prevention of hospital acquired infections. Indian J Crit Care Med. 2014 Mar; 18(3): 149-63. DOI - (10.4103/0972-5229.128705. PMCID: PMC3963198.)
What are Hospital Acquired Infections?
Hospital acquired infections (HAI), medically termed as nosocomial infections, are infections that are acquired by patients admitted in the hospital wards, as well as by hospital staff, including doctors and nurses who work at the hospital. The most common HAI are caused by bacteria. Fungi and viruses also cause HAI, but to a far lesser extent.
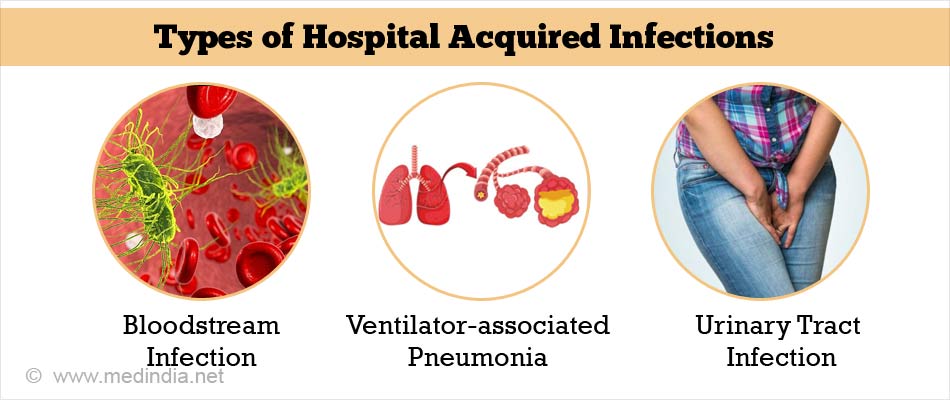
Types of Hospital Acquired Infections
The most common types of HAI are briefly discussed below:
- Bloodstream Infection (BSI): This type of infection is technically termed as septicemia. It occurs when an infection in any part of the body enters the bloodstream and spreads rapidly to other parts of the body. Septicemia can be life-threatening and must be treated quickly. Catheter-related bloodstream infections (CRBI) are very common in a hospital setting.
- Ventilator-associated Pneumonia (VAP): This type of infection occurs in patients who are on mechanical ventilator support in an intensive care unit (ICU). The patients are usually critically ill and elderly, who are highly susceptible to respiratory infections like pneumonia.
- Urinary Tract Infection (UTI): This type of infection affects the urinary tract. UTI is usually caused by bacteria. In certain cases, it is caused by fungi and occasionally by viruses. Infection can occur in the lower urinary tract, involving the bladder (cystitis) or the upper urinary tract, involving the kidneys (pyelonephritis). In a hospital setting, UTI can occur as a result of not using aseptic techniques during insertion of a urinary catheter for men/women.
- Surgical Site Infection (SSI): This is one of the most common types of infection in the operating room. SSI can be caused as a result of not following strict aseptic practices, before, during, and after the surgery.
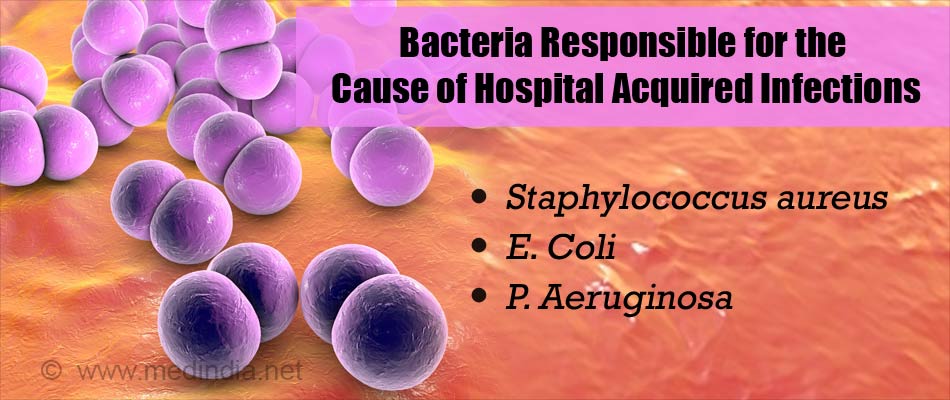
What are the Causes of Hospital Acquired Infections?
The major cause of HAI is bacterial infections, which account for about 90% of all HAI. The most common bacteria that cause nosocomial infections include Staphylococcus aureus (S. aureus), Escherichia coli (E. coli), and Pseudomonas aeruginosa (P. aeruginosa). These three bacteria, as well as other causes (fungal and viral) that are responsible for these infections are briefly discussed below:
- S. aureus:These bacteria are spherical in shape (coccus) that are clustered like a bunch of grapes. S. aureus is a very common pathogen in hospital settings. The methicillin resistant Staphylococcus aureus (MRSA) is a common strain involved in nosocomial infections. MRSA are so called because these bacteria are resistant to methicillin (antibiotic), indicating that methicillin is unable to kill this strain of bacteria. MRSA are resistant to virtually all types of β-lactam antibiotics. The patient is at high risk if methicillin has been previously administered; the patient has been admitted to an ICU; the patient has been exposed to an infected patient; or from surgical procedures.
- E.coli: These bacteria are commonly present in the gastrointestinal (GI) tract. Although most strains of E. coli are harmless, there are some, like the enteropathogenic E. coli that can be very dangerous, causing severe diarrhea, kidney damage and even death.
- P. aeruginosa: These bacteria are opportunistic pathogens, meaning they seek an opportunity to infect susceptible people such as those with a weak immune system. These include the elderly and people suffering from HIV/AIDS. These bacteria produce dangerous toxins that attack many organ-systems and cause a multitude of infections, including urinary tract infection (UTI), bacteremia, skin and soft-tissue infections, respiratory infections, GI tract infections and others.
- Other Causes: These include fungal and viral infections, which collectively account for 10% of HAI. Hospital-acquired fungal infections can be caused by Candida albicans, Aspergillus spp., and Cryptococcus neoformans. Some viruses that are implicated in HAI include respiratory syncytial virus (RSV), hepatitis B and C viruses, HIV, rotavirus, herpes simplex virus, and influenza virus.
What are the Signs and Symptoms of Hospital Acquired Infections?
The signs and symptoms of HAI are closely linked to the type of infection involved and the organ-system affected. The common symptoms include the following:
- Fever
- Headache
- Rashes
- Burning sensation during urination
- Difficulty urinating
- Redness, warmth, swelling, and pain from a surgical incision
- Oozing of fluid (blood and/or pus) from a surgical wound
- Severe coughing
- Shortness of breath
- Nausea and vomiting
- Diarrhea

What are the Risk Factors of Hospital Acquired Infections?
Anybody admitted in a hospital is at risk of infection. A study from Ethiopia found that approximately 11% of patients (sample size: 300) undergoing surgery contracted an infection. Nosocomial infections are more in developing areas like Asia, Sub-Saharan Africa, and Latin America, where approximately 40% hospitalizations result in acquired infections.
Some of the associated major risk factors are briefly listed below:
- Prolonged stay in the ICU (>3 days)
- Age above 70 years
- Prior use (or misuse/abuse) of antibiotics
- Coma
- Shock
- Trauma
- Indwelling catheters
- Ventilator support
- Surgery
- Drugs affecting the immune system (steroids, chemotherapy)
How do you Diagnose Hospital Acquired Infections?
Diagnosis of HAI is made by an experienced infectious disease specialist by direct clinical observation. Clinical signs and symptoms like skin rashes, coughing, fever, or runny nose, among other symptoms, indicate that an infection may be present. These clinical observations are confirmed by performing blood tests. The routine blood tests for infections include TC (total count), DC (differential count), ESR (erythrocyte sedimentation rate), and hemoglobin estimation. It may also be necessary to isolate the incriminating microbe by culturing the pathological samples.
How do you Treat Hospital Acquired Infections?
Treatment is carried out on the basis of isolation of the causative agent. This will help in selecting the specific antibiotic for treating the infection. In addition to the antibiotic therapy, the doctor will advise to eat a healthy diet, consume lots of fluids, and take adequate bed rest to help in the recovery process.
How do you Prevent & Manage Hospital Acquired Infections?
Prevention and management of HAI essentially revolves around the efficacy of infection control strategies. Some of these strategies are briefly described below:
Prevention of HAI by Standard Hygiene Practices
- Handwashing: Hands are the most common modes of transmission of pathogenic microorganisms. And handwashing is the single-most effective method to prevent this from happening. If the hands are visibly soiled or blood-stained, they should be washed with soap and water. Alternatively, if the hands are not visibly soiled, they should be rubbed with a solution containing 0.5% chlorhexidine and 70% ethanol.
- Gloves: These should be worn after hand hygiene procedure, particularly if a mucus membrane or broken skin needs to be touched or if some aseptic technique needs to be carried out, such as the insertion of a catheter.
- Gown: A gown should be worn to prevent accidental soiling of clothes and skin during procedures that may generate splashes of blood or other bodily fluids.
- Mask/Eye Protection: These should be worn to protect the mucus membrane of the eyes and respiratory tract from aerosols of blood or other bodily fluids, while carrying out procedures or attending a patient. Moreover, patients and their relatives should be made to wear masks if they present with respiratory symptoms.
- Head Covering: Proper head covering is mandatory for all surgical staff in the operating room. However, this is not required for routine patient care.
- Medical Equipment: All types of medical equipment should be handled with utmost care, avoiding unnecessary touching. Disposable items and sharps should be discarded safely in designated color-coded plastic bags. Any equipment (especially surgical equipment) soiled with blood or other bodily fluids should be regarded as an infection hazard and should be handled accordingly.
Management of Hospital Acquired Infections by Isolation Strategies
If an infection breaks out in the hospital, it can be managed by isolation of infected patients from uninfected patients and health staff.
Screening: In order to properly implement isolation strategies, the need for isolation should be carefully evaluated. This can be done by screening the patients for the following:
- Neutropenia (low count of neutrophils in the blood)
- Presence of an immunological disorder
- Skin rashes
- Diarrhea
- Patients known to have a communicable disease
Identification of the Type of Isolation Required: There are essentially two types of isolation in the ICU. These are briefly described below:
- Protective isolation for patients having neutropenia or if they are immunocompromised, so that they can be protected from acquiring opportunistic infections.
- Source isolation of infected patients so that they are unable to transmit the infection to other uninfected patients or health staff.







