- The Discovery of Insulin: An Important Milestone in the History of Medicine - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6205949/)
- Regulation of Insulin Synthesis and Secretion and Pancreatic Beta-Cell Dysfunction in Diabetes. - (https://doi.org/10.2174/157339913804143225)
- Insulin and insulin resistance. - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1204764/)
- Insulin delivery methods - Past, present and future. - (https://pubmed.ncbi.nlm.nih.gov/27014614/)
- Insulin delivery methods: Past, present and future. - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4787057/)
- Clinical outcome of using insulin at 40 IU/ml and 100 IU/ml in pump treatment. Results of a controlled multi-center trial. - (https://pubmed.ncbi.nlm.nih.gov/3307309/)
- A review of insulin pen devices. - (https://pubmed.ncbi.nlm.nih.gov/20463417/)
- Evolution of Insulin Delivery Devices: From Syringes, Pens, and Pumps to DIY Artificial Pancreas. - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7261311/)
- Current trends in needle-free jet injection: an update. - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5936486/)
- WHO Best Practices for Injections and Related Procedures Toolkit. Best practices for injection. - (https://www.ncbi.nlm.nih.gov/books/NBK138495/)
- Insulin pumps in general practice. Aust Prescr. - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6299172/)
- A Clinical Overview of Insulin Pump Therapy for the Management of Diabetes: Past, Present, and Future of Intensive Therapy - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6695255/)
- Use of insulin pumps in India: suggested guidelines based on experience and cultural differences. - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2956384/)
- Insulin Storage: A Critical Reappraisal. - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7783014/)
- Insulin. - (https://www.ncbi.nlm.nih.gov/books/NBK560688/)
About
Insulin delivery devices have evolved drastically since their invention in 1922. They are all aimed to provide insulin to the patients with minimal discomfort(1✔ ✔Trusted Source
The Discovery of Insulin: An Important Milestone in the History of Medicine
Go to source).
Insulin is a peptide hormone produced by the beta cells of the islets of Langerhans of the pancreas.Whenever there is a dysfunction in these cells, it can trigger pathogenesis of both type 1 and type 2 diabetes(2✔ ✔Trusted Source
Regulation of Insulin Synthesis and Secretion and Pancreatic Beta-Cell Dysfunction in Diabetes.
Go to source).
What is the role of insulin?
Insulin is primarily used to control blood glucose levels in people with diabetes. The techniques used earlier in insulin injections were cumbersome and painful and were different from the techniques employed today. Modern methods are a lot easier and are designed to help the patient, even a child, autonomously take the insulin shot without any help.
The other significant function of insulin are(3✔ ✔Trusted Source
Insulin and insulin resistance.
Go to source):
- Regulating glucose metabolism.
- Transporting amino acid within the cells.
- Stimulating Lipogenesis
- Decreasing the breakdown of lipids.
What happens when there is Lack of Insulin in the Body?
Insulin deficiency results in hyperglycaemia, which can cause the following symptoms weight loss, tiredness, vomiting, hypotension, infections, hyperventilation (due to ketoacidosis) and impaired conscious level and coma. Hence, we need to introduce artificial insulin in the body.
What is Artificial Insulin?
Insulin is available in many forms and is identical to human insulin. The first genetically engineered, synthetic “human” insulin was produced in 1978 using E. coli bacteria. Thanks to decades of research, people can choose various modes to deliver insulin to their body.
Delivery Modes
Pharmaceutical companies have developed several insulin delivery systems, each having its own advantages and disadvantages. Though subcutaneous insulin delivery is the standard route of insulin administration, it is associated with injection pain, needle phobia, lipodystrophy, noncompliance and peripheral hyperinsulinemia. Some of these systems are described below(4✔ ✔Trusted Source
Insulin delivery methods - Past, present and future.
Go to source):
- Syringe and Vial
- Insulin pens
- Jet Injectors
- Insulin Pump
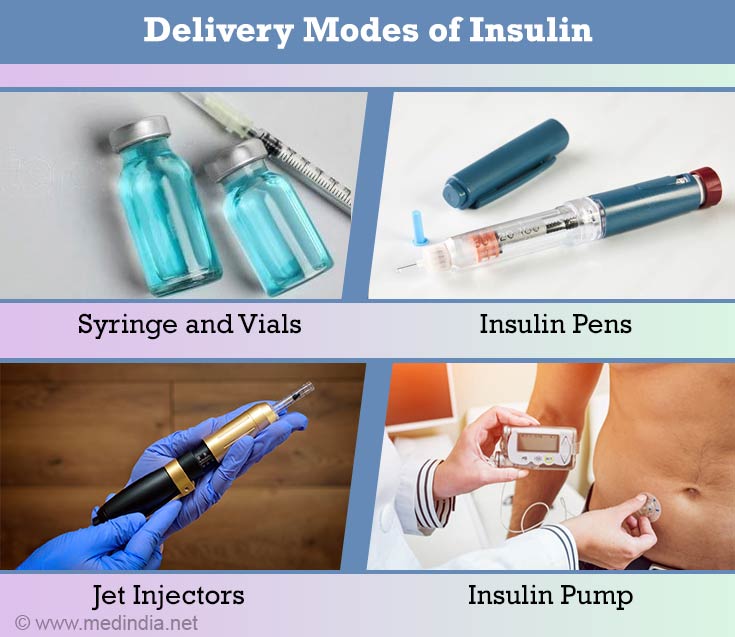
Syringe and Vial
This is the most commonly used, and the most economical of all the delivery devices. It consists of a vial or a small bottle and insulin syringes. The needles of the syringes are short and thin, making them less painful. Recent advancements have given rise to coated needles that further reduce the pain. The syringes have gradations to help draw the correct dosage of insulin(5✔ ✔Trusted Source
Insulin delivery methods: Past, present and future.
Go to source).
In India, these insulin vials are available in two strengths 40 IU/ML and 100 IU/ML. Accordingly two types of syringes are available – red cap for 40 IU syringe with gradation up to 40 and orange cap for 100 IU syringe with gradation up to 100(6✔ ✔Trusted Source
Clinical outcome of using insulin at 40 IU/ml and 100 IU/ml in pump treatment. Results of a controlled multi-center trial.
Go to source).
The patient must be careful in choosing the correct type of syringe for the correct dose of insulin.
Insulin Pens
These are available just like any oversized ink pen that can be carried in the pocket. They are available in two forms – temporary and permanent pens. These insulin pen devices are an alternative to the traditional insulin vial-and-syringe method and offer many advantages. They are less painful and more preferred by the patient(7✔ ✔Trusted Source
A review of insulin pen devices.
Go to source).
Temporary Pens
These are made of plastic with the insulin already filled in. However the pen needles have to be fitted separately. The pen has a colour-coded knob representing a particular type of insulin or a combination, e.g. yellow represents ‘short acting’ insulin. The pen has units marked on it denoting a particular dose level. The pen has to be adjusted to the recommended dose, and is then injected at the injection site. Once all the insulin is used up, the pen is to be discarded(8✔ ✔Trusted Source
Evolution of Insulin Delivery Devices: From Syringes, Pens, and Pumps to DIY Artificial Pancreas.
Go to source).
Permanent Pens
These are made of metal and are slightly heavier. The cartridges filled with insulin are separately available. The pen has to be fitted with these cartridges and used in the same manner as the temporary pen. Once a cartridge is fully used, new cartridges are fitted and the pen can be reused(8✔ ✔Trusted Source
Evolution of Insulin Delivery Devices: From Syringes, Pens, and Pumps to DIY Artificial Pancreas.
Go to source).
Advantages:
- It is user- friendly
- It is less painful
- It can be injected anywhere, at an airport or a party, hence is suitable for any busy person
Disadvantages:
- It is comparatively expensive
- It may be confusing to an ordinary person
- It cannot be used by the visually challenged
- It may not be easily available
Jet Injectors
These are pen-like insulin delivery devices. They look very similar to an insulin pen, but do not have a needle. They deliver a small jet of insulin under high pressure at the push of a button(9✔ ✔Trusted Source
Current trends in needle-free jet injection: an update.
Go to source).
Thus, unlike a pen, there is no puncture of the skin involved, and this insulin is delivered in the subcutaneous region. Certain cleaning instructions have to be strictly followed to maintain sterility. The jet injector should be cleaned with a damp cloth from the outside. This device should also be stored at the desired temperature(10✔ ✔Trusted Source
WHO Best Practices for Injections and Related Procedures Toolkit. Best practices for injection.
Go to source).
Advantages:
- It is less painful since a needle is not used
- It has better acceptance among patients than the pen.
- It can be carried anywhere.
- Disposing the pens or needles is effortless as there are no needles.
Disadvantages:
- It is fairly expensive
- It cannot be used by slim people or by the visually impaired individuals
- It may cause bruising in some individuals
- It is not recommended for those taking anti-coagulants, or for those on dialysis or individuals with hemophilia
- Some feel that it causes more pain than regular needles
- Sterilizing and preparing for the dose is time consuming
Insulin Pump
Today, the efficiency of the insulin delivery system of the insulin pump is closest to the natural human pancreas.
This device is quite similar to a pager and is fixed to the waist belt of the patient. A small canula or a needle is inserted into the subcutaneous tissue through which insulin is continuously delivered. This canula is attached to an insulin cartridge. The dosage is predetermined. The site of injection is to be changed every three days. The insulin is infused from the pump reservoir through an infusion set(11✔ ✔Trusted Source
Insulin pumps in general practice. Aust Prescr.
Go to source).
At any given time certain insulin is delivered to the body as a “basal” dose. This dose can be varied at different times. The patient has to deliver an extra dose (bolus) during or after meals. The insulin dose starts at 0.1 units. The patient can decide the rate at which this bolus is to be delivered.
This method is more suitable for type I diabetics. However the people using the pump must monitor the blood glucose 3-4 times a day to make sure that the pump is working well.
Adequate knowledge regarding calorie counting is very important to decide the bolus that needs to be delivered after each meal(12✔ ✔Trusted Source
A Clinical Overview of Insulin Pump Therapy for the Management of Diabetes: Past, Present, and Future of Intensive Therapy
Go to source).
Advantages:
- Patients have greater flexibility in choosing food as all they need to do is to count the carbohydrates value and set the bolus which will enable them to have normal blood glucose levels.
- Pricking the body 2-3 times a day is avoided.
Disadvantages:
- It is expensive, and therefore unaffordable by the common man.
- Knowledge regarding carbohydrate counting needs to be mastered to decide the bolus dose.
- The device needs to be worn all the time.
- Monitoring the blood glucose several times a day is required to ensure that the insulin delivery by the pump is not interrupted(13✔ ✔Trusted Source
Use of insulin pumps in India: suggested guidelines based on experience and cultural differences.
Go to source).
How can we Store Insulin?
Insulin that is in use can be stored at room temperature. When extra insulin vials or pens are bought, the one in use can be stored at room temperature in a cool dark place while the extra ones can be stored in the refrigerator.
Insulin should not be stored at or exposed to extreme temperature, in other words it should neither be exposed to sunlight nor frozen(14✔ ✔Trusted Source
Insulin Storage: A Critical Reappraisal.
Go to source).
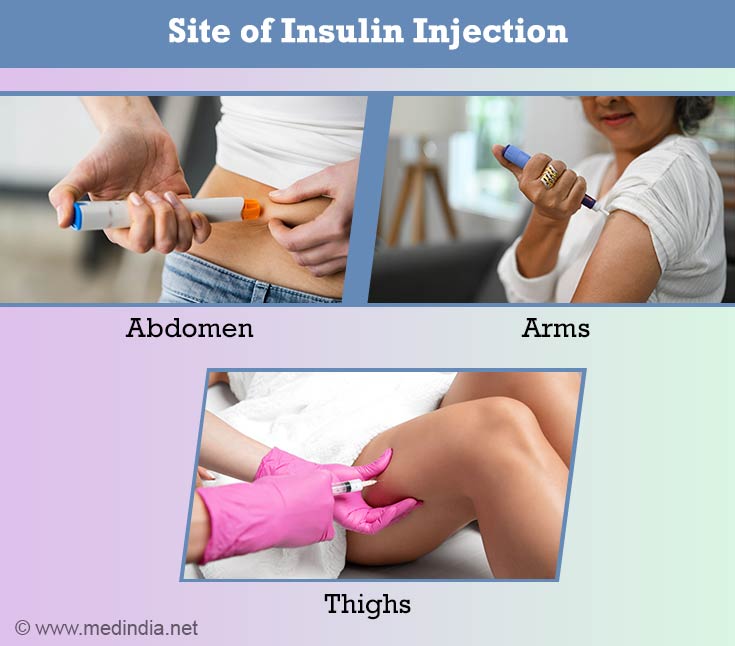
Where is Insulin Injected?
Insulin has to be injected in the subcutaneous region of the body. This is typically on the thighs, abdomen, buttocks or the arms. One may need assistance while injecting in the arms(15✔ ✔Trusted Source
Insulin.
Go to source).
Insulin should not be injected directly into the blood stream.
New Technologies
Apart from the above delivery devices, a lot of research is ongoing for the newer modes of insulin delivery. Artificial pancreas, islet cell transplant, non-invasive insulin delivery, including oral, transdermal, nanotechnology-based and gene therapy-based ones, are under research(5✔ ✔Trusted Source
Insulin delivery methods: Past, present and future.
Go to source).
Conclusion
Insulin is the one of the modes of treatment for diabetes. A wide variety of insulin delivery devices are available today. Each delivery device is directed to deliver the desired dose of insulin. The aim is to make the mode patient friendly with minimum discomfort.
It should be economical, painless and convenient for the patient. Research is ongoing for other modes of insulin delivery. Just like we have more patient friendly devices today than earlier, we can expect to see more patient friendly devices in the near future.