- FAQ: Getting a Liver Transplant - (https://www.ucsfhealth.org/education/getting_a_liver_transplant/)
- Center for Liver Disease and Transplantation - (http://columbiasurgery.org/liver/faqs-about-life-after-liver-transplant)
- Living Donor Liver Transplantation - (https://www.myast.org/sites/default/files/pdfs/living_liver.pdf)
- Overview - Transplant - (https://www.niddk.nih.gov/health-information/liver-disease/liver-transplant)
- Liver Transplant - (http://www.mayoclinic.org/tests-procedures/liver-transplant/home/ovc-20211840)
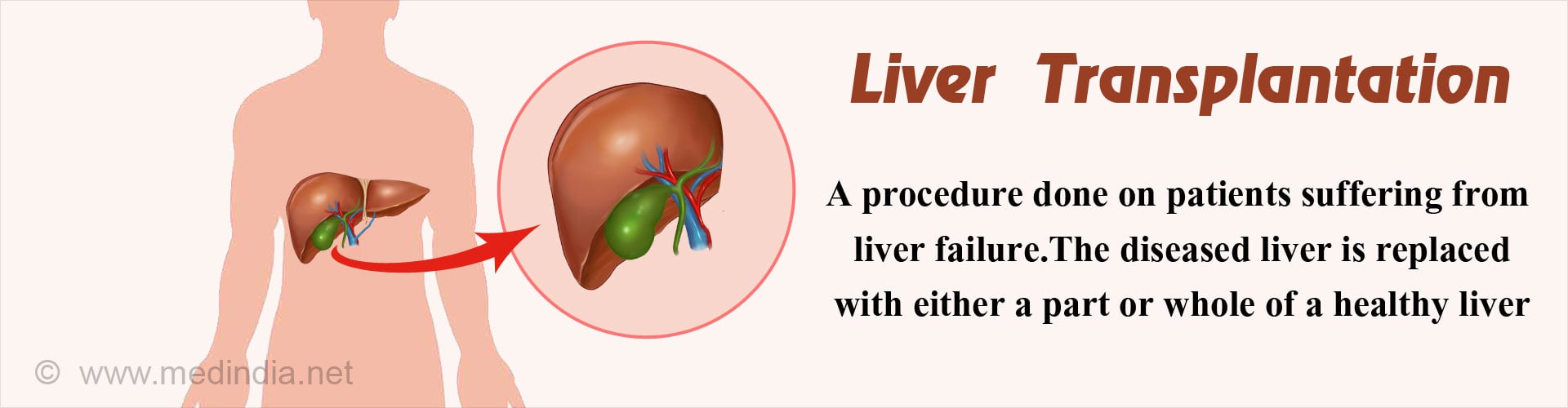
What is Liver Transplantation?
Liver transplantation is a surgical option for the treatment of liver failure where the surgeon replaces the diseased liver with a healthy one. The transplant ensures a better quality of life for the recipient.
Currently, the liver for transplantation is obtained from two different groups of donors.
Living donors:
In this case, it is possible for a liver failure patient to receive a liver from his/her blood relative. The rate of success is better if the liver is obtained from a first degree relative (father, mother, brother, sister, son or daughter).
Ideally it is important to match the tissue of the recipient with the donor so that the body will not reject it at a later stage. If a patient does not have any matched first-degree donor, then other relatives can be approached.
Only a segment of the liver from the donor would be transplanted to the recipient, as there is only one liver in the human body. The liver in the donor as well as in the recipient would then grow, as it has an excellent regenerative capacity.
Under exceptional circumstances, and only when it is medically and ethically acceptable to do so, it might be possible to consider a living unrelated donor for a liver transplantation as the supply of the organ far exceeds the demand. The procedure can be done if better results are anticipated when compared to a cadaveric organ donation and an enduring relationship exists between the donor and the recipient.
Such unrelated donation requires the permission of an authorization committee. This ensures prevention of any illicit trading of human organs.
Cadaveric donors:
This kind of donation is usually seen following a road traffic accident or an irreversible injury or tumor of the brain. In these individuals, a part of the brain known as the brain stem fails to function. If this happens, the patient is said to be brain dead. These patients are usually in the intensive care on ventilators and provided with artificial support and cannot be revived by any known means.
It has now been accepted that brain death equates in medical and ethical terms to the death of an individual. Following brain death, the brain stops functioning, however some solid and critical organs like the heart,lungs, liver, kidneys, and lungs may still continue to function. It is therefore possible to obtain organs for donation from such individuals as neither consciousness nor spontaneous respiration is possible in the absence of a functional brain stem.
Brain death is different from coma, as a comatose patient has chances of revival and recovery, whereas a person who is brain dead cannot be revived by any known means.
The patient's relatives are explained about the condition of the patient and requested for organ donation. Following their consent, it might be possible to retrieve the organs to be transplanted into a needy patient. The diagnosis of brain death can only be made when certain medical criteria have been met.
There is an increasing need to spread awareness about this concept of organ donation as most of the organs from potential brain dead donors often get wasted.
Facts and Statistics on Liver Transplantation
- More than 17,000 people are on the waiting list to get a liver transplant in the United States. While 6000 odd patients have their liver transplanted every year in the United States, around 1700 patients die waiting for it.
- Among the transplanted livers, 80% of them are still functioning after 1 year and about 65% of them are functioning after 5 years.
- Around 200 patients receive liver from living donors every year while around 6000 patients receive them from deceased donors.
- The living donor has a 38% chance of a complication due to the transplant and the risk of dying from it is 1 in 500.
What is the Role of the Liver in the Body and What is Liver Failure?
When the functioning of the liver is inadequate to meet the requirements of the body, a condition called liver failure sets in. It can either happen suddenly (acute liver failure for example following consumption of heavy poisonous substances or due to drug toxicity or it can occur over a prolonged period of time (chronic liver failure; like cirrhosis of the liver).
The liver is the largest organ in the human body and is situated below the diaphragm, on the right side of the abdomen. It would not be an exaggeration if the liver were compared to a very large chemical factory. In fact, it participates in more chemical reactions than that happens inside any factory.
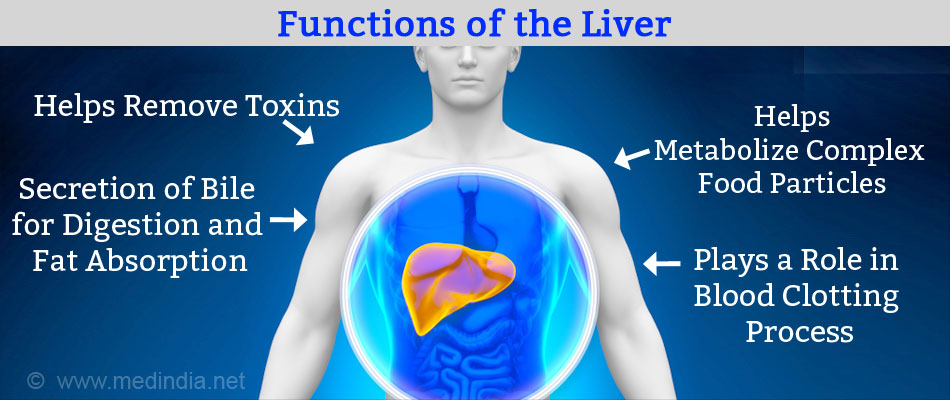
The liver functions -
- Plays a vital role in the detoxification process, and helps remove toxins and drugs from the blood.
- Produces several biologically important compounds such as bile that helps infat digestion, as well as certain specific proteins and vitamin absorption).
- Plays a major role in the metabolic process - it breaks down complex food particles into smaller ones in such a way that the human body can use it.
- Serves as a storage organ for sugar (glucose), minerals and other substances.
- Plays a very important role in the clotting of blood (we would otherwise bleed to death even after a small injury) by the production of several compounds required for the same.
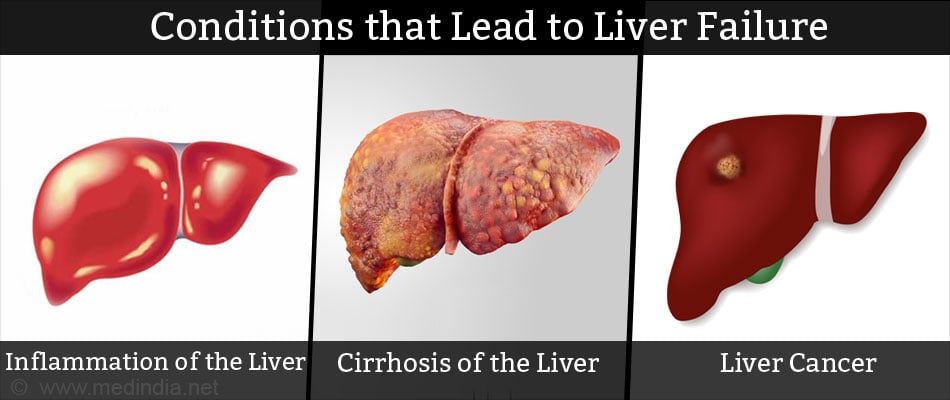
Due to the role it plays in the human body, it is vital to preserve our liver. The following conditions may give rise to liver failure:
- Inflammation of the liver over a prolonged time period.
- Cirrhosis of the liver.
- Disorder of the immune system, in which the bile duct gets badly affected and destroyed (autoimmune disorder), eventually leading to liver failure. This condition is referred to as primary biliary cirrhosis.
- Structural abnormality of the bile duct, called biliary atresia. In this condition there is either an absence or a closure of the bile duct opening. This is most commonly seen in children.
- Chronic alcohol intake, eventually leading to cirrhosis and liver failure.
- Congenital disorders of copper metabolism, leading to excess deposition of copper throughout the body including the liver (Wilson's disease, Menke's disease).
- Liver cancer
What happens following Liver Failure?
After a diagnosis of liver failure is made, the patient is referred to a transplant unit. The doctor will evaluate the patient’s condition and assess the need for a liver transplant. Certain tests will be conducted to check if the patient can undergo a liver transplant without any complication. The functioning of other organs such as the heart, kidney, and lungs are also evaluated. The tests include:
- Blood tests like liver function tests and tests for HIV or hepatitis.
- Imaging tests like computed tomography (CT scan) and ultrasound.
- Ultrasound to determine blood flow to the liver.
- Echocardiogram or ECG to evaluate cardiac function.
- Pulmonary function studies (PFT) to determine the functioning of the lungs.
If the patient opts for a deceased donor transplant then the name is entered in an organ transplant waiting list registry and is assigned a priority score depending on the medical condition. Two scoring systems determine the priority of the patient during this waiting time. The Model for End-stage Liver Disease (MELD) is used for people aged 12 years and older and the Pediatric End-Stage Liver Disease (PELD) is used for children under the age of 12 years. Specific blood tests are used to compute these scores. The child’s age as well as its degree of growth failure are also considered while computing PELD. Scores for MELD range from 6 to 40 while scores for PELD range from negative numbers to 99.
A higher score indicates a more urgent need for transplant. The score indicates whether a person is likely to die within the next 90 days without a transplant.
People who are critically ill with acute liver failure and are likely to die within a week are given the highest priority for liver transplant.
The complete details of the patient such as the blood type and tissue type are registered. In case of donor availability, the most eligible patient will be contacted for the liver transplantation.
What is the Difference between an Ideal and a Non-ideal Liver?
An ideal liver is one that is obtained from a living or a dead person who has no risk or very little risk of transmitting an infectious disease or cancer.
A donor liver is also considered a non-ideal if there is a higher risk of the liver not working well following the transplant. A non-ideal liver is also one that carries a higher risk of transmitting an infection or cancer.
Patients are sometimes offered such non ideal livers if the risk of dying from waiting is more than the risk from a non-ideal liver.
Examples of Non-ideal liver are -
- If the donor has been infected with hepatitis B or C.
- If the donor has had cancer.
- If the donor has used IV drugs or had sex with a high-risk partner in the past one year.
- If the liver obtained is a split one, is from an older patient
- If the liver donation happened after circulatory or cardiac death.
What are the Contraindications to a Liver Transplant?
Not all individuals with liver failure can undergo a liver transplantation. Certain conditions can make a patient unfit for the surgery and these include:
- Presence of a large cancer in the liver
- Presence of a malignancy (cancer) in any other part of the body
- Presence of an active infection
- Presence of severe heart, lung or kidney disease
- Presence of advanced HIV disease (AIDS)
Continued usage of alcohol or inability to comply to the recommendations made by the doctor would also exclude a patient from having a transplant. Normally a patient should be of alcohol for at least 3 to 6 months before they will b taken up for transplant surgery.
What is the Procedure for a Liver Transplant?
Before the Transplant -
During the waiting period, constant and regular follow ups are essential. To improve the chances for successful surgery, it is best to lead a healthy lifestyle ( example - stop alcohol & smoking) and maintain a positive attitude to life during this period.
If a suitable donor is identified,the hospital staff would contact the patient regarding the possibility of a liver transplantation, and a hospital admission will be made. Following admission, a number of blood tests and other specialized tests are done to assess the clinical condition of the patient.
The tissue of the donor and the recipient are tested for compatibility. The patient is also assessed by the anesthetist, who notes a complete medical and surgical history of the patient. Suitable instructions are given to the patient to be followed the day before the liver transplant is scheduled.
During the Transplant -
Two different medical and surgical teams work together to ensure the success of the liver transplantation. One team of surgeons and anesthetists prepare the potential recipient for the surgery, while the other team works on the removal of a liver segment from the donor.
The surgery on the recipient is performed under general anesthesia and can take anywhere between 4 to 14 hours. After a cut in the upper abdomen, the diseased liver is disconnected from its blood vessels and the common bile duct, and removed. The recipient’s blood vessels and bile duct are then attached to the donor’s liver, which is placed in the same location where the diseased one was located.
As liver transplantation is a major surgery, it would not be possible to move around during the next 24 or 48 hours. Several tubes are placed around the recipient's body to enable post-operative recovery. This ensures that the functioning of the body can go on without any compromise.
A tube is placed through the mouth into the windpipe to enable breathing. This is most commonly attached to a machine called the respirator that will help in breathing by contraction and relaxation of the lungs.The function of the bowel cannot resume immediately following the surgery. To aid in bowel function, a tube called the nasogastric tube would be placed through the nose, into the stomach.
Intravenous fluid will also be administered to provide hydration and nutrition.
In addition, a urinary catheter to drain the urine from the bladder would also be placed. This can be removed a few days after the surgery.
Furthermore, synthetic tubes would be placed around the abdomen to drain the blood and other fluids from in and around the liver. This can be removed after 1 week.
Post Transplant -
After the first few days in the intensive care unit (ICU), the patient is usually shifted into a single private room. A liver transplant patient will be expected to stay in the hospital for around 1 to 2 weeks.
The presence of infection, postoperative complications and the recovery of the patient are factors that play a critical role in planning the discharge.
During discharge, the patient is instructed about medications. Written instructions are usually given by most transplants units (called a discharge summary). It is very important to follow the instructions given by the doctor and take the appropriate medicines in time to ensure a better quality of life.
The drugs to prevent the rejection (immunosuppressive drugs) of the liver are required to be taken for rest of the life and SHOULD NOT BE STOPPED or the dose changed unless the doctor has been consulted.

What is the Follow up Procedure after a Liver transplantation?
Once a major surgery like liver transplant takes place, a lifelong follow up is required.
The first visit to the hospital is usually recommended after one or two weeks. However, if there is any fever or discharge from the wound or if the patient feels unwell for any other reason they would be advised to report back to the hospital immediately.
A contact telephone number of the unit should be kept handy in event of the necessity to contact either the doctors or the unit nurse.
During the first visit, the doctor examines the wound and removes the surgical sutures (stitches) if the wound has healed properly. Any problems faced by the recipient after surgery can be discussed with the doctor at this time. Subsequent visits are scheduled at the end of one month, 2 months, 3 months, 6 months, one year, 18 months and so on for life.
During these visits, blood tests to check the liver and the general state of health, ultrasound scans and x-rays may be undertaken. The immunosuppressant dosage may also be altered. In the long run, the dosage is gradually brought down.
What are the Complications of a Liver Transplant?
Rejection of the transplanted liver:
In case of transplants, drugs called immunosuppressants have to be given to suppress the natural tendency of the body to fight the foreign tissue, called immunity. Some of these have to be taken throughout the lifetime of the patient to prevent rejection.
Sometimes despite the drugs, the immune system identifies the liver as non-self and starts reacting against it aggressively and destroys it. This is called rejection.
Rejection can happen immediately after the surgery or a few days, months or even several years after the surgery. The rejection is diagnosed by blood tests and by a biopsy and can usually be controlled by additional medications or by increasing the dosage of medicines. The immunosuppressants drugs have to be taken throughout the lifetime of the patient to prevent rejection.
- Increased chances of infection: The immune system of a patient who is receiving immunosuppressants is compromised, leading to an increased susceptibility to infections. The incidence of these infections can be prevented if appropriate care is taken such as wearing masks, avoiding exposure to contaminated places and so on. The medications may also cause other side effects like bone thinning and increased chances of diabetes.
Other complications include:
- Leakage of bile
- Bleeding
- Chest infections
- Blockage of blood vessels by formation of blood clots
- Recurrence of the liver disease in the transplanted liver
What is the Prognosis for a Liver Transplantation Surgery?
- The outlook of patients who have undergone a liver transplant is good.
- Among the transplanted livers, 80% of them are still functioning after 1 year and about 65% of them are functioning after 5 years.
- Several patients are able to return to routine activities after recovering a few months following the surgery.
However, the outlook is dependent on -
- Undergoing regular blood tests to check for any damage in the liver due to rejection, infection or problems with the blood vessels or bile ducts.
- Regularly taking required medicines.
- Keeping all medical appointments.
- Maintaining a healthy lifestyle including exercising, not smoking or drinking and eating healthy.