- Pancreatic cancer - (https://en.wikipedia.org/wiki/Pancreatic_cancer#Prevention_and_screening)
- About Pancreatic cancer - (http://www.mayoclinic.org/diseases-conditions/pancreatic-cancer/basics/alternative-medicine/con-20028153)
- Bailey & Love's SHORT PRACTICE of SURGERY, 25th Edition
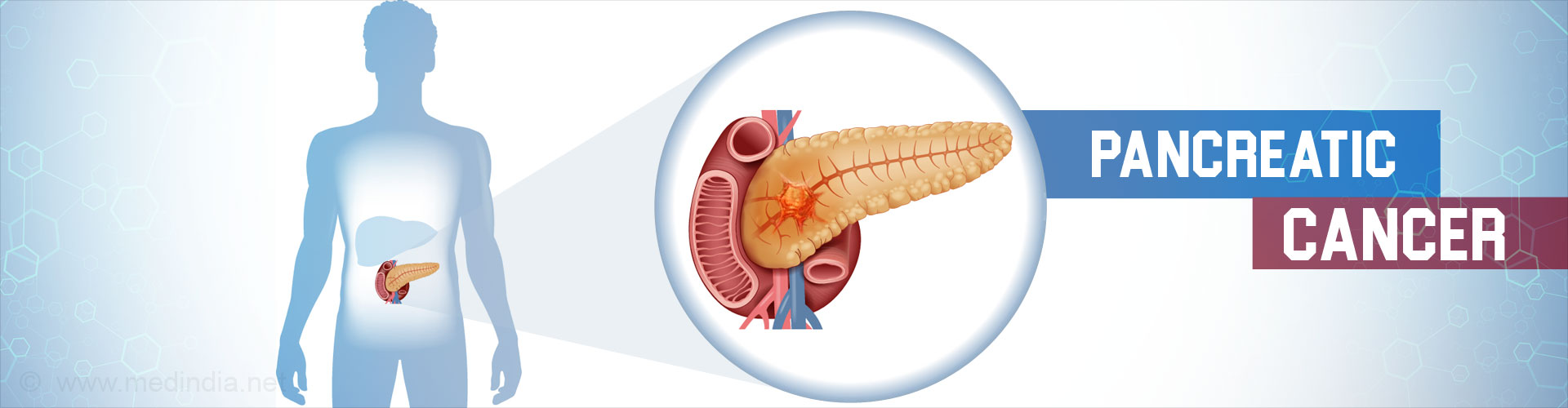
What is Pancreatic Cancer?
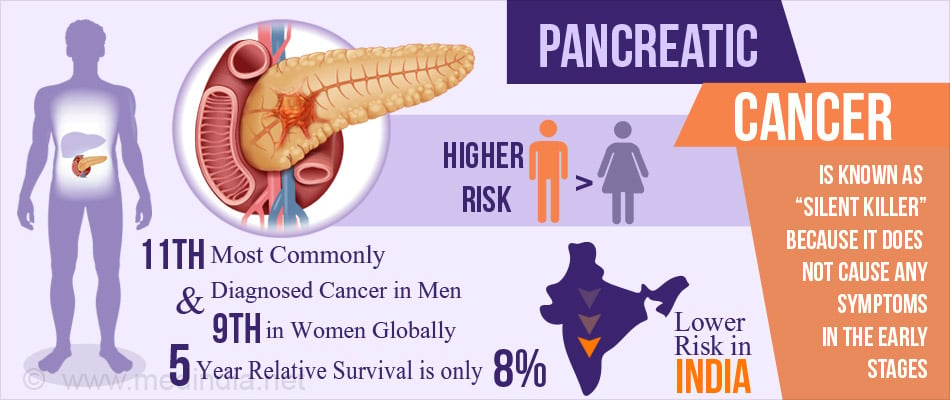
Pancreatic cancer is a malignancy of the pancreas, mostly involving its exocrine part. It is an aggressive tumor and very often not detected till it is quite advanced. As such it is one of the leading causes of cancer death.
Most tumors occur within the head or neck of the organ (75%). A few occur in the body (15 – 20%) and the rest in the tail of the pancreas.
Pancreatic cancer accounts for 2 – 3% of all cancers worldwide. It is the 6th leading cause of cancer death in the UK and the fourth leading cause in USA.
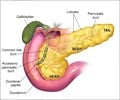
Overview of Pancreas
The pancreas is situated in the abdominal cavity behind the stomach and in front of the spine.
It has an exocrine part that secretes digestive juices and an endocrine part that secretes the hormones insulin and glucagon concerned with regulation of blood glucose levels.
Structurally, the organ is divided into head, neck, body and tail. The endocrine portion, referred to as the Islets of Langerhans is situated in the tail portion.
How Does Pancreatic Cancer Form?
Like every other cell in the body, the cells of the pancreas constantly grow and multiply, with old cells being replaced by new ones. There is a perfect balance between the cell death and renewal.
If by some mechanism, this harmony gets disturbed, a large number of cells are produced than what is required for normal function, resulting in a tumor or cancer. If this disorder occurs in the pancreas, it leads to pancreatic cancer.
The cancer can arise from either the endocrine or the exocrine cells of the pancreas.
This type of cancer is called primary pancreatic cancer. Cancerous cells can also spread to other parts of the body such as the liver, lungs, bones, brain, lymph nodes and other organs, leading to metastatic pancreatic cancer (spreads from pancreas to other parts of the body).
A metastatic cancer can also lodge within the pancreas from other cancers such as primary cancer of kidney, lung, colon, stomach or melanomas. They account for only 2-5% of all pancreatic cancers.
Most of the pancreatic exocrine cancers arise in its ductal system. They are termed ductal adenocarcinomas.
The cancers arising from the endocrine part are called neuroendocrine tumors (1 – 2%).
These tumors are less aggressive when compared to the adenocarcinomas and carry a better prognosis.
What are the Different Stages of Pancreatic Cancer?
For treatment purposes, pancreatic cancer is staged, usually by a CT scan. The most commonly used staging system is referred to as the AJCC – UICC system.
The disease is divided into four stages ranging from early to advanced disease. Factors taken into account include Tumor size, spread to lymph Nodes and distant Metastasis, which is referred to as TNM classification.
The disease is further broadly divided into three categories based on whether surgical resection is possible. They include ‘resectable’, ‘borderline resectable’, and ‘unresectable’.
Diseases in the earlier stages and those that have not spread to blood vessels or other organs may be resected provided the patient is fit and prepared to undergo this major operation.
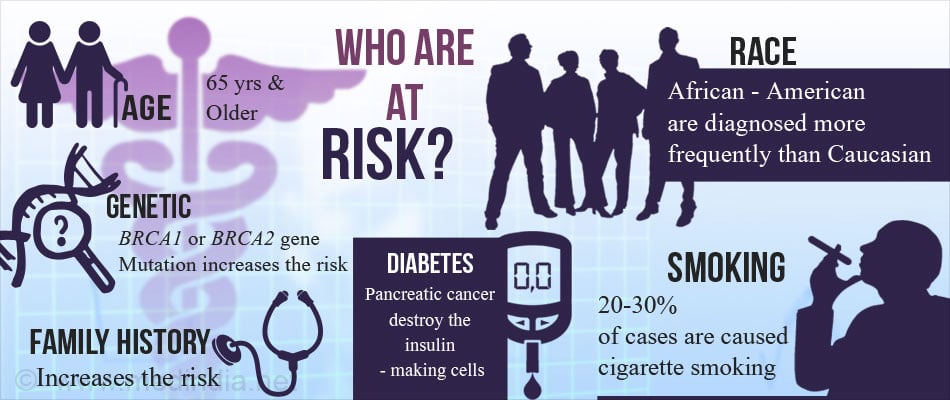
What are the Risk Factors of Pancreatic Cancer?
The incidence of pancreatic cancer is more in African Americans.
Age, sex and race - Pancreatic cancer risk increases with age. It is uncommon before 40 years. Most cases are diagnosed after 65 years of age.
Gender - It is more common in men compared to women
Following are the risk factors in developing pancreatic cancers -
- Cigarette smoking
- History of chronic pancreatitis
- Diabetes mellitus
- Obesity
- Family history of hereditary cancer syndromes such as Peutz Jeghers syndrome, dysplastic nevus syndrome, Lynch syndrome and BRCA-2 gene mutation.
- Family or personal history of pancreatic malignancy.
- Low levels of lycopene and selenium
- Occupational exposure to certain chemicals, radiation and a combination of other environmental factors can cause pancreatic cancer.
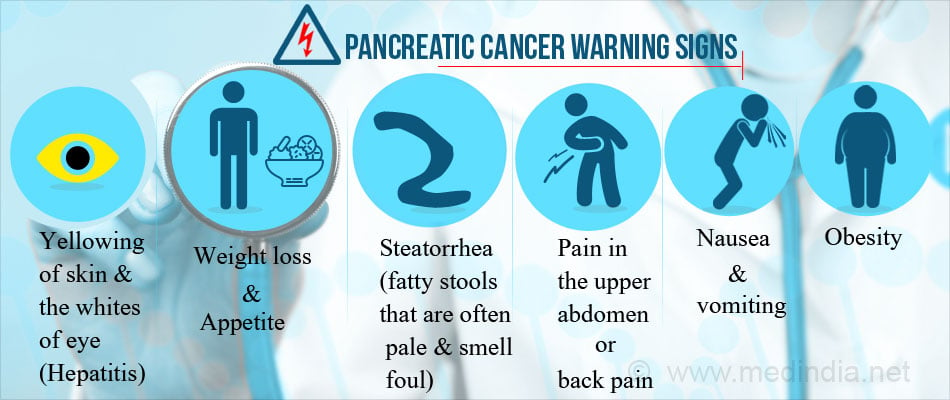
What are the Symptoms of Pancreatic Cancer?
Pancreatic cancer grows silently but aggressively and often does not produce symptoms till the disease is fairly advanced. This is one of the main reasons for its poor prognosis generally. The symptoms vary depending on which part is affected and extent of spread and include-
- Upper abdominal pain that may radiate to the back
- Jaundice or yellowish discolouration of skin and eyes
- Loss of appetite
- Nausea and vomiting
- Tiredness and fatigue
- Weight loss
- Enlarged glands in the neck
- Itching, that can be distressing
- Depression
- Venous thrombosis
What are the Complications of Pancreatic Cancer?
As the disease progresses, the following complications may ensue.
Obstructive jaundice due to blockage of the biliary system and bile not being able to flow to the intestines. A bypass may be necessary or a stent may be placed in the bile duct to keep it open.
Severe pain – As the tumor grows in size, it may compress the nerves causing severe often unbearable pain. Pain medications and radiation to shrink the tumor may offer temporary relief.
Occasionally a nerve block may be performed injecting alcohol into the nerves to control the pain.
Bowel obstruction – When the tumor infiltrates into the duodenum, it becomes obstructed, preventing the passage of food beyond.
A bypass surgery may be performed to bypass the obstructed part or a stent may be placed in the small intestine to keep it patent.
Weight loss – May be due to several causes such as nausea and vomiting caused by chemotherapy, bowel obstruction making eating difficult or deficiency of pancreatic juices causing impaired digestion and absorption of nutrients.
How do you Diagnose Pancreatic Cancer?
Usually the disease is fairly advanced when the doctor sees the patient. A history and physical examination may raise the suspicion of pancreatic cancer. Further tests are necessary to confirm the diagnosis and know the extent of disease in order to plan treatment.
- History - Patient usually gives a history of jaundice, weight loss and pruritis. Other points in the history such as smoking, family history of cancer, and presence of associated medical conditions such as diabetes may aid in diagnosis.
- Physical examination - may reveal enlarged neck nodes and an abdominal mass.
- Blood tests - show the presence of anemia.
- Liver function tests - may provide information about the type of jaundice.
Diagnostic Imaging
- Ultrasound provides a real-time visualization of the underlying abnormality and is usually the first choice as it is non-invasive and comparatively inexpensive.
- CT Scan Abdomen - Multiple x-ray images are taken and reconstructed in a computer.
- Magnetic Resonance Imaging (MRI) of the Abdomen - Using magnetic waves, detailed images are created.
- Positron Emission Tomography (PET Scan) - Injection of radioactive glucose into veins. This is taken up by the cancer cells and helps determine the extent of spread.
- Endoscopic Ultrasound and Biopsy - Using a thin, flexible tube, an ultrasound probe is passed into the stomach to obtain images. During this procedure, a sample of the tumor (Biopsy) may also be obtained.
- Endoscopic Retrograde Cholangio Pancreatography (ERCP) - A flexible endoscope is passed into the stomach. Through the endoscope, contrast medium is injected into the bile ducts using a catheter. These are then visualised radiologically. During this procedure, a sample of the tumor (biopsy) may also be obtained.
- Pancreatic Biopsy - A sample of the growth may be obtained by injecting a needle into the pancreas through the skin (fine needle aspiration). The sample can also be obtained using endoscopic ultrasound guidance.
A biopsy is sent for histopathological examination (HPE) and other studies. It provides definitive evidence of the disease.
Staging of the Disease
- Staging Laparoscopy – Using a laparoscope (thin tube passed into the abdomen via an incision), the surgeon visualizes the abdominal cavity and determines the stage of the disease to plan treatment.
- Diagnostic Imaging to determine the extent of spread
- CA 19-9 levels in blood are measured. It is a tumor marker used in pancreatic cancer.
- Levels may be measured before, during and after treatment to gather the response to therapy.

How do you Treat Pancreatic Cancer?
Treatment of the disease depends on several factors such as the stage of the disease, location of the tumor, the age and condition of the patient, and their willingness to accept the options put forth.
Treatment options include surgery, chemotherapy and radiation.
A. Surgery
Surgery is generally considered as a cure if the tumor is confined to the pancreas. In inoperable cases, it is done only as a palliative option to keep the patient comfortable and free from pain.
Tumor of Head of Pancreas
For tumors involving the head, the Whipple’s procedure (procedure is also called pancreatoduodenectomy) is performed. The gall bladder and a part of the bile duct may also be removed. The remaining parts of the pancreas and small intestine are reconstructed to allow passage of food and digestion.
Tumor Body and Tail of Pancreas
Surgery to remove the affected part of the body or tail may be performed (distal pancreatectomy). In some cases, the spleen may also be removed.
B. Chemotherapy
- Chemotherapy is the use of drugs to kill cancer cells. They may be administered orally or intravenously and singly or in combination.
- Chemotherapy may be combined with radiation (chemoradiation) to treat locally invasive inoperable tumors of the pancreas.
- Chemoradiation may also be tried after surgery to reduce the risk of recurrence.
- In patients with inoperable and advanced metastatic disease, chemotherapy may be used alone or in combination with targeted drug therapy.
C. Targeted Drug Therapy
This uses drugs that target specific defects within the tumor cells. Treatment is aimed at preventing their growth and division. For this purpose, the drug Erlotinib is used with chemotherapy in patients with advanced disease.
D. Radiation
Its role in pancreatic cancer remains controversial. It has been recommended as an option to shrink the tumor before surgery in resectable tumors. However its role in non-resectable tumors remains unresolved. Some recommend it as adjuvant treatment following curative surgery but its role still remains controversial.
E. Role of Clinical Trials
Clinical trials test out new unproven drugs, new forms of therapy such as gene therapy, or new approaches to existing treatment. They don’t guarantee a cure and may have unexpected side effects also.
However cancer clinical trials are closely monitored to ensure safety. Patients are offered access to treatment that is otherwise unavailable.
The patient and the family may weigh their options and decide to accept or reject the offer of a clinical trial.