- Harrison’s textbook of internal medicine – 18th edition
What is Prolapse of Intervertebral Disc?
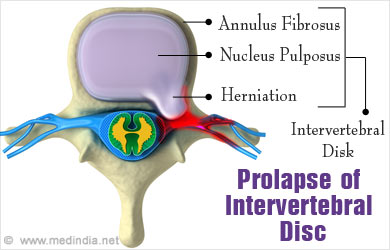
Prolapse of intervertebral disc or spinal disc herniation or herniated disc is a condition where the central gelatinous part of the intervertebral disc moves out of its position. It is usually a consequence of gradual changes in the disc, which ultimately lead to its prolapse.
The commonest level of disc prolapse is between the fourth and fifth lumbar vertebrae in the lower back and between fifth and sixth cervical vertebrae in the neck region. The most common symptom is low back pain and the pain radiates down the back of leg called sciatica or sciatic pain.
Relevant Anatomy
As the name suggests, an intervertebral disc is a cushion that lies between two vertebrae. It consists of two distinct components, nucleus pulposus and annulus fibrosus. The annulus fibrosus is a structure composed of concentric rings of fibro-cartilaginous tissue. It encloses the nucleus pulposus, which is a gelatinous layer in the middle. The intervertebral discs are supported posteriorly by the posterior longitudinal ligament and anteriorly by the anterior longitudinal ligament. These ligaments are attached to the vertebrae.
How does Prolapse of Intervertebral Disc Occur?
Several changes in the intervertebral disc over a period of time lead to its prolapse. The changes are as follows:
- The nucleus pulposus gets softened and fragmented.
- The annulus fibrosus becomes weak and the nucleus tends to protrude out of it. The protruded nucleus may press on the adjacent nerve roots as they emerge from the vertebral column. A further protrusion causes the nucleus pulposus to lie under posterior longitudinal ligament. Finally, a part of the nucleus gets separated from its parent disc and forms a free fragment in the vertebral canal.
- Later on, the part of nucleus pulposus that remains in between the vertebrae becomes fibrosed. The separated part also gets fibrosed and hardened due to calcification. The affected vertebral joint becomes prone to arthritis.
What are the Causes of Prolapse of Intervertebral Disc?
Causes of disc herniation include the following:
- Degenerative changes in disc due to aging. However, in very old individuals, the discs may undergo fibrosis and therefore, prolapse is rare
- History of preceding trauma such as a fall or a blow to the back
- Lifting something heavy which puts pressure on the back
- Pushing something heavy
- Contact sports which can lead to injury, so athletes are at greater risk of disc prolapse
What are the Symptoms and Signs of Prolapse of Intervertebral Disc?
The symptoms and signs of herniated disc include the following:
- Low Backache: Herniated disc causes severe backache, especially with movement. The spine is held rigid and in extreme cases, patients may not be able to do daily routine work. In prolapse occurring over a prolonged period, the pain is dull and worsens with exertion, forward bending, or sitting or standing in one position for a long time. It reduces with rest.
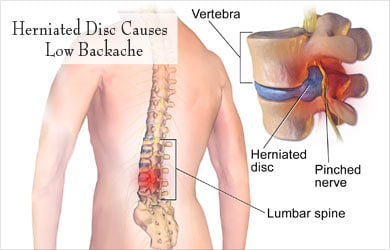
- Sciatic Pain: Sciatic pain is the pain associated with low back pain which radiates down through hips to thighs and ultimately towards legs. Depending on the nerve root compressed, the pain may even radiate to calf muscles, heel, front of leg and ankle. If the disc prolapse occurs at the upper back, the pain may radiate to the front of the thigh. The radiation may begin with walking and is relieved by rest.
- Neurological Symptoms: The patient may complain of ‘pins and needles sensation’ in the area supplied by affected nerve root. There may also be numbness or muscle weakness of the leg or foot. A more serious form of neurological disease is the appearance of bowel and bladder dysfunction due to compression of the lower nerves within the spinal cord. This condition is referred to as cauda equina syndrome.
How to Diagnose Prolapse of Intervertebral Disc?
The diagnosis is made by clinical examination and investigations.
- Clinical Examination
- Posture: A patient with a prolapsed intervertebral disc stands with a rigid and flattened lower back with the entire trunk shifted forwards on hips. The trunk may be tilted to one side; the tilt becomes worse while bending forwards.
- Straight Leg Raising Test (SLRT): The patient is asked to raise the leg straight while lying down. If pain is experienced at 40° or less, the test is considered positive and is suggestive of nerve root compression.
- Neurological Examination: It is done to evaluate muscle weakness, sensory loss or reduced reflexes in the area of distribution of the affected nerves.
- Investigations
- MRI Scan: This is the preferred test since it shows soft tissues very clearly.
- CT Scan: Normally, posterior border of the intervertebral disc appears concave on CT scan. In the case of disc prolapse, it appears flat or convex. The herniated disc material can also be seen pressing upon the nerve roots.
- Plain X-ray: A plain X-ray usually cannot detect changes in recent disc prolapse, but can be used to detect bony changes in prolonged disc prolapse cases or to rule out other causes of pain.
- Myelography: In this test, a dye is introduced in the spinal canal. It is rarely used now, but it is still performed if other tests like CT scan or MRI are not available
- Electromyography: This testis used to study the electrical activity of the muscle, and thereby localize the nerve affected.
How to Treat Prolapse of Intervertebral Disc?
Two treatment modalities can be used as follows:
- Conservative Treatment: The patient is advised rest on a hard bed for 2-3 weeks. He/she is given pain killers along with muscle relaxants to relieve the muscular spasms and pain. Also, physiotherapy with hot fomentation and gentle arching exercises are done. Patients who do not respond to the initial conservative treatment are considered for surgery.
- Operative Treatment: Procedures such as fenestration operation, laminotomy, hemi-laminectomy and laminectomy may be adopted to surgically treat disc prolapse.