- Serious complications in scrub typhus - (http://www.ncbi.nlm.nih.gov/pubmed/10496165)
- Diagnosis of Scrub Typhus - (http://www.ncbi.nlm.nih.gov/pmc/articles/pmc2829893/)
- Orientia tsutsugamushi in Eschars from Scrub Typhus Patients - (http://wwwnc.cdc.gov/eid/article/12/7/pdfs/05-0827.pdf)
- Scrub typhus during pregnancy and its treatment: a case series and review of the literature - (http://www.ncbi.nlm.nih.gov/pubmed/17123995)
What is Scrub Typhus?
Scrub typhus or mite-borne typhus is an infectious disease caused by a specific type of bacteria called Orientia tsutsugamushi. It is spread and maintained by the larvae of mites. These larvae are called “chiggers”. They bite human skin and leave a characteristic mark called an "eschar" (scar). The disease presents nonspecifically, but may rapidly progress to dreaded complications such as lung and liver failure. "Typhus" means fever with stupor, or smoke. It was a dreaded disease in the pre-antibiotic era, causing the deaths of thousands of soldiers during World War II. It is said that during Napoleon’s retreat from Moscow, a greater number of soldiers were killed by typhus than by the Russian army.

This disease is common in the Asian continent, so much so that it has to be considered in any patient in rural Asia who has an unexplained fever. The area of maximum occurrence is a triangle between Japan, Russia and Australia, called the "Tsutsugamushi Triangle". In India, scrub typhus is often seen in the Southern states Andhra Pradesh and Tamil Nadu.
What Causes Scrub Typhus?
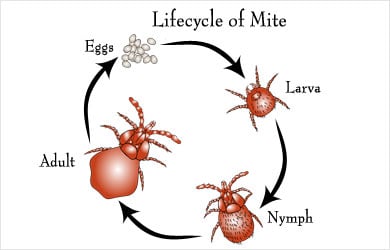
Scrub typhus is caused by a bacterium called Orientia tsutsugamushi. It has the ability to survive inside the cells of our body. It is transmitted to humans by the larva of a mite, called a “chigger”. These mites maintain infection among themselves by passing the bacteria onto their offspring, but only the “larval stage” of the mite (one of four life cycle stages: egg, larva, nymph and adult) can transmit the bacterium to human beings.
Scrub literally means a specific type of vegetation, somewhat similar to woods, and it is where the mite is most often found. But it can also be seen in semiarid areas and deserts. Mites can also spread rickettsial pox.
What are Symptoms and Signs of Scrub Typhus?
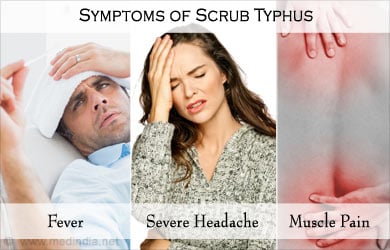
The disease begins to manifest itself approximately 10-12 days after the chigger bites. The first symptom is usually a small raised mark at the site of the bite, which later becomes a dried out, blackish spot called an “eschar” (scar). It is most often found near the groin, armpits, neck and in the external genital regions. There may be an associated rash around the eschar, and the lymph nodes near the affected area may become swollen. Fever may start abruptly, accompanied almost always by severe headache, chills, muscle pain and cough. There may also be redness of the eyes, drowsiness, vomiting, and shin pain.
The presence of an eschar is a valuable diagnostic clue to the physician, and it is present in approximately 50% of affected individuals. There may be evidence of liver enlargement and congestion of the lungs on physical examination.
Sometimes, in case of advanced disease, there may be features of lung involvement such as intractable cough, shortness of breath and drowsiness. Severe lung involvement may lead to Acute Respiratory Distress Syndrome (ARDS) which may require ICU admission and ventilator support. Other manifestations of severe disease include involvement of the lungs, the kidneys, the brain and inappropriate clotting of blood, called DIC (disseminated intravascular coagulation) which is a dreaded complication.
How to Diagnose Scrub Typhus?
The diagnosis of scrub typhus is aided by the presence of the characteristic “eschar” (scar). It is difficult to diagnose from the clinical findings alone, as they are nonspecific, and a high degree of suspicion is required, particularly in endemic areas. Many laboratory tests can aid in diagnosing scrub typhus, including general and specific tests.
General tests:
- Complete blood count may show a large number of white blood cells and a low level of platelets.
- Liver and kidney function tests may be abnormal.
- Chest Xray is often necessary and may reveal features of lung involvement.
- Ultrasound of the abdomen may be required to confirm enlargement of the liver or spleen.

Specific tests:
- ELISA for detection of antibodies to the bacterium, which is commonly used nowadays.
- Indirect Immunofluorescence antibody test, which is the gold standard.
- Weil-Felix test, which is not used so often now.
- Blood culture
- PCR (polymerase chain reaction)
How to Treat Scrub Typhus?
Treatment of scrub typhus should be initiated early, based on clinical suspicion. The recommended treatment is doxycycline 100 mg twice daily orally for 7 to 14 days based on the severity of the illness. In children and pregnant women, azithromycin 500 mg once daily is used. In places where there is resistance to doxycycline alone, azithromycin may be used in combination with rifampicin.
Complications such as ARDS may require invasive ventilation and supportive care in the ICU setting.
Treatment guidelines as suggested in the Indian Medical Gazette include doxycycline as the treatment of choice in adults, and azithromycin during pregnancy. Alternatives to doxycycline include chloramphenicol, telithromycin, roxithromycin, rifampicin and levofloxacin. It is important to note that rifampicin should not be used as a single agent.
Complications of Scrub Typhus
- Pneumonitis
- Acute Lung Injury (ALI)
- Acute Respiratory Distress Syndrome (ARDS)
- Acute Kidney Injury (AKI)
- Myocarditis
- Septic shock
- Disseminated Intravascular Coagulation (DIC)
- Scrub typhus in pregnancy - It may cause preterm labour and Neonatal Respiratory Distress Syndrome.
What are the Risk Factors for Scrub Typhus?
- Farm and forest workers
- Living at the edge of villages
- Wearing short sleeves
- Working bare hands
- Immune deficiency
Risk factors for severe infection:
A. Bacterial factors
- Strain of bacterium causing the disease
- Molecular variations
- Antibiotic resistance
B. Host factors
- Genetic factors
- Deficient immunity
- Underlying diseases
Health Tips
- Avoid places where mites are known to be present in a large number
- Wear protective clothing when travelling to an endemic area. Long sleeved clothes have been shown to be a preventive factor from getting infected.
- Apply mite repellents to exposed skin e.g. diethyl toluamide.
- People who have risk factors and who have to work in an endemic area can be given once weekly dose of doxycycline.






