- Cutaneous Tuberculosis - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2923933/)
- Cutaneous Tuberculosis - (https://www.ncbi.nlm.nih.gov/books/nbk482220/)
- Update on Cutaneous Tuberculosis - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4230662/)
- Cutaneous Tuberculosis: Diagnosis, Histopathology and Treatment - Part II - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4148266/)
- Cutaneous Tuberculosis: Epidemiologic, Etiopathogenic and Clinical aspects - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc4008050/)
What is Skin Tuberculosis?
Skin tuberculosis (TB) or cutaneous TB is a rare extra-pulmonary form of tuberculosis and accounts for only 1 to 1.5% of
Skin Tuberculosis History
- Laennec first documented cutaneous TB in 1826. Since the lesions were often found in individuals who performed dissections or autopsies, they were called prosector’s warts.(1✔ ✔Trusted Source
Cutaneous Tuberculosis
Go to source) - In the 1800s and early 1900s, skin TB was a major cause for concern in public health, which dissipated with the advent of the
BCG (Bacille Calmette Guerin) vaccine , improved personal hygiene, and beneficialchemotherapy . - However, with the advent of diseases, such as HIV, malignancy chronic disease, the increase in immune-suppressing treatments, and drug-resistant cases of tuberculosis, there has been a resurgence of skin tuberculosis from the mid-1990s.
- Some of the common pathological types of cutaneous TB are lupus vulgaris, cutaneous miliary tuberculosis, scrofuloderma, verrucosa cutis, and papulonecrotic tuberculids.
What are the Causes of Skin Tuberculosis?
Skin tuberculosis is a prolonged infection caused by the following 3 types of bacteria
- Mycobacterium ovis
Mycobacterium tuberculosis - Calmette-Guerin bacillus – BCG (occasional)
What are the Factors that Influence Occurrence of Skin Tuberculosis?
There are different factors that can influence the presence of skin TB.(2✔ ✔Trusted Source
Cutaneous Tuberculosis: Epidemiologic, Etiopathogenic and Clinical aspects
Go to source)
Environment: In Asia and Europe, lupus vulgaris is the common form of skin TB. In Brazil, it is scrofuloderma.
Virulence: The bacteria modify their presence and release certain proteins or lipids based on the surrounding environment and based on the drugs used. There are no confirmed virulence factors yet.
Route of infection: This could be either endogenous or exogenous.
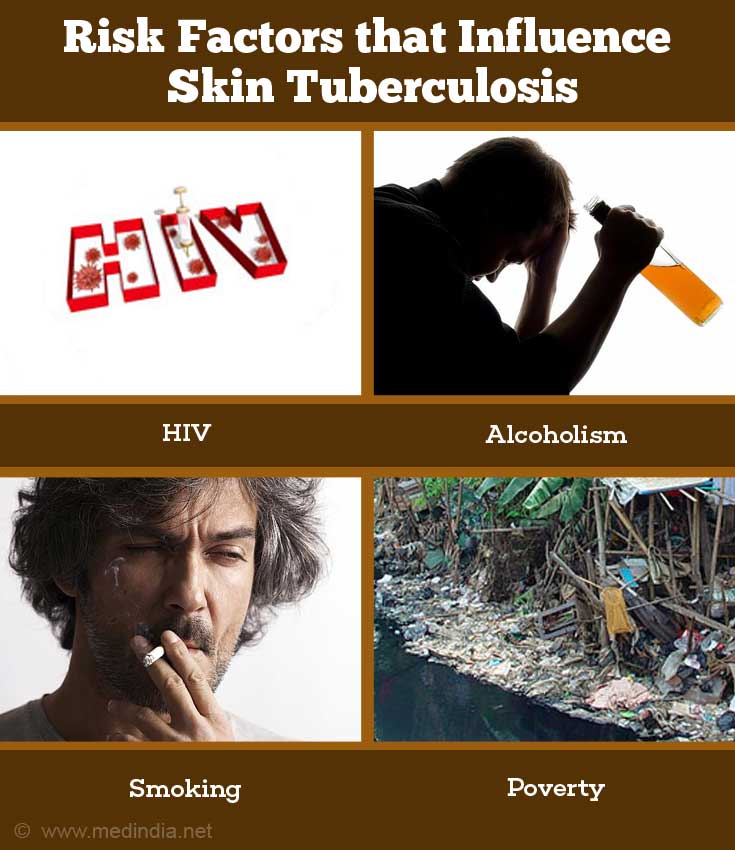
Patient risk factors: Cutaneous TB can occur in people of all ages, those with low immunity due to other infections such as HIV or alcoholism, smoking as well as in children with reduced immune resistance. Poverty, malnutrition, and overcrowded living conditions promote spread of the disease.
Drug resistance:
Host immunity: It goes without saying that an individual with a strong immune response can handle Mycobacterium tuberculosis infections without exhibiting the disease. However, reduced immunity in the body will predispose the individual to infections.
What are the Signs and Symptoms of Skin Tuberculosis?
The signs and symptoms of cutaneous TB vary based on the type of infection. Cutaneous TB is classified as exogenous or endogenous cutaneous TB.(3✔ ✔Trusted Source
Cutaneous Tuberculosis
Go to source)
Endogenous infections occur through the lymphatic system or through the blood. They occur secondary to a primary infection at another site.
Endogenous tuberculosis - Some of the endogenous forms of skin tuberculosis include
Papulonecrotic tuberculids – These tuberculids are skin infections due to either Mycobacterium tuberculosis infection or by another organism. The individual suffers from unusual loss of energy, fever, and weakness in the body. There are lesions on the buttocks, ears, face, trunk. Lymphadenitis may or may not be associated with the papulonecrotic tuberculids.
Erythema induratum of Bazin (EIB) –Women who are young and in their middle age, are prone to skin infection in the posterior area of the thighs and legs. The lesions are frequently painful, have a purple color, and regress on their own leaving scars. However, there is recurrence once every 3 to 4 months. While this infection is associated with tuberculosis, another skin infection erythema nodosum is often confused with EIB. However, erythema nodosum is caused by numerous infectious agents besides M tuberculosis.
Scrofuloderma – This condition is observed in children in India and Brazil. Patients with scrofuloderma are immune competent and show a positive Mantoux test. This infection spreads from an area that contains the TB infection (bone or lymph nodes) and lodges itself in the axillary regions, areas where there is less soft tissue between the bone and skin (e.g. the foot) or in the cervical regions. The inflammation develops into painless cold abscesses with purple plaques, which then spontaneously involute creating scars.
Lupus vulgaris – This is a common form of cutaneous TB in India and Europe. The lesions are either ulcerated or vegetative lesions, or nodules. They form reddish-brown plaques and are observed in legs, face, buttocks, and in the cervical region. As the lesion grows, there is loss of colour in the centre of the lesion. If left untreated, cancer develops.
Orificial tuberculosis – Senior citizens and middle-aged adults who suffer from advanced stage genitourinary, lung, or intestinal tuberculosis are affected with orificial TB.
The lesions are red to yellow and painful and ulcers develop. The outcome of this condition is not good since it is associated with primary disease elsewhere in the body.
Acute miliary tuberculosis – A rare form of cutaneous TB, acute miliary TB occurs in children and immune-compromised individuals. The characteristic symptoms are asthenia, fever, weight loss, and anorexia. White to purple plaques form in the lesions. When the plaques break down, crusts form, and eventually dry out to form scars. Liver and spleen are some of the organs that are affected, and when the immune system fails, death can occur.
Tuberculous gumma – This type of infection affects immune-compromised individuals and children who are malnourished. Lesions that form ulcers occur in the extremities and the trunk region. The outcome of this infection is not good because it tends to occur in immune-compromised individuals. They are also observed in
Exogenous infections – Exogenous infections occur due to an accidental exposure to the infection through a cut, crack, or wound on the skin.
There are 2 types of exogenous infections:
Tuberculous chancre – This is a rare form of cutaneous TB found in areas where there is no vaccination. Children are most likely to suffer from this infection. These infections occur due to tattoos or surgical procedures. The lesions are firm, painless, slowgrowing nodules or papules. Ulcers may develop. These lesions may resemble those of lupus vulgaris or scrofuloderma.
Tuberculosis verrucosa cutis (TVC) – Physicians and anatomists are exposed to Mycobacterium tuberculosis infection through injured skin. Walking barefoot with exposed skin in tropical areas can make an individual prone to infection. The infection begins as painless papules with a purple halo in toes and fingers, and then grows outwards to form plaques. Ulcers rarely form. Elephantiasis and other secondary bacterial infections are potential complications.
How do you Diagnose Skin Tuberculosis?
In general, diagnostic tests are not as sensitive to cutaneous TB. Hence, physicians must pay special attention to the symptoms and conduct the necessary diagnoses.(4✔ ✔Trusted Source
Update on Cutaneous Tuberculosis
Go to source)
The diagnosis of skin tuberculosis is based on a thorough physical examination and a medical history of the patient. In addition the following tests will have to be performed:
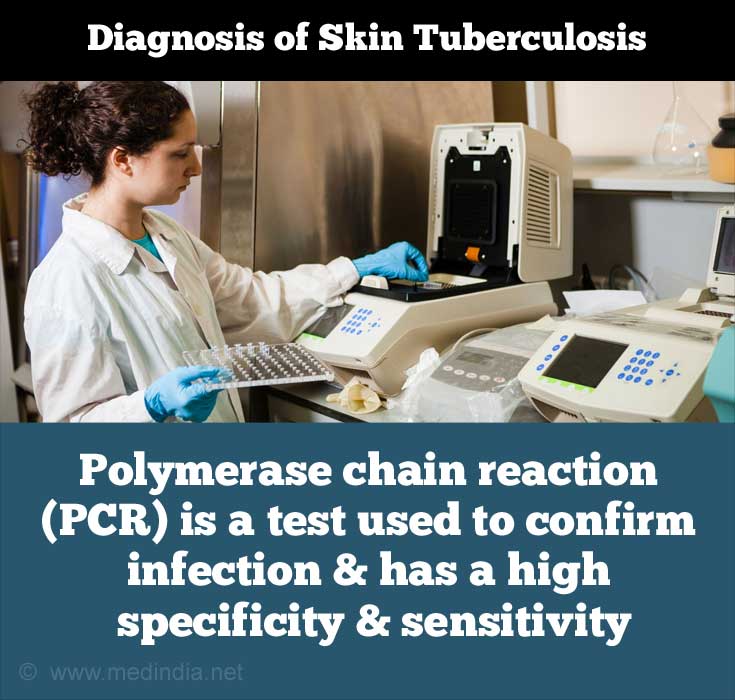
- Laboratory tests (e.g. Polymerase chain reaction [PCR], QuantiFERON tuberculosis Gold (QFT-G) - Interferon-gamma release assays, and Mantoux tests or Tuberculin sensitivity test
- Chest x-rays – to detect
pulmonary tuberculosis - CT scans
- Sputum, blood, urine culture samples
- Skin biopsy – specific stains identify the bacilli except in the case of lupus vulgaris
- Bone scans
- Identifying acid-fast bacteria in stained smear from skin lesions
- Mantoux tests are not reliable in the detection of miliary tuberculosis and papulonecrotic tuberculids but are good in confirming lupus vulgaris and scrofuloderma.
- In the absence of technology, patients are given
anti-TB medications if there is a faint suspicion of the infection. - Polymerase chain reaction (PCR) is a test specifically used to confirm cases of multibacillary infection and has a high specificity and sensitivity. However, due to the high costs, it is not a favored test unless there is a negative result from a histological assay.
How do you Treat Skin Tuberculosis?
- The basic treatment regimen is called RIPE (
rifampicin, isoniazid , pyrazinamide, ethambutol) used in the treatment of skin TB where there are 2 stages in treatment.(5✔ ✔Trusted Source
Cutaneous Tuberculosis: Diagnosis, Histopathology and Treatment - Part II
Go to source)
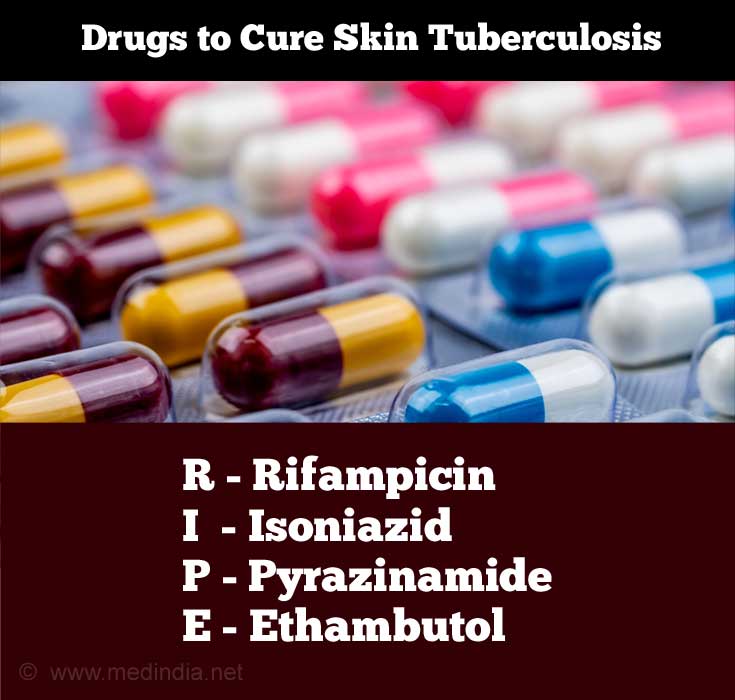
- The first stage (bactericidal) aims to reduce the Mycobacterium tuberculosis bacterial count. This normally takes 8 weeks following which the patient is not considered to be infectious.
- The second stage (sterilization) focuses on removing the remaining resident bacteria. Treatment typically lasts 6 months.
- In cases that are caused by atypical mycobacteria, certain
antibiotics are prescribed. - Surgery (incision and draining the abscesses, debridement) is recommended in cases that are not cured by drug therapy.
- It is important that patients follow the prescribed treatment regimen to avoid development of drug resistance.
- In India, cutaneous TB is treated based on the Revised National Tuberculosis Control Program.
How do you Prevent Skin Tuberculosis?
The following measures may be adopted to prevent skin tuberculosis:
- Use of sterilized needles for cultural rituals or piercing ears or injections
- Effective identification and treatment of infected individuals to prevent spread by contact
- Consume boiled and
pasteurized milk - Practice better hygiene and nutrition
- BCG vaccine helps in preventing the spread of pulmonary TB