- VESTIBULAR REHABILITATION THERAPY (VRT) - (http://vestibular.org/understanding-vestibular-disorder/treatment/treatment-detail-page)
- HEARING & BALANCE - (http://american-hearing.org/disorders/balance-and-vestibular-rehabilitation-therapy/)
- Vestibular rehabilitation exercises - (http://www.brainandspine.org.uk/vestibular-rehabilitation-exercises)
- ABOUT VESTIBULAR DISORDERS - (http://vestibular.org/understanding-vestibular-disorder)
- Benign paroxysmal positional vertigo - (https://en.wikipedia.org/wiki/benign_paroxysmal_positional_vertigo#treatment)
- Vestibular Rehabilitation - (https://my.clevelandclinic.org/services/rehabilitation-sports-therapy/specialty-therapy-services/hic-vestibular-rehabilitation)
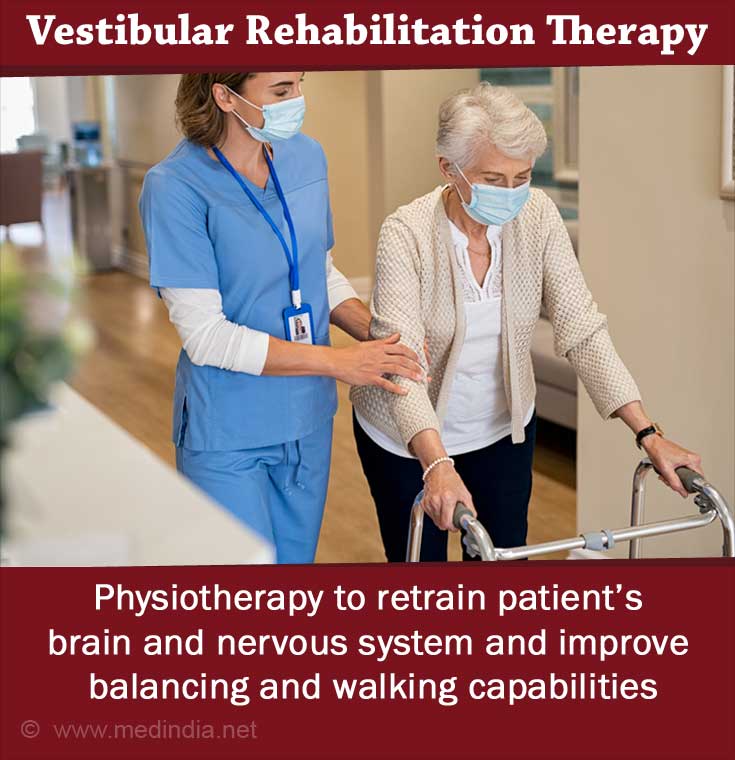
What is Vestibular Rehabilitation?
Vestibular rehabilitation involves improving on symptoms involving the vestibular disorders like dizziness, vertigo, visual disturbance or imbalance. Nausea, vomiting, fatigue and the inability to concentrate are secondary symptoms of vestibular disorders. The rehabilitation program uses specialized exercises to improve on gaze and gait stabilization.
The inner ear has two parts – the cochlea and the labyrinth. The cochlea receives sounds from the middle ear and converts it into electrical impulses, to be sent to the brain as sound signals via the cochlear part of the VIIIth cranial nerve.
The vestibule, or labyrinth, is responsible for the balance of the body. Problem with the inner ear (labyrinth) can lead to labyrinthitis. The vestibular system consists of three semicircular canals that converge and merge near the cochlea. The vestibular system coordinates with the visual system and this information, along with the sensations of the joints and muscles, is interpreted by the brain to create a sensation of balance. It gives information about the balance, equilibrium and orientation in three-dimension space. The signals about the position and balance are sent from the semicircular canals to the brain via the vestibular part of the VIIIth cranial nerve.
Any disorder in the vestibular system can result in symptoms like vertigo or dizziness confusion, the disorientation of position, loss of balance during walking, etc. Some of the vestibular disorders include:
- Labyrinthitis, also called vestibular neuritis, otitis interna, and vestibular neuronitis
- Menière’s disease affects the inner ear and the patient experiences symptoms of vertigo, loss of hearing
- Secondary endolymphatic hydrops
- Perilymph fistula
- Ototoxicity
- Acoustic neuroma is a benign intercranial tumor
- Disembarkment syndrome or Mal de débarquement
- Enlarged vestibular aqueduct
- Superior canal dehiscence
Autoimmune disorders, allergies and migraine-associated vertigo are some of the related vestibular disorders.
In most people, the disorder is permanent and vestibular function is restored in very few patients. Training other senses like vision and somatosensory, can help in compensation of body functions to maintain balance and people can lead a successful life.
Benign Paroxysmal Positional Vertigo
Benign Paroxysmal Positional Vertigo (BPPV) occurs when some of the calcium carbonate crystals normally embedded in the gel of the utricle dislodge themselves and migrate into the fluid-filled semicircular canals. This disturbance in the semicircular canals interferes with the normal movement of the fluids in response to the changes in the head positions and causes the vestibular system to send false signals of movement to the brain. These signals do not match with the inputs given by the vision and the proprioceptive senses and this false information is perceived by the brain as vertigo or dizziness. When the dislodged crystals make the brain believe that the person is moving even though they are not moving, the eyes try to move to coordinate, resulting in dizziness.
Further, the crystals are pulled downwards by gravity, causing unnecessary movements of the fluid in the semicircular canals.
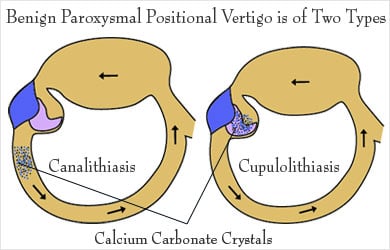
Benign Paroxysmal Positional Vertigo is of two types:
- Canalithiasis: In which the crystals can move freely in the fluid of the canal
- Cupulolithiasis: Crystals are thought to be “hung up” on the bundle of nerves that receive the sensation of fluid movement.
Symptoms of benign paroxysmal positional vertigo include vomiting, nausea, feeling faint, rotatory nystagmus, visual disturbance and vertigo. The nystagmus is typical where the top of the eyes rotates towards the affected ear in a beating or twitching fashion. Vertigo decreases with deliberate repetition of the provoking maneuver.
Patients do not experience neurological symptoms like numbness or weakness of muscles.
Medications do not seem to improve the symptoms of BPPV, but various types of exercises have proved that the condition can be stabilized and the patient with BPPV can control the symptoms so as to carry on the daily activities.
Vestibular Rehabilitation Therapy (VHR)
Vestibular rehabilitation therapy aims to overcome primary and secondary problems caused by vestibular disorders. This exercise-based program is personalized to improve vertigo, dizziness, enhance gaze stability and gait of a person with a vestibular disorder.
The symptoms that can be overcome by vestibular rehabilitation therapy include:
- Vertigo or dizziness
- Blurry vision and dizziness as a result of sudden head movement
- Stiffness, tightness or pain in the neck
- Gait instability, need to hold to wall or railing while walking
- Frequent falls
- Frequent headache
Vestibular rehabilitation therapy aims to improve in the following ways.
- Decreased risk of falling
- Improving on dizziness
- Improving stability in vision or gaze
- Improved balance
- Improved neck motion
- Better body strength
Indications for Vestibular Rehabilitation Therapy
Specific conditions of the vestibular system determine the type of intervention program. The following conditions can improve with vestibular rehabilitation therapy.
- Unilateral vestibular disturbance, such as in vestibular neuritis or acoustic neuroma
- Bilateral loss as in gentamicin toxicity
- Benign paroxysmal positional vertigo
- Post-traumatic vertigo
- Multifactorial disequilibrium, as seen in senior citizens
Vertigo caused by certain conditions is unlikely to improve with vestibular rehabilitation therapy.
- Low blood pressure
- Migraine associated vertigo
- Side-effects of medications
- Anxiety or depression
- Meniere’s disease
- Perilymphatic fistula
- Transient ischemic attacks
Assessment for Vestibular Rehabilitation Therapy
History:
Information about the patient’s condition is taken and the following points are noted:
- Symptoms noticed by the patient–type and intensity.
- Effect of symptoms on the daily activities of the patient.
- Previous treatments taken if any.
- Use of medications for the condition or otherwise
- Fall history
- Current activity levels of the patient.
Assessment of Vision and Eye Movement:
- Eye-head coordination tests – movement of eyes along with head movements
- Ability to track a moving object without moving the head.
- Using eye charts to examine the ability of eyes to focus during head movements
Assessment of Vertigo:
- Frequency and severity of dizziness symptoms
- Duration of dizziness episodes
- Other related symptoms such as nausea, sweating and nystagmus.
Assessment of Balance and Gait:
- Effects of controlled postural sway in different directions.
- Checking static balance skills like standing on one leg.
- Turning the head while walking.
- Suddenly changing the speed or direction of walking.
- Walking heel-to-toe (tandem walking)
- Ability to walk backward or sideways.
- Ability to stand steadily with eyes closed on a solid surface and soft surface.
- Coordination of leg and trunk movements for balance control.
- Ability to hold the head steady to maintain balance during movements of other body parts.
Assessment of the Musculoskeletal Movements:
- Range of motion
- Coordination of muscles during movements of the limbs
- Sensation of movement and position
- Muscle strength
Tests to Measure Balance:
Measuring balance is done on subjective assessment like questionnaires like Dizziness Handicap Inventory and Activities-Specific Intrinsic Variability. Some measures that can help understand the extent of the balance disorder include posturography, ENG testing, mobility oriented tests, rotatory chair testing, etc.
Techniques and Exercises of Vestibular Rehabilitation Therapy
General Vestibular Rehabilitation Therapy
Vestibular rehabilitation therapy is beneficial for patients with certain types of vestibular disorders. General vestibular rehabilitation therapy involves simple exercises that help in improving the symptoms of vestibular disorders:
- Habituation: Habituation exercise is prescribed for patients with increased dizziness due to sudden movements, changing the position of the head or visually stimulating environments.
An Example of Habituation Exercise: The patient is asked to focus on a target in front of him and move his head side to side, without taking his eyes off the target. These exercises can be increased regarding speed. Various positions like sitting, standing, lying down, walking, etc. must be tried out and practiced to get the eye movements habituated.
Alternately, the target can be moved and the patient is asked to focus on the target, without moving his head.
- Gaze Stabilization: These exercises help in better control of eye movements and eye-head coordination.
An Example of Gaze Stabilization Exercise: Two targets are placed at the eye level or wall, at about 3 to 4 feet apart. The patient looks at one target, moves the head without moving the eyes, to align with the other target.
- Balance Training: Improving steadiness is the main goal of balance training exercises so that daily activities are not disturbed.
The exercises include paying attention to other cues such as vision or positioning of hands or feet to maintain balance. The patient is trained to walk against real obstacles like walking on an uneven surface, walking in a dark place, etc.

The clinical assessment of the patient and the information from the tests and imaging studies form the basis for making a customized exercise and therapy plan. The patient and the caregiver are educated about the goals, purpose of the exercises and what to expect from the therapy program. The patient is also taught to do the exercises at home.
Specific Vestibular Rehabilitation Therapy
Specific exercises are prescribed based on the underlying pathologic condition and the symptoms presented. Benign paroxysmal positional vertigo can be improved with various exercises performed in the doctor’s office, like Epley maneuver, Semont maneuver and Cawthorne-Cooksey Exercises.
Epley Maneuver:
Epley maneuver is a canalith repositioning procedure. It involves sequential movement of the head into four positions. The patient stays in each position for about 30 seconds. Once the patient is familiar, he can do it at home. Steps to perform Epley maneuver are:
- Patient sits in upright position, with legs extended and head rotated 45 degrees towards which rotational nystagmus occurs.
- The patient is quickly forced down backward by the clinician, to a supine position. The head is still extended towards the same side, but with 30-degree extension. The patient remains in this position for about 1 to 2 minutes.
- The patient’s neck is extended to 30-degrees, while the head is rotated 90 degrees so that opposite ear is towards the floor. This position is maintained for about a minute or two.
- From the supine position, the patient rolls so that he lies on his shoulder, and rotates the head another 90 degrees. The patient is now looking downwards at a 45-degree angle. This position is maintained for about 1 to 2 minutes.
- The patient is slowly brought to a sitting posture, with the 45-degree head rotation. This position is held for about 30 seconds.
The patient may experience dizziness at any or all the steps, but the whole procedure is repeated 2 to 3 times. The patient may be provided with a soft collar to be worn for the day after exercises.
Semont Maneuver:
- The patient sits on a table with legs hanging down. The clinician turns the patient towards the side opposite to the rotational nystagmus, at a 45-degree angle.
- The patient is then quickly turned to lie on the affected side, with the head turned up 45-degrees. This position is maintained for about 3 minutes and allows the calcium debris to move towards the apex of the ear canal.
- A quick movement of the patient is done to make him lie down on the unaffected side, now the head facing 45-degrees downwards. This position is also maintained for about 3 minutes. The debris now moves towards the exit of the ear canal.
- The patient is now slowly brought back to the sitting position, making the debris fall into the utricle of the canal, thus decreasing the symptoms of vertigo.
Cawthorne-Cooksey Exercises
The aim of this procedure is to relax the neck and shoulder muscles. Cawthorne-Cooksey exercises also help train the eyes to move independently of the head. The exercises involve practicing good balance in daily activities and practicing head movements that cause dizziness.
Initially, dizziness may get worse for a few days after the start of the exercises, but when practiced regularly, they help in improving general coordination and encourage natural unprompted movements.
Exercises may include the following, based on the individual problems and symptom presentations.
- Eye movements can be done in sitting, lying down or standing positions. Eye movements are done to look up and down and from side to side, without moving the head. Focusing on an object or finger moving towards and away from the patient is done. Head movements like bending forwards and backward, and side to side, are done, without taking eyes off from a focus object.
- Shoulder shrug and circular movements are done. Bending forward or side to side to pick up objects from the ground is a part of the exercise.
- Changing to sitting and standing positions with eyes closed and then, with eyes open. Throwing a ball from hand to hand, so that the ball goes above eye level and then below knee level helps in eye-hand coordination.
- Walking across the place with eyes open, walking up and down a slope with eyes open, and walking up and down stairs with eyes open, are some of the exercises that help in the eye-head coordination and also coordination of the musculoskeletal system in maintaining balance.
- Games that involve stooping, stretching and aiming, like bowling, tennis, etc also help in improving symptoms of vestibular disorders.
Other exercises like Brandt-Doroff exercises and roll maneuver are also done.
Factors that can Limit the Success of Vestibular Rehabilitation Therapy
- Sedentary lifestyle
- Pain
- Presence of other medical conditions
- Emotional reactions to the disorder or in general









