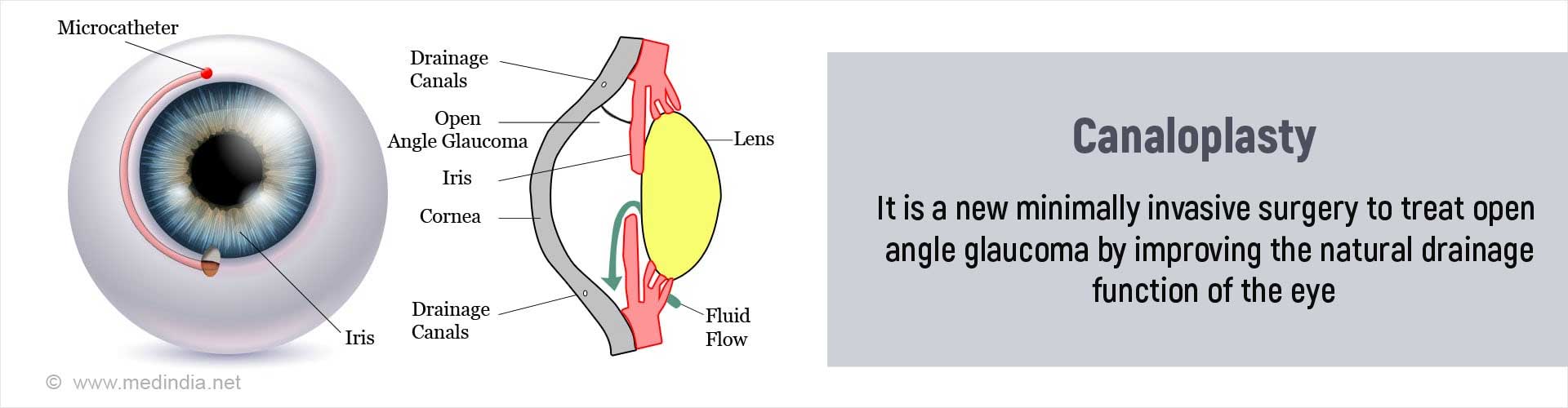
What is Canaloplasty?
Canaloplasty is a newer surgical technique that aids drainage of aqueous humor via the natural outflow pathways by dilating Schlemm's canal (SC). Since this is a non-penetrating procedure, that is, it does not involve entering in to the anterior chamber (space between the cornea and the iris) it is believed to be a safer option with fewer complications compared to traditional glaucoma surgeries.
Canaloplasty is a minimally invasive and non-penetrating procedure that has evolved from the similar viscocanalostomy procedure done for open angle glaucoma.
The incidence of complications is much lower, and the procedure involves fewer follow up visits to the doctor compared to trabeculectomy, which is the gold standard in treatment of open angle glaucoma.
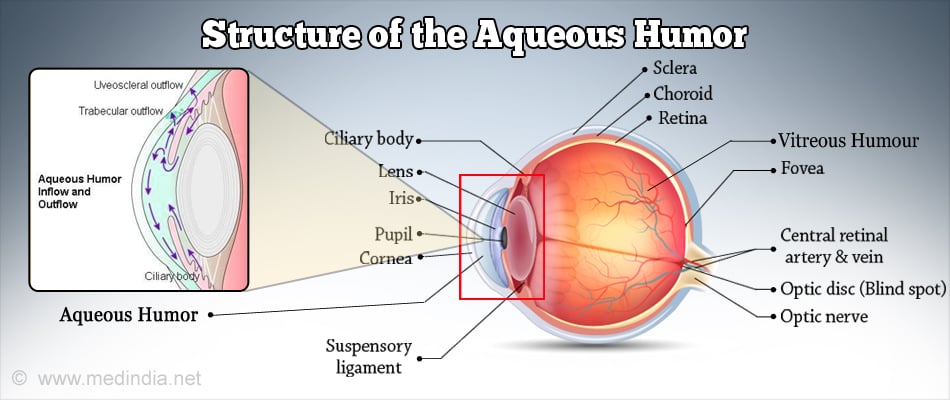
Aqueous humor Aqueous humor is the fluid present in the anterior segment of the eye, and which helps to maintain the intraocular pressure
The production of aqueous humor and its drainage occur at an equal rate in the eye. Any small change in either function can have a large change in the intraocular pressure. Aqueous humor is produced in the ciliary body and drains via a sieve like tissue called the trabecular meshwork in to a tube like structure called the Schlemm’s canal, from where the aqueous passes via collector channels in the sclera into the episcleral veins.
That is why most glaucoma surgeries involve the trabecular meshwork and Schlemm’s canal.
Glaucoma and Canaloplasty Overview
Glaucoma refers to a type of optic nerve involvement that is most commonly due to a rise in intraocular pressure that may occur due to a variety of causes. The rise in intraocular pressure is due to inadequate drainage of the aqueous humor from the anterior chamber of the eye. This may occur because of a lack of access of the aqueous to the trabecular meshwork in narrow angel glaucoma, or due to increased resistance to aqueous flow in open angle glaucoma. Regardless of the cause, untreated glaucoma can lead to blindness that is irreversible.
Surgery is indicated in open angle glaucomas when medications no longer control the progression of the condition.
What are the Indications for Canaloplasty?
Canaloplasty is considered a safe and effective procedure in the following situations
- Primary open angle glaucoma (an adult onset glaucoma where the angle between the iris and cornea is open)
- Pseudoexfoliative glaucoma (glaucoma caused by the blockage of the trabecular meshwork by a protein containing material that is present in the eye and throughout the body.
- Pigmentary glaucoma (a type of glaucoma where the trabecular meshwork is blocked by pigment from the iris, and which is more common in young male myopes).
- Children with congenital glaucoma (glaucoma present from birth)
Some of the reasons to choose canaloplasty are in the above situations are:
- Canaloplasty is safe and effective in those undergoing cataract surgery or contact lens users.
- It is also an option in patients who have already undergone trabeculectomy surgery followed by recurrence.
- It is the preferred option in patients having active lifestyles and therefore will not be able to follow the rigorous postoperative care needed following a trabeculectomy.
- It is also safe in persons with an increased risk of bleeding or infection.
How do you Prepare before Canaloplasty?
Starting a few days before the surgery
- Your eye doctor will conduct a comprehensive eye examination that includes checking the visual acuity, presence of afferent pupillary defect, gonioscopy, slit lamp exam, dilated fundoscopic exam and visual field assessment.
- If it is agreed that you need a canaloplasty, then you will be given certain instructions to follow during the few days leading up to the procedure.
- You will be advised to stop smoking, stop certain medications you may be regularly taking such as blood thinners for a few days before the surgery.
- You should inform the doctor about other underlying conditions you may be having such as hypertension and diabetes and these have to be appropriately controlled.
- You will have to undergo routine blood and urine tests as well as a chest x-ray and an electrocardiogram (ECG) to evaluate your general condition and heart and lung function.
- The type of anesthesia best suited to you will be discussed although the surgery is usually done under local anesthesia.
Day before Surgery and Morning of Surgery
- You will need to get admitted to hospital on the morning of surgery.
- If you are being operated under local anesthesia, you may have a light breakfast early on the morning of the surgery. Confirm this from your doctor.
- The team at the hospital will confirm the procedure to be performed and the side to be operated. You will then be given a sterile gown to wear and shifted to the theater and asked to lie down on a table specially designed for eye surgeries.
What Happens during Canaloplasty?
- The anesthetic used can either be in the form of eyedrops or can be injected in the tissue around the eyeball.
- A conjunctival opening is made to expose the sclera.
- A scleral flap involving about half the thickness of the sclera is dissected and raised. The second deep scleral flap (that unroofs Schlemm’s canal ) is dissected down to about 90 % of the scleral thickness. The eye is decompressed and the deep scleral flap is then removed. A flexible microcatheter illuminated at its end is then passed into the Schlemm’s canal to enable its visualization.
- After the catheter has passed the full circumference of the Schlemm's canal, a suture is tied to the catheter which is removed by reversing its direction. While the catheter is being withdrawn, a small amount of viscoelastic material is injected into the Schlemm's canal every 2 clock hours. Once the suture comes out through the opening of the canal, it is cut off from the catheter, is tightened, and tied to pull the trabecular meshwork inwards and keeps the Schlemm's canal open. The suture now replaces the catheter in the lumen of the Schlemm's canal.
- The superficial scleral flap is sutured tightly to the adjacent sclera and the conjunctiva is closed.
- The eye may be covered with dressing and eye shield to prevent injury.
What Happens after the Procedure?
- Since the surgery is done under local anesthesia, you will be shifted to your room and kept under observation for a few hours.
- You will be discharged the same evening if your condition is deemed stable. You will need someone to drive you home.
- You will need to use antibiotic eye drops for a week and steroid eye drops for about 2-4 weeks to inflammation
- There are no specific dietary restrictions following this surgery.
- Doctor’s instructions about resuming routine activities and washing and bathing should be followed strictly.
- You may have to wear a plastic shield at night for a few days to avoid accidentally injuring the eye.
- You will need to return to the clinic for review checkup within a week and then as requested by your doctor.
Important Do’s and Don’ts Following Canaloplasty
- Use the eyedrops as recommended by your eye doctor
- You may bathe the next day but avoid water getting into your eyes for at least 2 weeks
- Strenuous activities should be avoided for 2-4 weeks after the procedure.
- Driving may be resumed after a week if vision permits.
- Eye makeup should be avoided for one month after the procedure
- Water related and contact sports including swimming and tennis can be resumed after a couple of weeks after discussion with your eye doctor. In both these activities, it is important to wear protective eye wear that does not press upon the eyeball, but rests on the bones surrounding the eyeball.
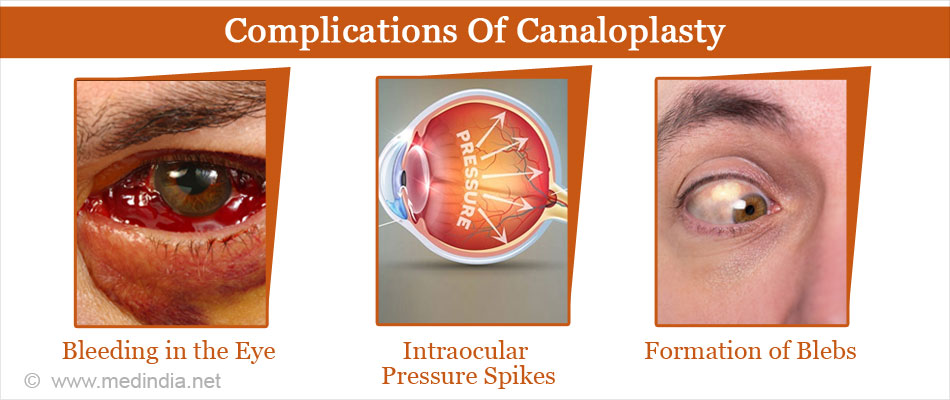
What are the Complications of Canaloplasty?
Canaloplasty is a very safe procedure although complications can occur. These include the following:
- Bleeding in the eye (hyphema) – This will usually resolve over time.
- Intraocular pressure spikes during surgery – In fact for a few days postsurgery the IOP will be higher than before surgery, but will normalise over a few days.
- Formation of ‘blebs’ – In a trabeculectomy procedure, formation of a stable bleb at the site of incision is desired, while in canaloplasty, it is considered a complication. Although the effectiveness of the canaloplasty is not diminished, these blebs can limit wearing of soft contact lenses.
- Descemet’s membrane detachment (a basement membrane in the cornea) – This can occur upon injection of the gel, if the canal is very tight. This may affect vision, though it improves over time. If this does not happen, the doctor may inject a gas bubble into your eye to press the Descemet’s membrane against the cornea.
- Failure of canaloplasty – Less than 1 in 20 canaloplasty surgeries may fail needing a traditional glaucoma surgery or trabeculectomy either intraoperatively or at an appropriate later date.
- Low IOP or hypotony – Rarely in around 1 in 200 cases of canaloplasty, the IOP may drop to less than 5 mmHg and can affect vision. This complication in encountered more often in trabeculectomy surgery.
- Infection – Endophthalmitis or infection of the eye may rarely occur and has to be treated with antibiotics injected into the eye.
What is the Prognosis (Outlook) of Canaloplasty?
- Overall, canaloplasty is a safe and effective procedure and the incidence of complications is significantly less compared to traditional glaucoma surgeries such as trabeculectomy.
- Also there is no limitation of certain activities or the need for strict postoperative care making it the preferred option for many people.
- The frequency of follow ups is also much lesser.
- Use of medication eye drops following canaloplasty is also significantly reduced.
When should Canaloplasty Not be done?
- Chronic angle closure
- Narrow angles
- Neovascular glaucoma
- Angle recession
- Previous surgeries that hinder Schlemm’s canal cannulation like trabeculectomy, trabeculotomy and goniotomy.