What is Colostomy?
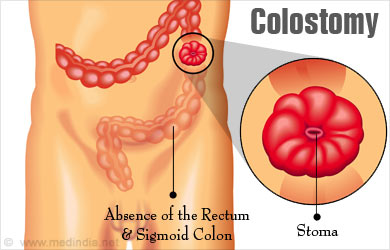
Colostomy surgery is a procedure where the colon or large intestine is diverted to an artificial opening on the lower section of the wall of the abdomen so that it can expel out fecal matter to the exterior.
The fecal matter is collected in a colostomy bag or pouch which is attached to the abdomen and this can be discarded once it fills up.
Anatomy of Large Intestine - The large intestine or colon consists of the caecum, ascending colon, transverse colon and the descending colon. The last part is S-shaped and is called the sigmoid colon. It opens into the rectum, which in turn opens into the anus.
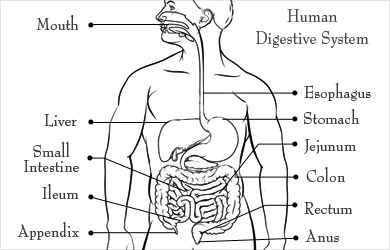
In a normal person, partly digested food from the stomach passes into the small intestines. Here, the food is digested into a liquid consistency and is partly absorbed. The contents then pass into the large intestine, where absorption of water from the digested contents takes place. The unwanted material forms feces, which passes out of the body through the rectum and anus.
Which Patients Require Colostomy?
Colostomy is required for the large intestine under the following possible circumstances:
- Where there is an obstruction to the passage of feces
- When a part of the bowel needs resection due to a disease condition
- When a part of the bowel needs to be given some rest to heal
Conditions in which a colostomy is done include the following:
- Cancer of the rectum or anus or other sections of the colon where it needs to be removed
- Fistulae of the colon leading to peritonitis - Fistulae are small holes that develop through the wall of the colon due to a disease condition like diverticulitis, Crohn’s disease or tuberculosis of the intestine. As a result of the fistulae, the contents of the colon pass into the abdominal cavity and can cause a life-threatening condition called peritonitis. A colostomy may be created as a temporary procedure to keep the affected part clear of fecal matter to give it an opportunity to heal.
- Injury to the colon such as stab or gunshot injury or due to surgery (e.g. laparoscopic surgery)
- Anomalies affecting the colon that are present from birth (e.g. Hirschsprung (HERSH-sproong) disease or anorectal malformations)
- Temporarily for obstruction of colon for example – volvulus of the sigmoid colon
Colostomy may be Permanent or Temporary
In permanent colostomy, the colostomy remains for the lifetime of the patient.
In temporary colostomy, after the condition that required the colostomy has subsided or is treated, the cut ends of the bowel are sutured back and the colostomy is surgically closed.
What are the Tests Required Before Colostomy?
In an acute surgical emergency, the decision for colostomy may need to be taken during the surgery. This type of colostomy is usually temporary and no specific tests are done.
All patients who have undergo an elective surgery (which is more planned), routine tests are required and include the following:
- Blood tests like hemoglobin levels, blood group, liver and kidney function tests
- Test for blood in the feces (called occult blood test)
- Urine tests
- ECG to study the electrical activity of the heart
- Chest x-ray
- In older group of patients, assessment of the heart maybe required
The need for colostomy in such situation is established using the following tests:
- Colonoscopy – Colonoscopy, a flexible tube with a video camera and a light source is introduced through the anus into the colon to detect any pathology in the colon. Adequate preparation of the bowel is necessary prior to the procedure so that it is clear of feces
- Lower GI X-ray or CT Series - where barium is introduced through the anus, and its passage in the lower digestive tract is studied.
How is Colostomy Surgery Performed?
Type of Anesthesia - The colostomy procedure is done under general anesthesia. You will be asleep during the procedure and not aware of what is going on.
Pre-operative Check-up - If it is an elective surgery, routine tests as indicated above are ordered a few days before the surgery. Admission is required a day or two before the surgery.
Day before Surgery - An enema is administered the previous afternoon or evening before the surgery along with gut sensitive antibiotics.
The site at which the colostomy should be done is marked in sitting as well as standing positions.
A colostomy nurse may sit with you to explain to you about how it works. It is best to ask your surgeon if you can see the nurse or make an appointment with an expert who can explain everything about how to take care of the colostomy and what it involves to live with it.
Fasting before surgery - Overnight fasting is required and occasionally intravenous fluid maybe required to keep you well hydrated. Sedation is sometimes required for good overnight sleep before the surgery.
Shift from the ward or room to the waiting area in the operating room - An hour or two before the surgery you will be shifted to the operating room waiting area on a trolley.
Once the surgical room is ready, you will be shifted to the operating room.
Shift to the Operating room - The ambience in the operating room can sometimes be very daunting and a small amount of sedation can help overcome your anxiety. From the trolley, you will be shifted on to the operating table. As you look up, you will see the operating light console and at the head end will be the anesthesia machine. There may also be monitors to check oxygen levels, ECG and other vital parameters. A constant beeping sound may be present from the monitors, which may sometimes be irritating.
Anesthesia before surgery - The anesthetist will inject drugs through an intravenous line and make you inhale some gases through a mask that will put you in deep sleep for anesthesia. Once you are in deep sleep, a tube will be inserted into your mouth and windpipe to administer the anesthesia gases to overcome pain and keep you comfortable.
Colostomy Surgery - The abdomen is opened through a planned incision depending on the type of surgery. It can be in midline or next to it either on the right or left side. Currently more and more surgeons perform laparoscopic or robotic surgery and only require to make multiple small keyholes to operate on the colon and to remove it.
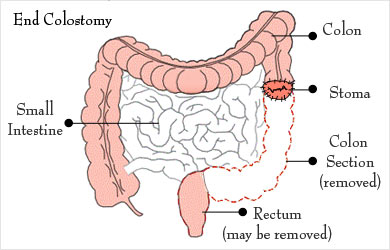
Once the main surgery is over, a circular incision is made on the skin where the colostomy site has been marked,. The muscle below the skin is dissected and the intestine is mobilized and brought out through the opening. The colon should be correctly identified at this stage. Once identified, either one of the following may be performed:
- End colostomy: End colostomy is done when the colostomy needs to be there permanently. In this type of colostomy, the colon is cut through its full thickness at the desired site. The healthy end of the colon is brought out to the anterior abdominal wall. Its edge is turned on itself to form a cuff, which is then fixed on the skin with sutures. The remaining part of the colon and rectum is closed with the help of sutures or is removed.
- Loop colostomy: Loop colostomy is done when the colostomy needs to be temporary for a few months. In this procedure, a small cut is made in the colon and the edges of the cut are sewed to the rim of the skin incision. A pencil-like plastic or glass rod may be kept just below the loop. This prevents the fecal contents spilling over back into the downstream of the colon and helps healing of a pathology like a fistula or a perforation by giving it rest. The colostomy is closed after this healing is complete so that the patient can become normal again.
- Double barrel colostomy: Like loop colostomy, double barrel colostomy is done when the colostomy needs to be temporary for a few months. In this procedure, the large intestine is cut through its full thickness and opened into the abdominal wall as two stoma. The stoma connected to the stomach excretes fecal matter, while that connected to the remaining part of the large intestine secretes mucus. Sometimes, the mucus secreting stoma is closed, in which case there is only one stoma that excretes fecal matter while the mucus passes out through the anus. The colostomy is closed after healing is complete of the primary pathology for which the colostomy was done.
Waking up from Anesthesia - Once the surgery is over you will wake up and the tube down the wind pipe will be removed. You will be asked to open your eyes before the tube is removed. You will be sedated and the voice of the anesthetist may be faint. Once the tube is out, you may have cough and sometimes nausea.
There may be a tube going into the stomach called a Ryles tube to keep it empty. There will also be an intravenous line. You will remain on oxygen. Once fully awake, you will be shifted on the trolley and taken to the recovery room.
Recovery room - In the recovery room, a nurse will monitor your vitals and observe you for an hour or two before shifting you to the room or a ward.
Post-operative recovery - You will remain in the hospital for a few days following the procedure. Normally, on the first day, you will not be allowed much to drink or eat. Once your bowel start recovering you will be given fluids and a light diet. This may take one to three days.
Change of dressing and colostomy bags will be done as required. Intravenous lines for fluids and drugs will continue for a few days till you start eating normally.
Chest physiotherapy maybe started after 24 hours to prevent chest infection.
DVT Prophylaxis – Early movement of your legs and some mobilization prevents DVT or deep vein thrombosis, where a clot is formed in the deep veins of the legs. The clot can travel up to the lungs and even be fatal. Other measures like small dose of heparin and special stockings may also be used.
Understanding How to Take Care of the Colostomy
Before you are discharged, you must be fully familiar with how to take care of the colostomy. A colostomy can be an overwhelming experience if no counseling is available both before and after the procedure. You will need to have a positive approach towards the colostomy, and continue with most routine activities just as before the surgery. A special nurse will train you into it.
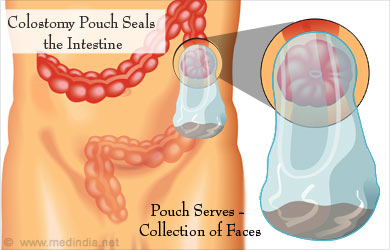
What is a Colostomy Pouch - Following a colostomy procedure, the contents of the intestine are now directed out through the abdominal wall. There is no sphincter to control the passage of the contents, which can continuously leak out. Therefore, the opening is sealed with a small bag called colostomy pouch.
The colostomy pouch consists of two parts – the barrier and the disposable plastic pouch. The barrier fits around the stoma and is attached to the pouch. In some pouches, the barrier and plastic pouch are fixed to each other and cannot be separated. It is important to note that the barrier should fit well around the stoma. This prevents the intestinal contents from coming in contact with the skin and resulting in sores.
Instructions Given Following Colostomy:
- You and/or your caregiver are taught how to care for the colostomy. The area around the stoma has to be kept clean with warm water and make sure that it is dry before a new bag can be placed.
- The pouch has to be emptied several times a day when it is around one-third full, while the barrier may be replaced every 3 to 7 days. The pouch is emptied either from below, or by removing the entire bag, depending on the type of pouch. The pouch and the barrier have to be removed gently.
- If a particular type of pouch does not suit the body habitus, you can opt for a different type.
- Some people may not require a pouch if they can predict when the bowel movement will occur like after taking certain foods or drinks. Thus, they can irrigate the stoma at regular intervals with the help of special equipment available for the purpose. The stoma may be covered with a stoma cap at other times.
- There is no specific diet that is recommended. However, over time, you will learn to avoid foods that do not suit you or cause excess gas.
- If you wish to wear tight clothes, you can wear an ostomy guard over the colostomy to prevent direct pressure over it.

What is Colostomy Reversal Surgery?
For conditions where the colostomy is not permanent, another surgical procedure is carried out to close the colostomy. During this procedure, the part of the colon attached to the skin is separated and is attached with sutures to the remaining part in the body.
What are the Benefits and Risks of the Colostomy Procedure?
Benefits of a colostomy procedure are:
- The procedure gives rest to the diseased bowel, which may not otherwise heal in the presence of feces
- Living a life with a colostomy bag may be a challenge at first, but if you are counseled well and trained to maintain the stoma and the bag, you can get back to normal activities. It usually does not create social problems since it is not obvious externally and does not give out any odor.
Possible complications of colostomy include the following:
- Complications due to the surgical procedure like bleeding or trauma to adjacent structures, and complications due to anesthesia
- Passing of excessive gas for the initial few days following the procedure
- Problems at the stoma like skin irritation, infection, narrowing of the stoma, prolapse of a part of the bowel through the stoma, appearance of a hernia around the stoma, retraction of the stoma tissue, or gangrene of the tissue
- Blockage of the colostomy caused by hard feces or formation of fibrous tissue between the intestine and other abdominal surfaces
- Diarrhea, which could result in electrolyte imbalance
- Phantom rectum, where the patients have an urge to pass stools through the anus, and may actually pass mucus when they go to the toilet
- Infection of the abdomen