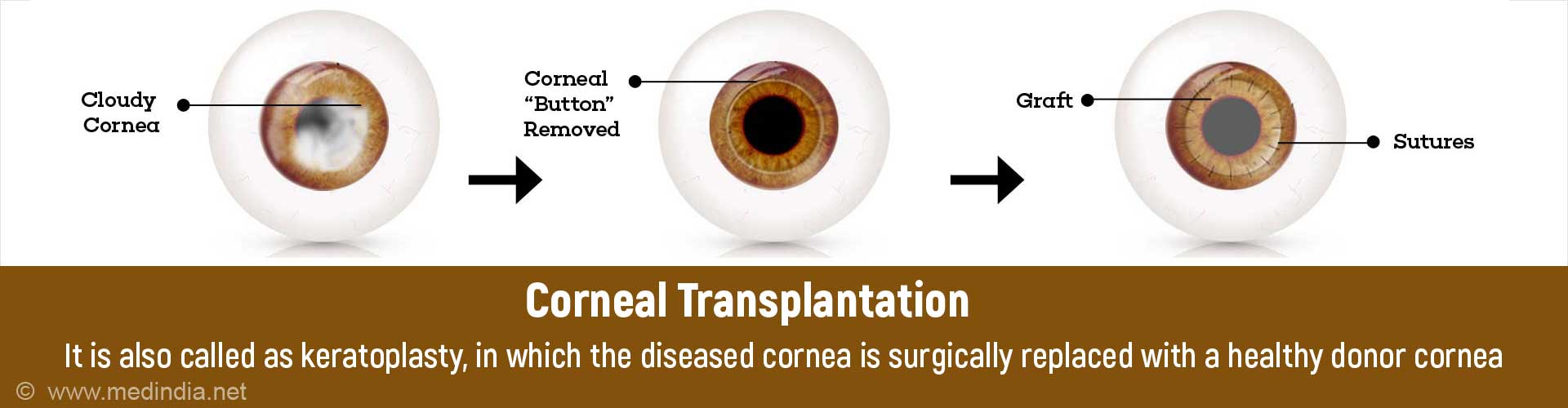
What is Corneal Transplantation?
Corneal transplantation or keratoplasty is the surgical replacement of a partial or full thickness portion of the diseased cornea in a patient with a healthy donor cornea from another individual.
Facts and Statistics of Corneal Blindness and Transplantation
Corneal blindness ranks fourth among the leading causes of blindness worldwide, after cataract, glaucoma and age-related macular degeneration. There are almost 10 million people who are blind due to bilateral corneal disease world-wide.
Corneal transplantation was the first successful solid human organ transplantation and was performed first in 1905 by Dr Edward Zirm, an Austrian ophthalmologist. Corneal transplant is the most frequently performed organ transplant. The main goals of corneal transplant are maintenance of clarity of the cornea, and restoration of vision. Unlike most other organs in the body, the cornea has neither blood vessels nor lymph vessels. This is the reason that rejection in corneal grafts is much less than that for other organ transplants, thereby making it the most successful organ transplantation.
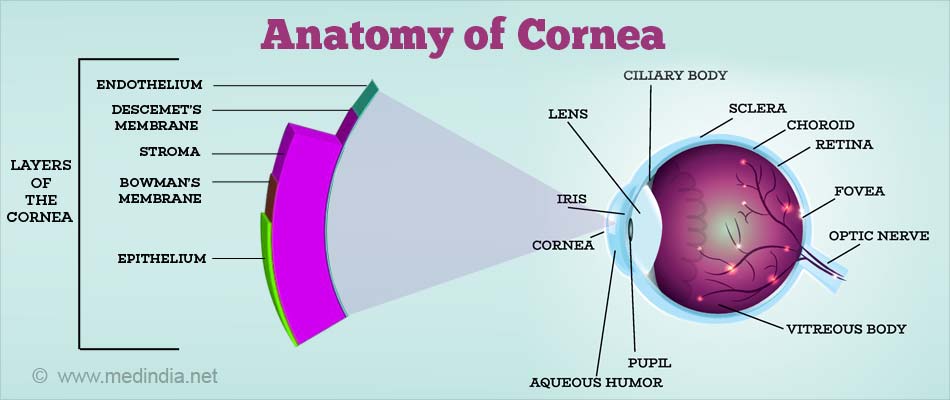
Anatomy of the Cornea
The cornea is the transparent part of the front portion of the eye that refracts (changes the direction of) light entering it. In cross section, it has six microscopic layers.
From outside to the inside these are -
| Layer | Properties |
| Epithelium | Outermost layer of cornea that provides a barrier to external stimuli |
| Bowman’s membrane | Separates the epithelium from the stroma |
| Stroma | Constitutes > 90% of cornea. Consists of collagen and water |
| Presdescemet’s or Dua’s layer | Discovered very recently by Dr Harminder Singh Dua |
| Descemet’s membrane | Intact membrane necessary to prevent hydration and swelling of the corneal stroma |
| Endothelium | The most vital layer of the cornea Contains an enzyme pump that helps keep the cornea in a dehydrated state |
What are the Types of Corneal Transplantation?
Corneal transplantation or keratoplasty is broadly of 2 types –
1. Full thickness or penetrating keratoplasty
The full thickness (all 6 layers of the cornea) are transplanted
2. Partial thickness or lamellar keratoplasty, which can be classified as:
a. Anterior lamellar keratoplasty (only the superficial layers are transplanted – performed when the Descemet’s membrane and endothelium are healthy). It can be of the following types:
- Superficial anterior lamellar keratoplasty (SALK)
- Deep anterior lamellar keratoplasty (DALK)
b. Posterior lamellar keratoplasty (The Descemet’s membrane and endothelium are transplanted – performed when the anterior cornea is healthy). It can be of the following types:
- Descemet’s stripping endothelial keratoplasty (DSEK)
- Descemet’s stripping automated endothelial keratoplasty (DSAEK) (graft thickness ~ 170 microns)
- Descemet’s membrane endothelial keratoplasty (DMEK) (graft thickness ~ 20 microns)
There are also other varieties like rotational autograft (a procedure where, in a small central corneal opacity, the scarred portion is cut, rotated 1800, and then sutured back in the same place) and keratoprosthesis, which is a corneal transplantation using an artificial cornea.
What is the Source for Donor Cornea?
Donor corneas are almost always obtained from a person after death (cadaveric donor). Either just the cornea (along with a rim of attached sclera), or the entire eyeball is removed from the dead person within 6-8 hours after death, and stored in an eye bank. Nowadays with good preservative techniques, donor corneas can be preserved for up to 2 weeks or more, providing adequate time to process the tissue and select a candidate for transplantation.
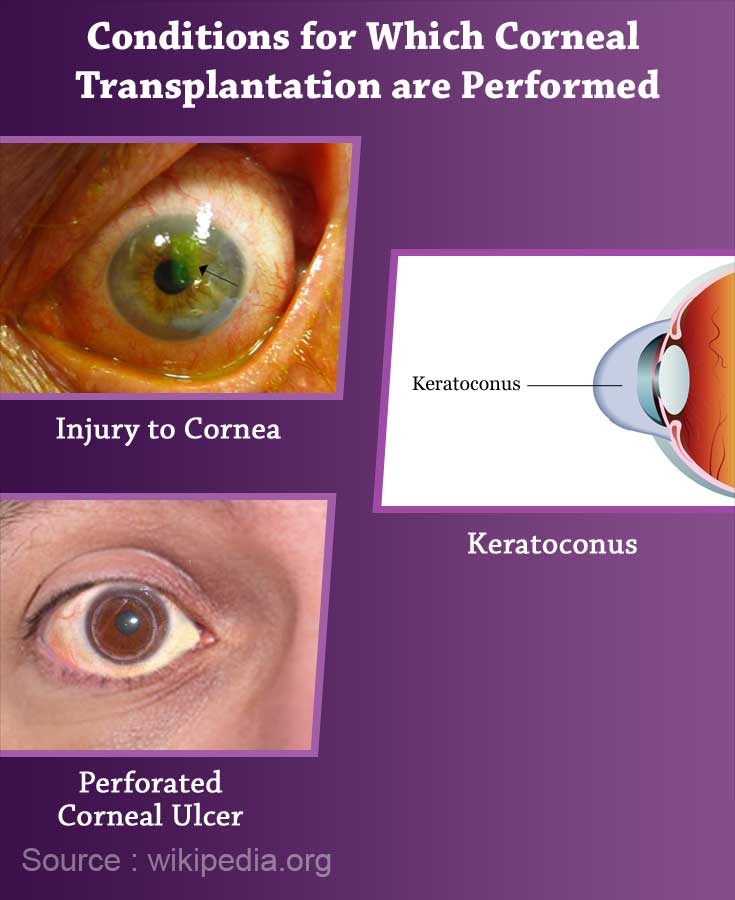
What are the Conditions for which Corneal Transplantation is Performed?
Any person with a permanent opacification of the cornea is a candidate for corneal transplant, provided the rest of the eye is healthy. Some of the indications are -
| Conditions for which corneal transplantation is performed | |
| Keratoconus | A condition associated with progressive thinning of the cornea and outward bulging resulting in diminished vision and scarring |
| Fuchs’ endothelial dystrophy | Bilateral slowly progressive swelling of the cornea due to dysfunction in the endothelium of the cornea in elderly patients |
| Pseudophakic bullous keratopathy | Chronic corneal swelling due to surgical damage of the endothelium during cataract surgery with IOL(intraocular lens) implantation |
| Previous graft failure | Following a previous corneal transplantation |
| Injury to cornea | Resulting in corneal scarring |
| Healed corneal ulcers | Resulting in corneal scarring |
| Perforated corneal ulcer | A deep corneal ulcer which gives way to expose the interior of the eye |
| Acid or alkali injuries | Resulting in corneal scarring |
| Congenital corneal disorders | Such as corneal dystrophies |
| Non-healing corneal infection | Transplantation done to remove the infective load and promote healing |
Penetrating keratoplasty is the most common type of keratoplasty performed. However, nowadays there is a greater tendency towards lamellar procedures, which avoid some of the disadvantages of penetrating keratoplasty. The decision to perform either a penetrating or a lamellar procedure depends on the type of corneal opacification and the experience and comfort of the surgeon. Anterior lamellar keratoplasty is nowadays preferred over penetrating keratoplasty in cases such as keratoconus, and superficial corneal scars. DSEK and DSAEK are preferred over penetrating keratoplasty in cases such as Fuchs’ endothelial dystrophy and pseudophakic bullous keratopathy.
How is an Eye evaluated prior to Corneal Transplantation?
A thorough ophthalmic evaluation is done to identify any infection, inflammation, dryness of the eyes or reduced corneal sensation, any condition that may alter the success of the graft such as presence of abnormal blood vessels in the cornea or raised intraocular pressure, or any condition that may prevent restoration of vision following the graft such as retinal or optic nerve disorders. The above can be identified with slit lamp examination, measurement of intraocular pressure, and retinal examination.
How to Prepare for Corneal Transplantation Surgery?
- Avoid eye makeup from 3 days prior to surgery
- You may be prescribed antibiotic eye drops from 1-3 days prior to the surgery by your doctor
- This is a day care procedure and does not require admission. You may reach the hospital on the day of your procedure
How is Penetrating Keratoplasty Performed?
- An oral anti-anxiety medication may be recommended to be taken on the morning of the procedure to calm you down.
- In the operation theatre, you will be made to lie down on the operating table. The skin around your eyes will be cleaned with povidone – iodine or alcohol for antiseptic purposes.
- Penetrating keratoplasty is usually performed under local anesthesia, except in children and uncooperative adults where general anesthesia is preferred. The anesthetic solution is injected into the tissue around the eyeball.
- A sterile drape will be placed over your face to expose only the eye that is being operated. An instrument will then be placed in your eye to keep the eyelids separated so that your eye remains open. You might feel some pressure but there will be no pain.
- The donor cornea is placed on a Teflon block and the required size of the corneal donor button is cut with the help of a trephine (a circular blade to cut tissue). A scleral fixation ring may be sutured to your sclera to prevent collapse of the eye. Your cornea will also cut with a trephine (about 0.5 mm smaller than the donor button) to remove the abnormal area. The donor cornea is then placed on your eye and sutured with 10-0 continuous or interrupted nylon sutures. An injection of steroid and antibiotic under the conjunctiva is given, the eye is patched and a protective shield is placed over it.
- Nowadays some eye surgeons use the femtosecond laser (which uses an infrared scanning pulse to cut tissue) instead of the microkeratome to make the cut in donor and recipient tissue in both penetrating and lamellar keratoplasty for more precision.
What is the Post-operative Course Following Penetrating Keratoplasty?
- After penetrating keratoplasty you may be allowed to go home after about an hour or two, if there are no other systemic or local complications
- You will need to visit your eye doctor the next day when he will open your eye patch.
- You will be instructed to instil antibiotic and dilating eye drops for up to month. Steroid eye drops are usually continued for one year following surgery.
- You will need to visit your eye doctor regularly for check-ups for a minimum period of one year. Sutures are generally not removed before one year.
Here are some do’s and don’ts after the procedure:
- DO avoid rubbing and squeezing of the eyes. Use a fresh clean tissue (can be moistened with clean warm water) to gently clean the outside of your eyelids if there is any watering or crusting.

- You may shower the next day, but wear the protective eye shield. If you are washing your hair, tilt your head back so that water does not get into your eyes.
- DO wear sunglasses when you go outdoors
- DO wear the plastic protective eye shield at night till your doctor tells you to stop. This may be anywhere from one to six months. In the daytime, wear either your glasses or the protective shield.
- DO NOT lift any weights over 5 kilograms, or do any strenuous work
- DO NOT engage in sports, swimming, jogging, exercise (other than walking) or coitus till one month after surgery. Confirm with your doctor regarding when you can continue with the above activities
- DO NOT engage in any activity that puts your head lower than the rest of the body, including yoga.
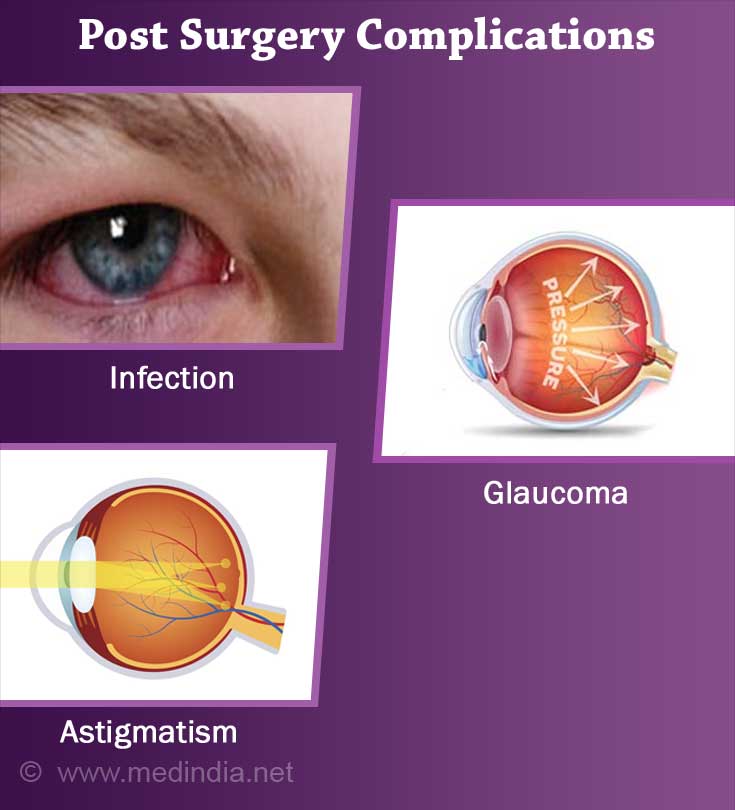
Risk and Complications of Penetrating Keratoplasty
Some of the complications that can arise after the procedure are -
Early: Wound leak, raised intraocular pressure, infection, primary graft failure, graft rejection.
Late: Astigmatism, glaucoma, cystoid macular edema (swelling of the macular region of the retina), recurrence of the original disease in the graft, graft failure, graft rejection.
What is Some of the Latest Research in this Field?
Recent years has seen a greater requirement for donor corneas due to better results following adaptation of lamellar procedures. However, the the limited availability of donor material is the major hurdle to reducing the burden of corneal blindness world-wide. The main focus of current research is to either produce methods to find an alternative to corneal transplantation, or to reduce the risk of graft rejection.
Even though rejection in case of corneal transplantation is much less compared to other organ transplants, it is still the major reason for graft failure (loss of graft clarity). Efforts are on to see whether HLA matching (HLA or human leucocyte antigens are situated on the surface of most cells and are responsible for organ transplant rejections) which is performed routinely for other organ transplants, will help reduce the risk of corneal transplant rejection as well. Successful primary grafts reduce the burden of repeat surgeries, which diminish the demand for donor procurement.
A new technique in corneal transplantation in keratoconus is isolated Bowman's layer transplantation – the Bowman layer is dissected out of the donor eye and transplanted into the stroma of a recipient eye diagnosed with keratoconus. This strengthens the cornea and stabilises the outward bulging in keratoconus.
A biosynthetic implants such as recombinant human collagen implants (which are free of cells) have been tried to enable regeneration of a normal cornea in place of the abnormal one.
Efforts are being made to culture corneal endothelial cells (by harvesting from a single donor eye, and then transplanting to multiple recipients), in an effort to replace the cornea for conditions such as Fuchs’ endothelial dystrophy and pseudophakic bullous keratopathy.
Preliminary attempts being made to regress pathologic corneal lymph vessels are showing some promise in trying to improve graft survival rates.
Attempts are being made to administer interleukin -2 to improve graft survival rates.
Most of these are in the very preliminary stages and it may be some time before they actually come out in practice.