What is Craniotomy?
Craniotomy is a surgical procedure where an opening is made in the skull to enable to access and expose the brain.
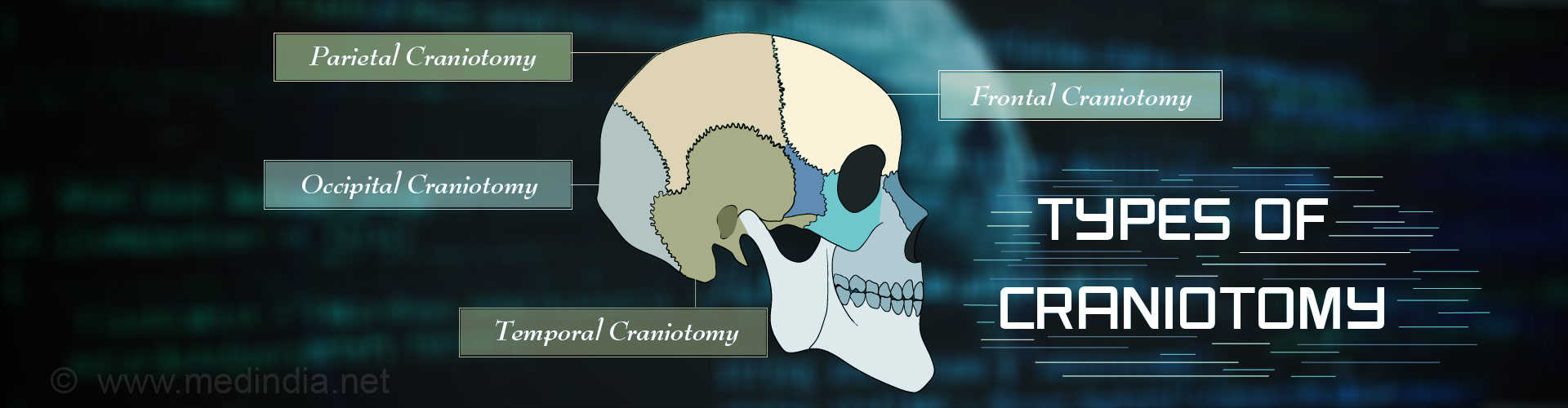
What are the Types of Craniotomy?
Craniotomy can be classified into several types depending on the location. The skull consists of the frontal bone located at the forehead, the temporal bones at the temples, the parietal bones on both sides, and the occipital bone at the back of the head.
- Frontal craniotomy is performed through the frontal bone
- Temporal craniotomy is performed through the temporal bone
- Parietal craniotomy is performed through the parietal bone
- Occipital craniotomy is performed through the occipital bone
- Pterional craniotomy is performed at the junction of the frontal, temporal, greater wing of sphenoid and parietal bones. The sphenoid is a bone at the base of the skull.
Craniotomy can involve more than one skull bones, for example, frontotemporal craniotomy, frontotemporoparietal craniotomy
Other types of craniotomies include:
- Keyhole Craniotomy, where the surgery is carried out through a small hole. It is done for lesions that are not immediately just below the brain.
- Stereotactic Craniotomy, where a 3-dimensional coordinates system is used to precisely locate the problem area that needs surgery.
- Awake Craniotomy, where the patient can be woken up during the surgery. It is commonly done for epilepsy surgeries, or when the lesion is close to a critical area of the brain. The patient’s responses are checked during the surgery to make sure that the vital parts of the brain are not being affected.
What are the Indications for Craniotomy?
A craniotomy gives access to the inside of the skull. Indications for craniotomy include:
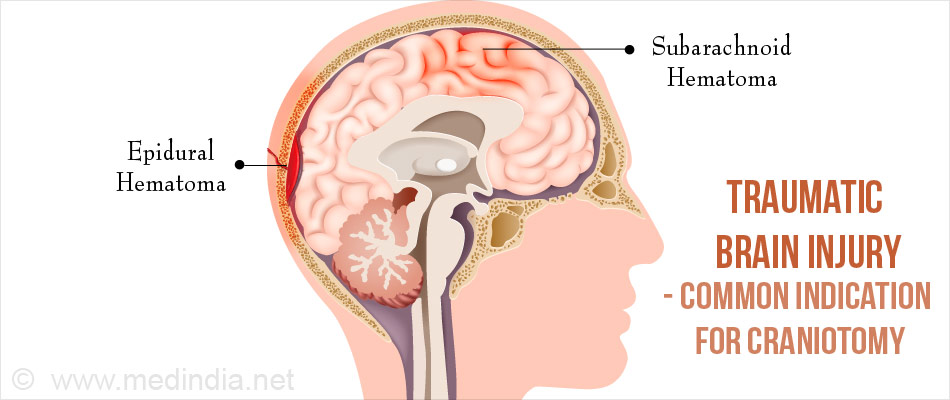
- Surgical removal of a tumor or blood clot, or draining of an abscess within the skull. Brain injury following trauma is one of the commonest indications for craniotomy.
- Clipping of an aneurysm: An aneurysm is a dilated artery with weakened walls, which has the potential to burst and result in life-threatening consequences. Clipping of the aneurysm reduces blood flow through it and therefore decreases its size and its potential to burst.
- Removal of an arteriovenous malformation: An arteriovenous malformation is an abnormal communication between an artery and a vein. It can bleed and result in grave consequences.
- Surgery for epilepsy: Certain cases of epilepsy do not respond to medication and require surgery
- Ventricular shunting. Ventricular shunting is a procedure performed to reduce pressure in the skull due to excess fluid accumulation.
- Other procedures like inserting deep brain stimulators for the treatment of conditions like brain tumours, Parkinson’s disease, essential tremor and dystonia.
What are the Tests Done Prior to Craniotomy?
Tests done prior to craniotomy include the tests required to diagnose the pathology and locate it precisely within the skull, as well as routine tests done before any surgery. These include:
- Imaging Tests like CT scan (most common), MRI and functional MRI are performed to identify and locate the lesion. An angiography may also be done in selected cases to identify the blood supply to the lesion.
- Routine Tests which are done before any surgery include:
- Blood tests like hemoglobin levels, blood group, and liver and kidney function tests; tests to ensure that the blood coagulation system is intact
- Urine tests
- ECG to study the electrical activity of the heart
- Chest x-ray
In older patients, a detailed assessment of the heart may be required to make sure that they are fit for surgery.
Medications that are administered prior to the surgery depending on the type of lesion include:
- Anti-seizure medications to prevent the development of seizures
- Corticosteroids to reduce swelling
- An antibiotic to prevent infection due to the surgery
Blood thinners should be stopped a few days before the surgery to prevent excess bleeding
How is Craniotomy Performed?
Type of Anesthesia - A combination of general anesthesia and local anesthesia is often used for the craniotomy procedure. If you are under general anesthesia, you will be asleep during the procedure and will not be aware of what is going on. If you are undergoing a sleep-awake-sleep craniotomy, you may be given general anesthesia but will be woken up during the surgery. The local anesthetic is mixed with epinephrine to reduce bleeding from the incision.
Pre-operative Check-up - Routine tests as indicated above are ordered a few days before the surgery. Admission is usually required a day before the surgery.
Fasting Before Surgery - Overnight fasting is required and occasionally intravenous fluid maybe required to keep you well hydrated. Sedation is sometimes required for good overnight sleep before the surgery.
Shift From the Ward or Room to the Waiting Area in the Operating Room - An hour or two before the surgery, you will be shifted to the operating room waiting area on a trolley.
Once the surgical room is ready, you will be shifted to the operating room.
Shift to the Operating Room - The ambience in the operating room can sometimes be very daunting and a small amount of sedation can help overcome your anxiety. From the trolley, you will be shifted on to the operating table. As you look up, you will see the operating light console and at the head end will be the anesthesia machine. There will also be monitors to check oxygen levels, ECG and other vital parameters. A constant beeping sound may be present from the monitors, which may sometimes be irritating.
Anesthesia Before Surgery - If you have to undergo general anesthesia, the anesthetist will inject drugs through an intravenous line and make you inhale some gases through a mask that will put you in deep sleep. Once you are in deep sleep, a tube will be inserted into your mouth and windpipe to administer the anesthetic gases to overcome pain and keep you comfortable. If local anesthesia is used, an anesthetic drug will be injected in the region where the incision will be taken.
Incision for Craniotomy - The location of the incision for the craniotomy procedure depends on which part of the brain has to be operated. The inner part of the skull is divided by tissue called tentorium cerebelli into an upper supratentorial part and a lower and posterior infratentorial part.
- For a surgery in the supratentorial part, the incision is made through the frontal, temporal, parietal or occipital bones, or through more than one bone
- For a surgery in the infratentorial part, the incision is made through the back of the skull just above the neck
The desired location of the incision is marked on the skin. The hair in the area may be shaved off and a scalp flap is made. The incision should preferably be behind the hairline for cosmetic effect. A local anesthetic with epinephrine is usually injected just before the incision is made to reduce bleeding. The muscles below the scalp are separated to reach the bone of the skull.
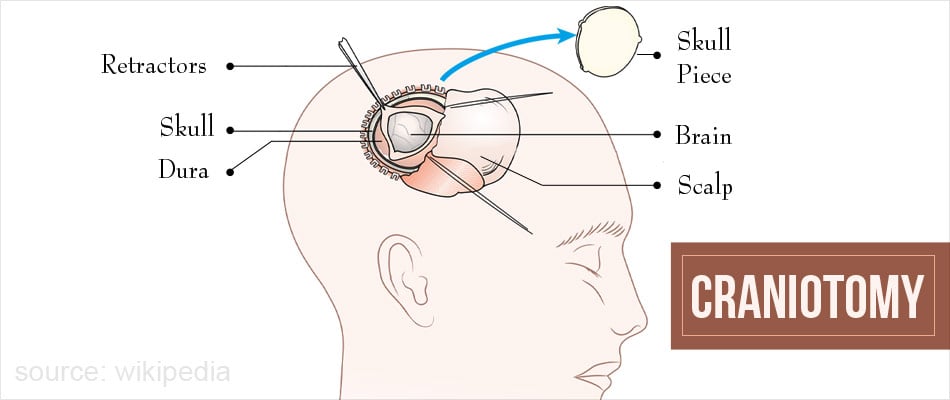
Craniotomy - Four to five holes are bored into the skull. The holes are connected with a saw and a bone flap is cut out after carefully separating it from the dura below. The dura is then cut and retracted, exposing the brain.
Once the surgery on the brain is done, the bone is usually replaced and kept in position with soft wire, or plates and screws. The overlying tissues are replaced and the scalp is then sutured into position.
Waking up from General Anesthesia - If you have received general anesthesia during surgery, once the surgery is over you will wake up and the tube down the wind pipe will be removed. You will be asked to open your eyes before the tube is removed. You will be sedated and the voice of the anesthetist may be faint. Once the tube is out, you may have cough and sometimes nausea. Your doctor will do some tests to make sure that your nerves are not damaged during the surgery.
There may be a tube going into the stomach called a nasogastric or Ryle’s tube to keep it empty. There will also be an intravenous line. You will remain on oxygen (usually through a face mask). Once fully awake, you will be shifted to the recovery room.
Recovery Room - In the recovery room, a nurse will monitor your vitals and observe you for an hour or more before shifting you to an intensive care unit, where you will be monitored carefully.
Post-operative Recovery - You will remain in the hospital for a few days following the procedure. Light foods may be allowed following the surgery.
Chest physiotherapy maybe started after 24 hours to prevent chest infection.
DVT Prophylaxis - Early movement of your legs and some mobilization prevents DVT or deep vein thrombosis, where a clot is formed in the deep veins of the legs. The clot can travel up to the lungs and even be fatal. Other measures like small dose of heparin and special stockings may also be used.
After you are discharged from the hospital, you will have to revisit your doctor after 5 to 10 days for removal of the sutures.
What are Risks Associated with Craniotomy?
Craniotomy is a highly complex surgery. Complications of craniotomy can be life threatening and include:
- Headache
- Leakage of cerebrospinal fluid (CSF), the fluid surrounding the brain, through the cut area if it is not closed properly
- Bleeding resulting in the formation of a hematoma. The hematoma may be required to be removed with repeat surgery
- Spasm of blood vessel resulting in reduced blood supply to a particular part of the brain, thereby resulting in damage to that part
- Infection
- Air embolism, where air enters a blood vessel and interferes with blood supply to a particular part. Insertion of a CVP line (central venous pressure line) just before the surgery helps to remove any possible air embolisms
- Diabetes incipidus due to damage to the pituitary gland, an important endocrine gland in the brain
- Seizures
- Damage to cranial nerves, the nerves supplying the head and neck region
- Respiratory problems