What is Hepatectomy?
Hepatectomy is a surgical procedure to remove a diseased liver.
The liver is a large organ in the upper abdomen, more on the right side. It has several important functions like digestion through secretion of bile, removal of toxins and production of clotting factors.
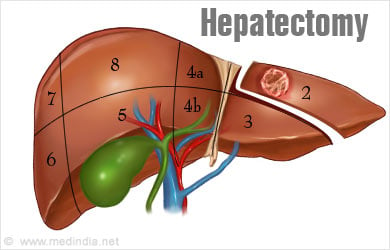
Anatomically the liver consists of two parts, the larger right lobe and the smaller left lobe. It can also be divided into segments. Each segment has its own artery, vein and bile duct. Thus, a segment can be safely removed without affecting the functioning of other parts of the liver.
Hepatectomy surgery may be partial or complete.
- Total or Complete Hepatectomy involves removal of the entire liver. This procedure is followed by liver transplantation.
- Partial Hepatectomy removes only a part of the liver. The liver is an organ that is capable of regeneration. Thus, if a part of the liver is removed, the cells of the remaining part multiply to replace the cut portion. However, this is possible only if the remaining part of the liver is completely normal.
What are the Indications for Hepatectomy?
Hepatectomy is done for several conditions that affect the liver. These include:
- Liver cancer called hepatocellular carcinoma that arises from the liver cells. Cancers that are limited to a part of the liver may be completely cured by partial hepatectomy.
- Cancers that have spread to the liver from the colon or carcinoid tumor. In these cases, part of the liver can be resected if the cancer is restricted to one particular portion of the liver.
- Benign liver tumors especially those, which cause pain or are at a risk for rupture.
- Hepatolithiasis or bile stones in the liver
- Parasitic cysts in the liver: Cysts are fluid-filled swellings which may be caused by a tapeworm infection; this condition is referred to as hydatid cyst disease.
- Large liver hemangiomas that cause symptoms, hemangiomas are abnormal growths consisting of blood vessels.
- Acute or chronic liver failure, where total hepatectomy is followed by liver transplantation.
- Congenital diseases where the liver is affected.
In addition, partial hepatectomy is also done on a live healthy donor to obtain a part of the liver for liver transplantation.
What Tests are Commonly Done Before Hepatectomy?
A. Blood Tests
Besides general blood tests such as measuring the hemoglobin, white blood cells, red blood cells and platelets, checking the electrolytes and kidney function tests (blood urea nitrogen (BUN) and creatinine), liver-specific tests are advised. These include -
Tests to measure for viral hepatitis: Your doctor might recommend blood tests to check for hepatitis B and C.
- Alpha-Fetoprotein Blood (AFP): If AFP is high in someone who has a solid tumor in the liver, it means that it is a malignant tumor. AFP is a protein substance that normally is found in high amount in a fetus (hence the name) but it goes down after birth. The protein is a marker for liver cancers and some other tumors. It also acts as a marker for following up patients after they are treated and if it goes up, it means the disease has come back.
- Liver Function Tests (LFTs): Specific enzymes of the liver like SGOT/SGPT and other chemical substances like bilirubin and proteins such as albumin, globulin and alkaline phosphatase can measure how well your liver is functioning and are advised before surgery.
- Blood Clotting Tests: The liver helps stop bleeding by producing certain proteins that help with blood clotting. A compromised or damaged liver might not make enough of these clotting factors, which could increase the risk of bleeding. These tests are called prothrombin time (PT) and partial prothrombin time (PTT).
B. Radiology Tests
Usually first ultrasound is done and depending on the findings, other imaging tests are advised. These are usually a CT scan or MRI scan. These tests are done for both, knowing the extent of the disease and doing a biopsy to confirm the diagnosis. The advanced tests are also useful in planning a partial hepatectomy surgery.
MRI Scans - Although MRI scans can be little more uncomfortable than CT scans, they are very useful when looking at the liver tumors and can sometimes differentiate a benign tumor from a malignant one.
After a plain MRI, a contrast material called gadolinium is injected into the vein to help see details of blood vessels and other structures more clearly. The dynamic contrast-enhanced MRI also gives details of other parts of the body.
For MRI, the patient is placed inside a narrow tube which can make the person claustrophobic if the individual has a fear of enclosed spaces. Few centers do offer more open MRI machines, but the drawback is that the pictures may not be as clear. The MRI machine makes loud clicking noises and it is advisable to ask for earplugs to help block these noises out.
Positron Emission Tomography (PET) - This nuclear medicine imaging technique provides a three-dimensional image of the liver or pancreas and its surrounding structures. Generally PET is used in conjunction with CT to produce more accurate and detailed pictures of the liver.
C. Angiography
An angiogram is an x-ray test to look at the architecture of the blood vessels of an organ. A contrast medium, (also called dye) is injected into an artery to outline blood vessels while multiple x-ray images are taken. A CT or MR angiography can also be taken instead of injecting into the liver artery directly. Angiograms give an idea of the extent of the tumor and help in planning the surgery.
Direct injection into the liver artery is used to guide some types of non-surgical treatment, such as embolization of the cancer where a material is injected to block the blood supply of the tumor.
For any of these procedures usually an intravenous line is inserted before starting the procedure.
D. Radionuclide Scan
- Bone scan - A bone scan is advised where the doctor suspects spread of the cancers to the bones. Generally it is not a routine test.
- Radiolabeled meta-iodobenzyl-guanidine (MIBG) scans help in visualizing cancers such as carcinoid tumors and neuroblastoma of the liver.
What is the Surgical Procedure for Hepatectomy?
Hepatectomy is done either as an open surgery or through laparoscopy. In most instances an open surgery is undertaken.
Anesthesia
Hepatectomy is done under general anesthesia and the patient will be unconscious throughout the surgery, and feel no pain. To prepare for the surgery, no food or drink is allowed for 6 to 8 hours before the anesthetic. However to keep hydrated, patient may have a ‘drip’, where a small tube is placed into one of your veins and attached to a bag of fluid.
Procedure
In an open surgery, the incision is made under the ribs and sometimes in the middle of the abdomen. Ligaments that keep the liver in place are divided and the liver is mobilized. The veins, arteries and the bile ducts to the part being resected are identified and isolated.
Several techniques are used to cut off the affected part of the liver. An ultrasonic surgical aspirator is commonly used. Laser may also be combined with the procedure. A cautery or diathermy, which uses heat produced from electricity, may also be used.
A wedge resection may be used for superficial lesions, where only the affected part of the liver with a small amount of normal tissue around it is removed. In other cases, one or more affected segments or a lobe of the liver may be removed.
Laparoscopic hepatectomy uses a laparoscope for the surgery. A laparoscope is an instrument with a camera at the end which is introduced into the abdomen through a small incision. Additional small incisions are made to introduce instruments to carry out the surgery. Sometimes, the surgeon may plan a laparoscopic surgery but may have to convert it to an open surgery during the procedure if any difficulties or complications arise.
Partial Hepatectomy – In a partial hepatectomy for liver transplantation, 60% of the adult liver is removed andextreme care must be taken to minimize blood loss or injury to critical structures such as bile ducts and blood vessels, and the exact anatomy of these structures should be studied as best as possible prior to even starting the operation. However when the donation is to a child only 25% of the liver is removed and it is usually the left lobe of the liver.
After the Procedure
First 24 to 48 hours - Once the surgical operation is over patient will be kept in a special intensive care unit where well trained specialist team of intensive care doctors and nurses take care of the patients to ensure that they are kept stable hemodynamically (blood pressure, oxygenation, fluids and urine output) are balanced and maintained.
Normally for the first 24 to 48 hours, the patient will be kept on ventilator (a special machine that keeps the lung expanded and the body well oxygenated) and will be deeply sedated until it is time to remove the ventilator. Once the ventilator is removed, the person will be fully conscious, and can start eating and moving around slowly.
Function of the resected liver is monitored closely by blood tests and ultrasound examinations. The liver function tests should demonstrate a trend towards normal during this time. On rare occasions, there might be a surgical complication such as a bleeding vessel or a leak of bile and may require an exploration surgery.

During this period, a limited number of relatives maybe allowed to see the patient.
Postoperative Days (PODs) 3-10 days –The patient will be extubated (ventilator removed) once the condition is stable.
In the ICU, the patient is surrounded by monitors and tubes that go into the vein to provide with fluids and drugs. There will also be a catheter draining the urinary system. A naso-gastric tube to drain the secretions into the stomach is also expected in some cases.
A drain may be inserted into the abdomen during the surgery and will be removed after a few days.
Patient may experience discomfort in the abdomen or with one of the tubes and doctors can prescribe pain-killers to alleviate the pain. The patient usually remains on the fluid ‘drip’ until the person drinks enough fluids themselves.
As a progress in seen in a patient all the tubes will be removed one at a time. Of all the tubes, the naso-gastric tube maybe the most uncomfortable. This is usually removed once ‘wind’ or flatus is passed.
After the urinary catheter has been removed, a mild burning discomfort may be experienced during urine passage. This symptom is normal, and will not last for long.
Usually after a few days (varies usually from 2 to 7 days), patient can return to the general room for further recovery. Here, nurses and doctors ensure adequate pain control and a normal recovery path, regularly monitoring liver function tests.
The patient may be asked to sit up and will become ambulatory in the room. Sutures are removed after 2weeks usually after discharge 8 to 14 days.
The bladder catheter is removed on postoperative Day #3 and usually the surgical drains are all removed prior to discharge home. The sutures closing the skin incision are not removed until 2-3 weeks after the operation and this is done in the outpatient clinic. When the patient’s liver function tests (and all other labs) normalized and they are ambulating and tolerating a regular diet, the Transplant Pharmacist and/or Transplant Social Worker have teaching sessions with the patient and family to ensure that everyone understands the many different drugs that must be taken, their purpose, their doses and their potential side effects. Also, general discharge advice about avoiding infection and when to return to the outpatient clinic are imparted.
What are the Advantages of Laparoscopic over Open Surgery for Liver Resection?
Laparoscopic surgery is usually preferred over open surgery whenever possible. The incisions used are smaller, and therefore surgical scars are smaller. Pain is less and recovery is usually faster.
What are the Complications of Hepatectomy?
Hepatectomy is often a safe procedure in experienced hands. Complications of hepatectomy could include the following:
- Excessive bleeding
- Trauma to surrounding organs
- Accumulation of fluid in the abdomen, called ascites
- Accumulation of fluid in the pleural space outside the lungs, called pleural effusion
- Infection
- Leakage of bile into the abdomen
- Liver failure
- Kidney failure
- Ileus, where the intestines are paralyzed. Normally, they recover in 2 to 3 days after surgery but when they take longer, the abdomen swells up and there is discomfort in breathing and you will feel very bloated up.
- Pulmonary embolism, a condition where a blood clot travels to the lungs. This complication is seen in major surgeries, where the patient cannot move for prolonged durations
- Complications due to anesthesia like chest infection, cough and sometimes pneumonia.
- Rarely death
- Postoperative pain