What is LASIK?
LASIK is an acronym for laser assisted in-situ keratomileusis. It is a type of laser procedure performed on the eye to correct refractive errors and presbyopia by reshaping the cornea.
It was first performed by Pallikaris in 1990.
The refractive power of the eye depends primarily on 3 factors:
- Curvature of the cornea
- Curvature and refractive index of lens
- Antero – posterior diameter (axial length) of the eye
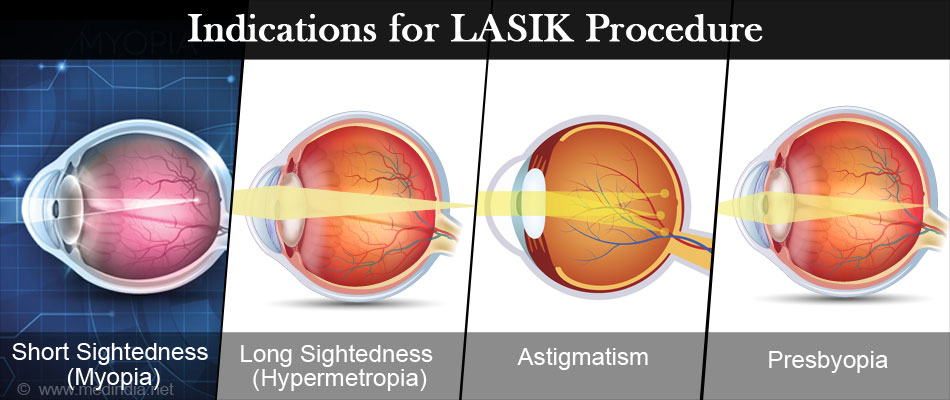
In LASIK, the corneal curvature is altered by reshaping the cornea using an excimer laser, regardless of the cause of the refractive error (maybe due to short sightedness, long sightedness or astigmatism or presbyopia - age related difficulty in seeing near objects) to correct defective vision.
Why is LASIK Procedure Performed?
A refractive error results when the light rays from an object does not fall on the retina after the refraction that takes place at the cornea and lens. The light rays either fall in front of the retina (short-sight or myopia), behind the retina (long sight or hypermetropia) or differentially in different meridians of the eye (astigmatism). Alternately, in presbypopia (age related physiological weakness of accommodation), images from near objects alone fall behind the retina.
For example, in myopia the rays fall in front of the retina due to excess convergence. Hence, the cornea can be flattened to result in a mild divergence of rays (due to reduced converging ability) so that they can fall exactly on the retina. This is done by removal of corneal tissue (ablation) in the center of the cornea. Similary, in hypermetropia, the central portion of the cornea is made more convex to increase convergence by ablating tissue in the form of a ring around the center of the cornea.
In astigmatism, the cornea is shaped differentially according to the refraction.
In presbyopia, either the cornea is converted in to a multifocal surface, or one eye is made more convex so that that eye can be used for near vision while the other eye is used for distant vision (monovision). When LASIK is used to correct for presbyopia it is called presbyopic LASIK.
Wavefront-Optimized and Wavefront-Guided ablations do a little more intricate reshaping of the curvature of the cornea to give better quality of vision after the procedure.
What Type of Laser is Used?
A 193 nm ultraviolet argon fluoride excimer laser (where excimer stands for excited dimer) is used for tissue ablation.
A Femtosecond laser (which uses an infrared scanning pulse to cut tissue) is also sometimes used instead of the microkeratome to create the corneal flap – this is also called bladeless LASIK.
How is LASIK Performed?
The cornea is the transparent part of the front portion of the eye.
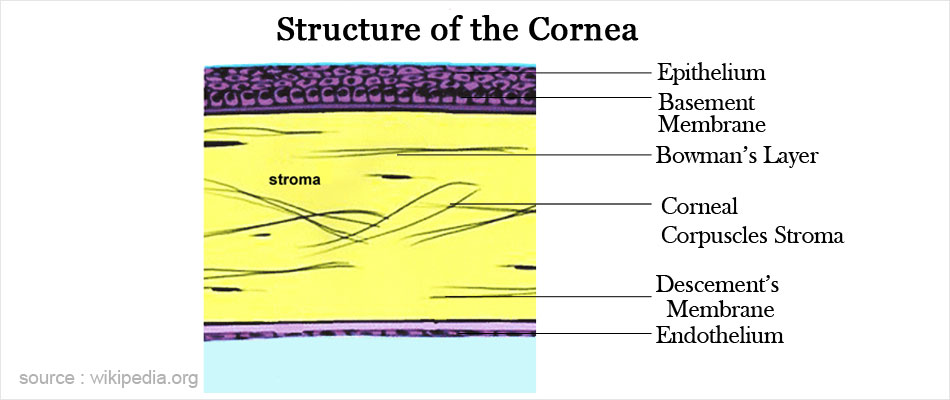
In cross section, it has six microscopic layers – epithelium, Bowman’s membrane, stroma, Dua’s layer, descemet’s membrane and endothelium.
A hinged corneal flap (usually about 130-180 microns in thickness) is created by splitting the cornea through the middle of the stroma in to a superficial and deep part The flap is then retracted and excimer laser applied to the remaining stroma (stromal bed). The tissue removal is achieved by destruction of intermolecular bonds. The location of ablation is determined by the type of refractive condition – central ablation for myopia, and midperipheral ablation for hypermetropia. The flap is then replaced where it will get adhered to the deeper structures during healing.
Who can Undergo LASIK?
- Patients with refractive powers ranging from +6.00 to -12.00 dioptres, and up to 4 dioptres of astigmatism, and who do not wish to wear glasses or contact lenses.
- Patients with presbyopia who do not wish to wear glasses for reading.
- Patients in the above refractive range who take up vocations where spectacle wear is not allowed.
What Should the Patient Undergoing LASIK Expect?
- LASIK can correct only up to about 12-14 dioptres of myopia. Higher powers would require some other procedure like placement of an intraocular lens in the eye.
- Younger patients undergoing refractive procedures should be aware that if correction of the refractive error is undertaken, the person would still need to wear glasses by about the age of 40 years due to the onset of presbyopia. Presbyopia affects all near vision tasks such as reading, mobile phone use, computer use, looking at one’s face in the mirror, tailoring, looking at labels at shops and looking at a watch.
- Patients in and around the presbyopic age-group need to be aware of this, and may consider going in for unilateral correction or undercorrection if myopic, if they wish to read without glasses after the procedure. A trial of contact lenses prior to the procedure would help the patient understand the situation better, so that they can make an informed decision.
- LASIK cannot prevent future ocular problems like cataract and glaucoma.
- Also, since LASIK corrects the refractive error at the level of the cornea, and does not affect the retina, any tendency to retinal detachment in a high myope is not addressed, and the person would still require to undergo regular ophthalmic screening even if the myopia is corrected.
LASIK vs. Photorefractive Keratectomy (PRK)
In Photorefractive Keratectomy (PRK) too similar Laser is used but it is used for surface ablation (tissue removal) of cornea and not raising flaps. The difference between the two procedure is shown in the table:
| Lasik | PRK | |
| Laser Used | 1. Excimer 2.Femtosecond in bladeless LASIK | Excimer |
| Depth of cornea at which treatment is performed | Deep (mid-stroma) | Superficial |
| Corneal flap related complications | Yes | No |
| Pain after the procedure | Minimal | Can be moderate to severe |
| Procedure can be done in thin corneas | No | Yes |
| Risk of ectasia (outward bulging of cornea) after procedure | More | Less |
| Post-operative vision recovery | Less than 1 day | 3-7 days |
| Corneal haze | Less common | Quite common |
In Photorefractive Keratectomy (PRK) also, a similar laser is used. However PRK is a surface ablation procedure and no corneal flap is raised. The difference between the two procedures is shown in the table:
When Should LASIK Not be Done?
- If patient is less than 18 years of age
- If the power is not stable for at least one year (> 0.5 dioptre change in power)
- If the cornea is < 500 microns in thickness.
- Severe dry eyes
- Presence of corneal disease
- Presence of other ocular conditions like uncontrolled glaucoma, cataract etc.
- If there is evidence of corneal ectasia (outward bulging) as evidenced on corneal topography, then LASIK should not be done as there is a risk for further ectasia after the procedure. Even a subclinical evidence of ectasia is a contraindication to LASIK.
- Presence of only one functioning eye.
- Pregnancy and lactation
- Immunocompromised states like cancer, HIV / AIDS
- Diabetics with reduced corneal sensation
- Progressive retinal conditions
- Patients with deep set eyes or large eyebrows (which lead to difficult in achieving suction with the suction ring)

LASIK should be done with caution in the following conditions:
- Mild dry eyes
- Diminished corneal sensation
- Connective tissue diseases like rheumatoid arthritis, systemic lupus erythematosus, Sjogren syndrome, Granulomatosis with Polyangiitis.
- Any corneal disease
- Patients on medication with isotretinoin, amiodarone, sumatriptan, and topical or oral corticosteroids
What are the Tests Required before LASIK?
You will have to be first evaluated by an eye doctor to consider suitability for the procedure
- If you are wearing contact lenses, you will be required to discontinue soft lenses for about 2 weeks and rigid lenses for about 2-3 weeks prior to examination by the eye doctor
- A complete ophthalmic examination will be carried out which includes testing your visual acuity, refraction, slit lamp examination, measurement of intraocular pressure and examination of your retina.
- Corneal topography (computerised analysis of corneal surface) will be done.
- You will be asked to place your chin on the chin rest of the topographer and make your forehead touch the forehead rest. You will see lighted concentric rings. The images of these on your cornea will be used to map the surface configuration of your cornea. This does not hurt and takes just a couple of minutes.
- Pachymetery (measurement of corneal thickness) - The procedure is similar to that described above for corneal topography.
How to Prepare before LASIK Surgery?
- Avoid eye makeup from 3 days prior to surgery
- You may be prescribed antibiotic eye drops from 1-3 days prior to the surgery by your doctor
- This is a day care procedure and does not require admission. You may reach the hospital on the day of your procedure.
What Happens During the LASIK Surgery in the Operation Theatre?
- The entire procedure takes about 10-15 minutes.
- An oral anti-anxiety medication may be recommended to be taken on the morning of the procedure.
- In the operation theatre, you will be made to lie down. The skin around your eyes will be cleaned with povidone – iodine or alcohol for antiseptic purposes.
- A sterile drape will be place over your face, and local anesthetic eye drops will then be instilled in your eyes to make them numb and pain free. The entire procedure after this is painless.
- An instrument will then be place in your eye to keep the eyelids separated. You might feel some pressure but there will be no pain.
- A suction device will be placed on the eye and the suction applied in order the raise the intraocular pressure to a high level. This is done to make the cornea firm so that the blade can make a good cut of the cornea. While the suction is being applied, you will experience a complete loss of vision; this is normal. Vision will return once the suction is removed.
- The blade of the microkeratome is used to make the corneal flap,.
- Alternately, in some cases the flap is created using the femtosecond laser. If the flap is created by a femtosecond laser, your bed is then moved so that you are now placed under the excimer laser machine.
- You will be required to maintain fixation on the blinking green light.
- The corneal flap is then raised to expose the stromal bed.
- While the flap is raised and the procedure is being done, the fixation light may appear distorted; this is normal. Just gaze at the center of the light.
- The laser is centered and focussed and laser energy is delivered to your eye.
- The flap is then replaced.
- Your eyes may be checked at the slit lamp to make sure the flap is properly aligned.
- A shield will be placed over the eyes, and you can go home immediately.
Recovery after LASIK Surgery
- Vision usually improves within the first day, during which time you may feel a mild gritty sensation in your eyes.
- You will be instructed to instil antibiotic eye drops and corticosteroid eye drops for about 3-7 days after the procedure. You may be asked to use more frequent or longer duration of corticosteroid eye drops if you have undergone a femtosecond LASIK.
- You will need to wear a protective shield for up to a week during sleep and while showering.
- You will be seen the next day to make sure the flap is properly aligned. After that visits are usually scheduled 1 week, 1, 3, 6 and 12 months after the procedure.
- Dryness of eyes is usually present for a few weeks to months after the procedure. Discomfort due to dryness may be addressed by the use of artificial tears.
- Reduction of low contrast visual acuity and night vision symptoms like glare and halos may occur for a couple of months following LASIK. This can cause difficulty in driving at night for some people.
What are Some Do’s and Don’ts after the Procedure?
- Avoid rubbing and squeezing of the eyes to prevent flap displacement.
- Avoid swimming and hot tubs for at least 2 weeks after the procedure.
- Avoid getting sweat and water inside the eyes for about 2 weeks.
- Exercise is best avoided for 2 weeks.
- You may bathe the next day, but water should not get into the eyes.
- Eye makeup and creams should not be used for a week.
- Artificial tears in the form of eye drops may be used for dry eyes, but ointments should be avoided in the early post-operative period to prevent migration under the flap.
Complications and Risks of LASIK Surgery
LASIK is a relatively safe surgery. However sometimes complications can occur as follows:
- Overcorrection or under-correction
- Optical aberrations
- De-centered ablations
- Dry eyes and diminished corneal sensation
- Infection of the cornea
- Scarring of cornea
- Raised intraocular pressure due to corticosteroid use
- Corneal perforation
- Flap related complications:
- Irregular or thin flaps
- Buttonholing of the flap
- Folds in the flap
- Complete loss of the flap (flap dislocation)
Diffuse Lamellar Keratitis (also called Sands of Sahara Syndrome)
- This is a non-infectious inflammation due to debris or toxins at the interface of the corneal flap. Treatment usually requires lifting the flap and irrigating out the debris.
- Growth of corneal epithelium under the flap
- Corneal ectasia (outward bulging of the cornea)












