What is Orchidectomy?
Orchidectomy/orchiectomy is a surgery performed to remove one or both testes in a male. The testes (or testicles) are the male reproductive organs that produce both sperm and the male hormone known as testosterone. The external sex organs, the penis and the scrotum (the loose sac that contains both the testes), are left intact during the operation.
Anatomy of the Testes
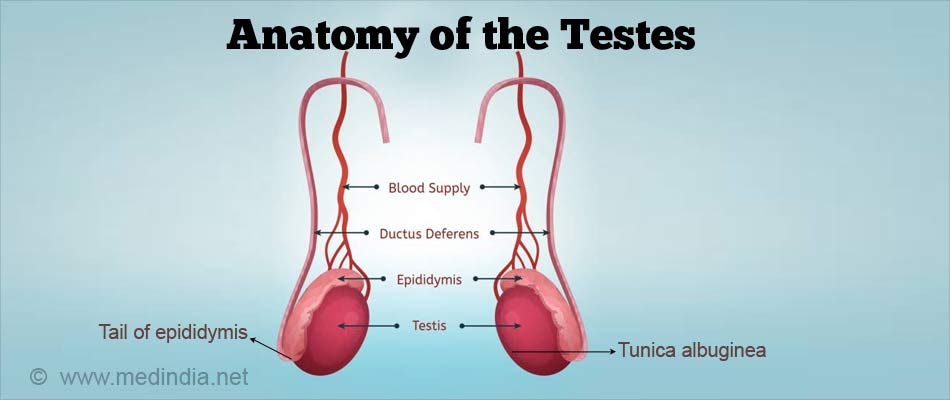
The testes (singular = testis) are a pair of ovoid organs located in the scrotum outside the abdomen since they require a lower temperature than the temperature present inside the body. Each testis is suspended by the spermatic cord and enclosed in a thick, fibrous capsule called the tunica albuginea. There is a mass of convoluted tubes behind each testis called the epididymis, where the sperms are stored and mature. A tube called the vas deferens carries the sperms from the epididymis and joins the duct coming from the seminal vesicle to form the ejaculatory duct. The ejaculatory duct passes through the prostate and opens up into the urethra.
What are the Types of Orchidectomy?
There are three types of orchidectomy:
- Simple orchidectomy
- Subcapsular orchidectomy
- Radical or inguinal orchidectomy
Simple and subcapsular orchidectomy procedures are usually done under local or regional anesthesia and completed in about 30 minutes, while radical orchidectomy procedure takes up to an hour to complete and possibly requires general anesthesia.
Why are the Indications for Orchidectomy?
Simple or subcapsular orchidectomy is performed for the following reasons:
- Cancer of the testes
- Certain cases of prostate cancer whose growth is testosterone (hormone) dependent
- Trauma or torsion of testes
- Part of sex reassignment surgery from male to female (MTF)
- Other conditions like male breast cancer and post-puberty undescended testis (to prevent cancer development)
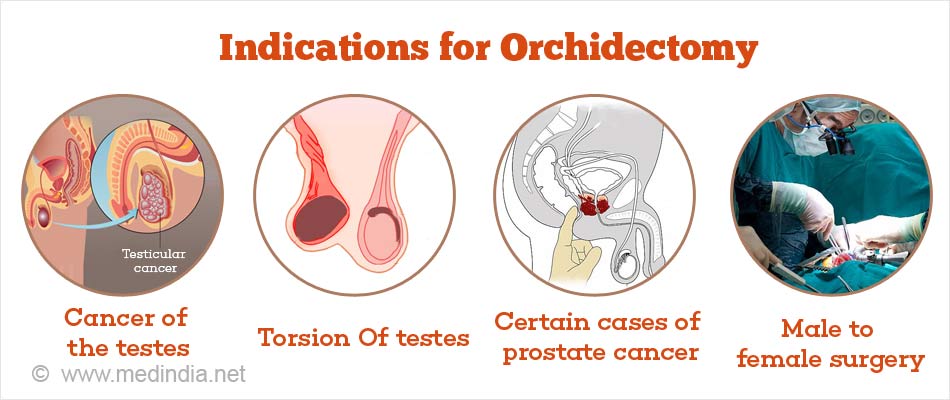
Simple orchidectomy is usually done bilaterally (removal of both testes) to halt the production of testosterone in prostate cancer and as part of sex reassignment surgery from male to female.
Subcapsular orchidectomy is a variation of simple orchidectomy and is performed to treat hormone-dependent prostate cancer. The capsule of the testes is left behind to maintain the shape of the scrotum.
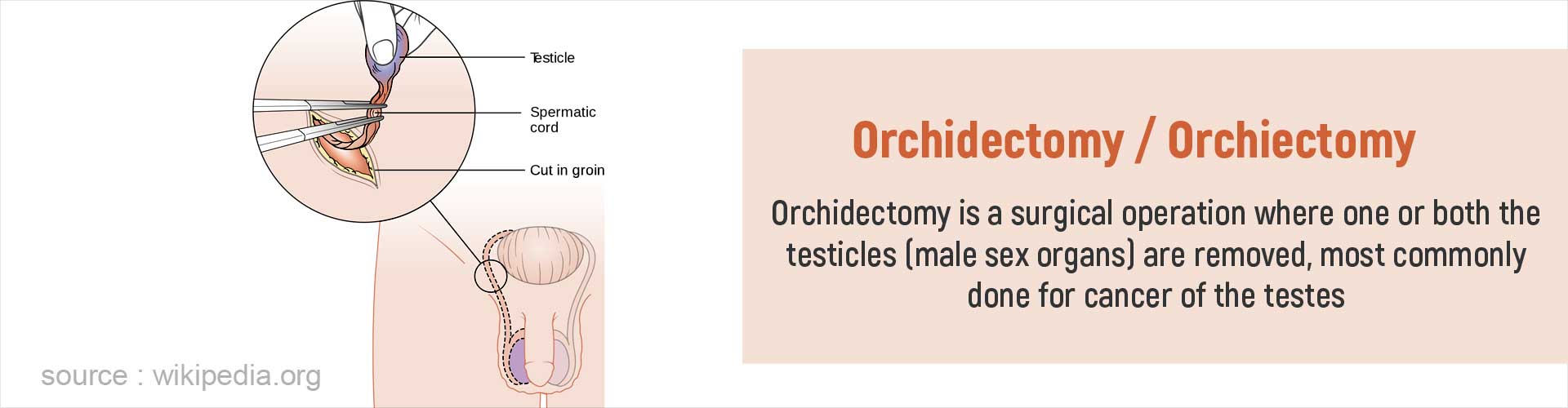
Radical orchidectomy is the removal of the testis and the spermatic cord. It is done through an incision in the groin and most commonly performed to treat suspected testicular cancer. It can be done unilaterally or bilaterally.
How do you Prepare Before Orchidectomy?
The decision for surgery is made based on a physical examination and tests to confirm the underlying condition; the next step is to plan necessary preoperative preparations. If you wish to undergo gender transformation, you will be given extensive psychiatric assistance before the procedure and will be allowed to undergo the procedure only once the doctor confirms that you need it. You will be prescribed hormones to be taken for months to years before the surgery.
Preoperative Assessment (A few days before the operation)
- You will need to undergo routine blood and urine tests as well as a chest x-ray and an electrocardiogram (ECG) to assess your general health condition.
- If you are on blood thinners such as aspirin, you may be asked to stop them for a few days before the operation to reduce bleeding during the surgery.
- You may be advised to reduce or avoid smoking for a few days before the surgery to improve healing post-operatively.
- During the visit to the preoperative assessment clinic, the anesthetist will review you to assess if you are fit enough to tolerate general anesthetic (if required).
- You will be counseled about what to expect after the surgery, especially with regards to sexual changes. Sperm banking may be advised if you wish to father a child after the surgery.
The Day before the Surgery
- You should not eat or drink anything for about 8 to 10 hours before the operation.
- You may be given specific medicines to take, such as an anxiolytic, the night before surgery to enable a good night’s rest.
Morning of the Surgery
- You will have to report to the hospital early on the morning of surgery.
- You can have a regular bath or shower as usual before coming.
- In the hospital, you will be required to sign a consent form for the surgery. You should understand the reason for surgery, the procedure involved and the possible risks of the procedure.
- The nurse will clean the groin area including the external genitalia and shave the hair overlying the skin.
- You will be given an operation theater gown to wear for the procedure.
- A few minutes before the procedure you will be wheeled into the operating room.
What Happens during the Surgery?
Shift to the Operating room - The ambience in the operating room can sometimes be very daunting. From the trolley, you will be shifted on to the operating table. As you look up, you will see the operating light console, and at the end where your head is, there will be the anesthesia machine. There may also be monitors to check oxygen levels, ECG, and other vital parameters. A constant beeping sound may be present from the monitors, which may sometimes be irritating.
Anesthesia before Surgery - If the procedure is done under general anesthesia, the anesthetist will inject drugs through an intravenous line and make you inhale some gases through a mask that will put you in a deep sleep. Once you are asleep, a tube will be inserted into your mouth and windpipe to administer the anesthetic gases to overcome pain and keep you comfortable while the surgery is going on. If the procedure is done under local anesthesia, you will receive an injection to numb the skin.
Simple orchiectomy:
- The penis will be taped to the abdomen to give clear access to the operating area.
- The surgeon will make a cut in the midpoint of the scrotal skin and cut through the deeper layers.
- When the testis is reached, the surgeon will remove the testis (usually both sides) through the opening of the incision.
- After removal of the testes, the layers of the wound are closed with sutures and a skin dressing placed over the wound.
- If the patient wishes, a prosthetic testicle may be inserted through the incision before closing the wound to retain the normal appearance of the scrotum.
Subcapsular orchiectomy:
- Another procedure commonly performed for the treatment of prostate cancer is subcapsular orchiectomy. It is similar to a simple orchiectomy; however, only the glandular tissue is removed rather than removing the entire testis. This type of operation is preferred to maintain the normal appearance of the scrotum.
Radical or Inguinal orchiectomy
This operation is usually performed for testicular cancer where the testis and the spermatic cord are removed to prevent the spread of cancer via the spermatic cord to regional lymph nodes and other organs in the abdomen. It can be performed either unilaterally or bilaterally.
- The surgeon makes a cut in the patient's groin area just above the inguinal ligament (in contrast to a scrotal incision in both simple and subcapsular orchiectomies) and dissects through the deeper layers of tissue taking care not to damage the ilioinguinal nerve.
- The testis (or both testes) along with the entire spermatic cord is removed through the incision.
- A long, non-absorbable suture may be left in the stump of the spermatic cord should a repeat surgery become necessary.
- Following the removal of the cord and testicle(s), the surgeon cleans the area with saline solution, and the incisions are closed with sutures.
- The wound is covered with a sterile gauze dressing and bandaged.
What Happens After the Orchidectomy?
- If you have received general anesthesia, once the surgery is over, you will wake up, and the tube down the wind pipe will be removed. You will be asked to open your eyes before the tube is removed. You will be sedated, and the voice of the anesthetist may be faint. Once the tube is out, you may experience a cough and possibly nausea.
- Once you are fully awake, you will be shifted to the recovery room where vital signs such as your blood pressure, temperature, pulse, and breathing will be checked regularly by the nurse.
- Your wound site will be checked for bleeding or oozing from the incision.
- You will be given painkillers for relief of pain in the operative site.
- You may be permitted to take sips of water as soon as you return from your operation, unless you feel nauseous; you will be given medicines to reduce the feeling of nausea.
- If general anesthesia has been used, you will be given intravenous fluids until you pass wind, when liquid diet will be introduced first, and gradually normal diet will be resumed. You will be encouraged to walk around early to prevent deep vein thrombosis.
- You may have scrotal support or support pants on to keep your dressing secure.
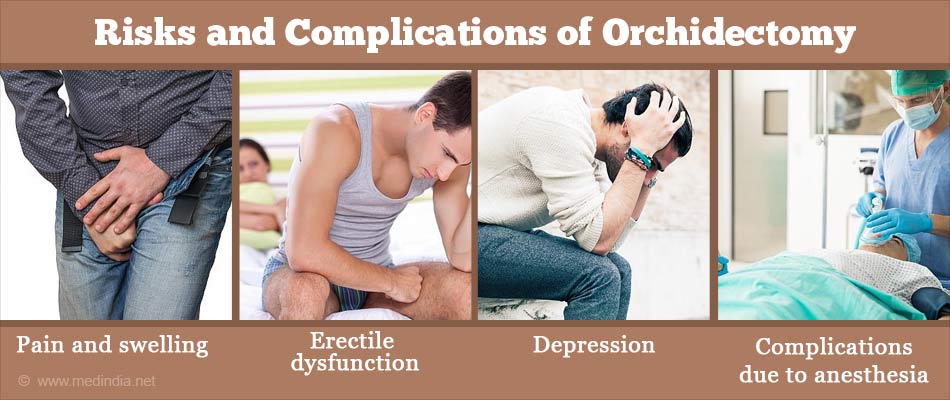
What are the Risks and Complications of Orchidectomy?
Orchidectomy is a safe procedure but can be associated with certain complications
- Pain and swelling around the wound and scrotum are quite common
- Erectile dysfunction (impotence)
- Bleeding and hematoma formation
- Infection
- Hot flashes, depression, breast enlargement, weight gain and mood swings, brittle bones (all these symptoms are due to the lack of testosterone)
- Complications due to anesthesia
Recovery After Orchidectomy
- The dressing under the scrotal support may be removed or changed 24 hours after the surgery, and you may then be allowed to shower.
- You can wear the scrotal support until you are free from pain and use painkillers and ice pack as needed.
- It is normal to have slight bruising, pain and swelling in the operative area- this will settle over the next few weeks. However, excessive swelling is not normal. Undue pain or swelling and persistent oozing or bleeding is not normal and if this happens, contact your doctor immediately.
- Usually the stitches will dissolve on their own and need not be removed. However, if you have skin staples, you will be given an appointment within a week to have them removed.
- It is normal to feel tired for a few weeks after having an operation; this will get better over a few weeks. You can return to work and perform other routine activities as you feel comfortable.
- Avoid lifting and carrying heavy loads for up to 6 weeks. Sex should be avoided until the doctor gives the green signal.
- Regular followup with your doctor will be needed as appropriate in case of testicular cancer or prostate cancer.