What is Parotidectomy?
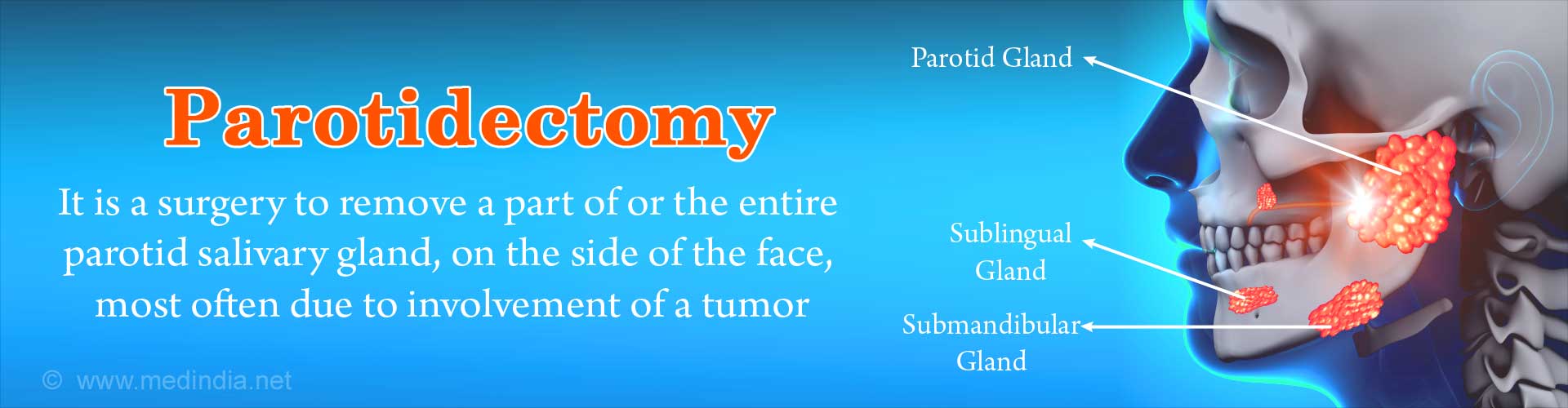
Parotidectomy is a surgical procedure done to remove a part or the entire parotid gland when there is a disease or tumor associated with it. The amount of parotid gland to be removed depends on where the lesion is located in the gland.
Parotid Glands - Overview
The parotid glands are the largest salivary glands. There are two parotid glands, one on either side of the face situated below and in front of the ears. Along with the other salivary glands, the parotid glands secrete saliva to keep the mouth moist and aid in chewing and swallowing of food.
Each parotid gland has superficial and deep parts or lobes. An important structure, the facial nerve runs in the mid-plane of the gland with the superficial part above the facial nerve and the deep part below it.
The facial nerve has important functions and is responsible for the action of muscles that cause facial expressions. It is also responsible for the secretion of saliva by the submandibular and sublingual salivary glands, and the secretion of tears by the lacrimal gland (though it passes through the parotid gland, it does not supply to the gland). Therefore it is important to ensure that the facial nerve is identified and not damaged during parotid surgery.
What are the Types of Parotidectomy?
The types of parotidectomy include the following:
- Superficial parotidectomy – Superficial parotidectomy is a surgical procedure in which the part of the gland above the facial nerve is removed. This is the most common type of surgery performed. When only the lesion in the superficial part of the gland is removed leaving behind the portion of the gland unaffected by the tumor or lesion, the procedure is referred to as partial superficial parotidectomy.
- Total parotidectomy – In this procedure, both the superficial and the deep lobes of the parotid gland are removed as they are affected by the disease. This is a less commonly performed procedure as compared to superficial parotidectomy. If the facial nerve is free from disease, it is important to carefully identify and retain all its branches while removing the gland.
- Radical parotidectomy – In this surgery, in addition to a total parotidectomy, the facial nerve is also removed. Sometimes, other structures such as the temporal bone and the skin overlying the parotid gland are also removed, in which case the surgery is referred to as extended radical parotidectomy.
What are the Indications for Parotidectomy?
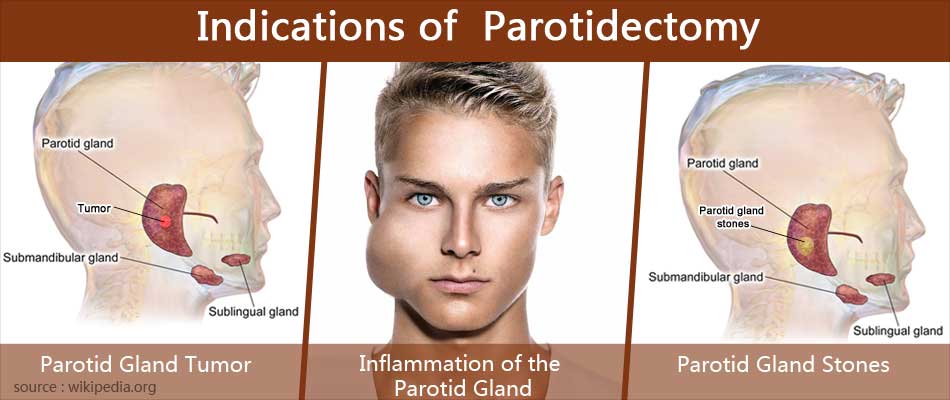
Parotidectomy may be performed for the following reasons:
- Benign or malignant tumor in the parotid gland (most common reason)
- Chronic inflammation of the parotid gland (chronic sialadenitis)
- Parotid gland stones
- Parotid gland infection and abscess formation
- Excessive salivation (sialorrhea), which may rarely require parotidectomy surgery
What are the Tests required before Parotidectomy?
During the initial visits, the doctor will conduct a clinical examination and tests to confirm the disease of the parotid gland. A CT or an MRI scan and a final needle aspiration biopsy may be done to understand the type and extent of the tumor growth.
Routine tests are also advised before the surgery that include the following:
- Blood tests to include a full blood count, liver and kidney function tests, estimation of blood glucose levels, bleeding and clotting times, tests for Hepatitis B, C and HIV, and blood group and type
- Urinalysis to check for diabetes, kidney disease, urinary infection or other diseases.
- Chest x-ray and electrocardiogram (ECG) tests to look for lung or heart diseases that may alter the type of anesthesia or choice of anesthetic agent.
After the investigations, the patient is evaluated and cleared for surgery by the cardiologist and the anesthetist.
What is the Preparation required for Parotidectomy?
Before the surgery, the following preparations have to be made to ensure a better outcome.
- Medications such as aspirin, anticoagulants or NSAIDs should be stopped at least two weeks prior to the surgery as they increase the risk of bleeding.
- You will have to get admitted to the hospital on the evening prior to the surgery to administer certain medications or for certain procedures. Nothing should be taken to eat or drink for at least 10-12 hours before the surgery.
- Medications may be administered the night before surgery to reduce secretions during anesthesia and the surgery and to allay anxiety before the surgery.
- The skin overlying the lesion is shaved to remove hair and cleaned with antiseptic solution.
What is the Procedure for the Parotidectomy procedure?
Once the surgical room is ready, you will be shifted from the waiting area to the operating room. There will be monitors to check oxygen levels, ECG and other vital parameters.
The parotidectomy surgery is performed under general anesthesia due to which you will be asleep during the procedure. During general anesthesia, the anesthetist will inject drugs through an intravenous line and make you inhale some gases through a mask that will put you in deep sleep.
A tube will then be inserted into your mouth and windpipe to administer the anesthesia gases to overcome pain and keep you comfortable during the surgery. Your vital signs like blood pressure and heart rate will be constantly monitored.
During the procedure:
- You may be connected to a monitor that will give a signal when the facial nerve or its branches are stimulated.
- The surgeon makes an incision below and in front of the ear along the natural skin crease to reduce scar visibility. An incision in the neck may be used for total parotidectomy.
- After going through the tissues overlying the parotid gland, the surgeon reaches the diseased area and removes the tumor plus or minus the facial nerve as appropriate.
- If a part of or the entire facial nerve is removed during the procedure, a nerve graft may be performed. Additionally if the temporal bone needs to be removed, a bone resection may be performed.
- A drainage tube may be placed within the gland coming out through the skin to drain any blood or fluid that may collect after the surgery.
- The layers of tissue are sutured and the skin incision is closed with surgical clips or sutures.
What Happens After Parotidectomy?
- If you have received general anesthesia during the surgery, once the surgery is over, you will wake up and the tube down the wind pipe will be removed. Once the tube is out, you may have cough and sometimes nausea. There will also be an intravenous line and may still have a nasogastric tube going into your stomach. You will remain on oxygen support.
- Once fully awake, you will be shifted on the trolley and taken to the recovery room. Your vital signs will be monitored for a few hours and if stable, you will be shifted back to your room.
- Medications will be given to relieve postoperative pain and intravenous fluids to keep you hydrated on the night of the surgery.
- By the next day, if conditions permit, you may be given a liquid diet or soft solids. You will be encouraged to move from your bed early to prevent deep vein thrombosis.
- The drainage from the surgical site is monitored and once it stops, the tube will be removed.
- Depending on the extent of surgery and duration of drainage, you may be kept in the hospital for 3-7 days.
- Once all the tubes are removed and you are independent, you will be discharged. Sometimes, you may be discharged with the drainage tube in place and a plastic bulb attached to the tube to collect the secretions.
- Oral medications will be prescribed to reduce pain.
- You will be instructed to come to the hospital on the 6th or 7th post-operative day for removal of sutures and to collect the biopsy report. Additional radiotherapy or chemotherapy may be prescribed if the growth turns out to be cancerous on the biopsy report.
- Mild pain on the face and a degree of numbness may be normal after parotid surgery, but if you are unable to smile or wink or find it difficult to make facial expressions, or have a dry mouth, these may indicate facial nerve injury and you should report to the hospital immediately.
- Followup imaging studies may be performed in 6-8 weeks in case of a cancerous tumor to check if the tumor is returning.
- Most patients improve gradually and within one year regain full function of the facial nerve.
What are the Risks and Complications of Parotidectomy?
The complications of parotidectomy include the following:
- Bleeding – If there is continued bleeding in the operated area, there may be a rapidly enlarging swelling or hematoma with severe pain. You will be immediately taken to the operating room, where the doctor will identify the bleeding blood vessel and tie it.
- Infection – Post-operative infection with fever and swelling of the operated site has to be treated with antibiotics.
- Loss of sensation – There may be loss or reduced sensation over the skin of the neck, side of the face and ear lobe. Over time, the area affected will reduce in size, but the earlobe continues to lack sensations.
- Seroma – Accumulation of fluid under the skin of the neck may occur after the drainage tube is removed. This may resolve spontaneously or may need aspiration with a needle.
- Sialocele – Sialocele is a collection of saliva under the skin of the surgical area. The swelling will get bigger with eating. Applying a pressure bandage will help or in some cases, repeated aspiration may be needed.
- Facial nerve injury – This is a feared complication of parotid surgery. In spite of the skill of the operating surgeon, a few branches of the facial nerve may be inadvertently injured or cut. If the nerve is only stretched, the symptoms may be temporary. If the nerve is cut, the damage is permanent. If this happens, you will be unable to use muscles of facial expression on the same side as the operation or blink the eye. Treatment involves performing a nerve graft and ensuring that the affected eye remains moist and lubricated at all times to prevent dryness and corneal ulceration. Facial reanimation procedures may be undertaken to enhance the appearance.
- Frey’s syndrome – Frey’s syndrome is a complication of parotid surgery characterized by sweating on the skin of the face and neck associated with eating. This occurs because the nerve endings that stimulated saliva secretion during eating are now in contact with the sweat glands under the skin (since the parotid gland is removed). While eating, the nerve endings stimulate the sweat glands and cause the sweating.
This complication can be avoided by placing a barrier of fascia or muscle between the free nerve endings and the skin.