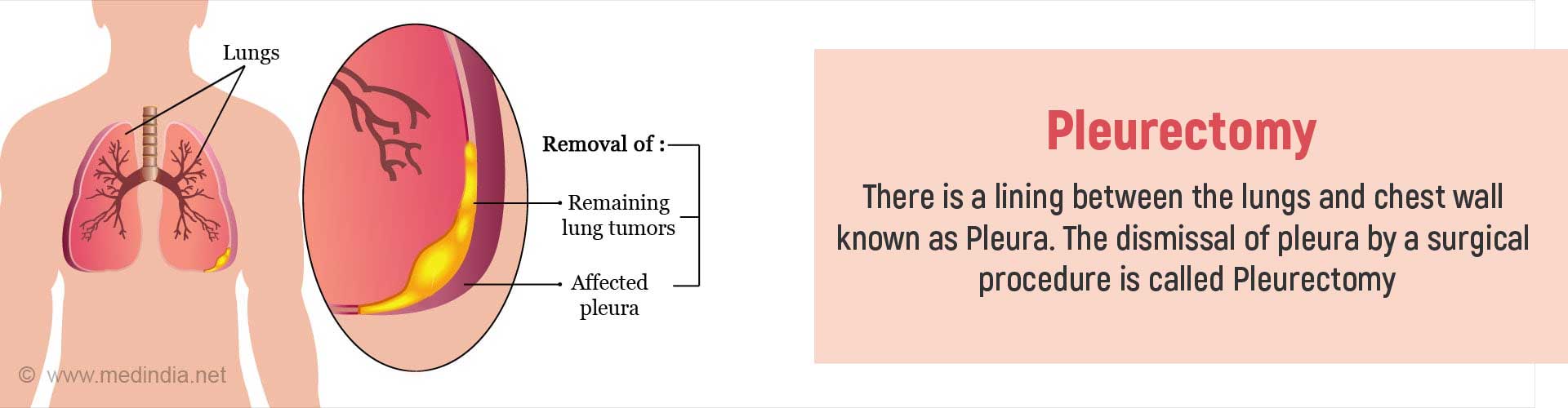
What is Pleurectomy?
The lungs has an outer lining called the pleura and this lining separates the lung from the chest wall. The removal of the diseased pleura is performed by a surgical procedure and this is called pleurectomy.
The pleura are two thin layers of tissue that protect the lungs; it is partitioned into two membranes. Visceral pleura is the inner layer that is close to the lungs and covers the surface of each lung. Whereas Parietal pleura is the outer layer that is close to the chest wall. The space between the two layers of the pleura is known as pleural cavity. There is also a small quantity of fluid present in between that protects the lungs during respiration.
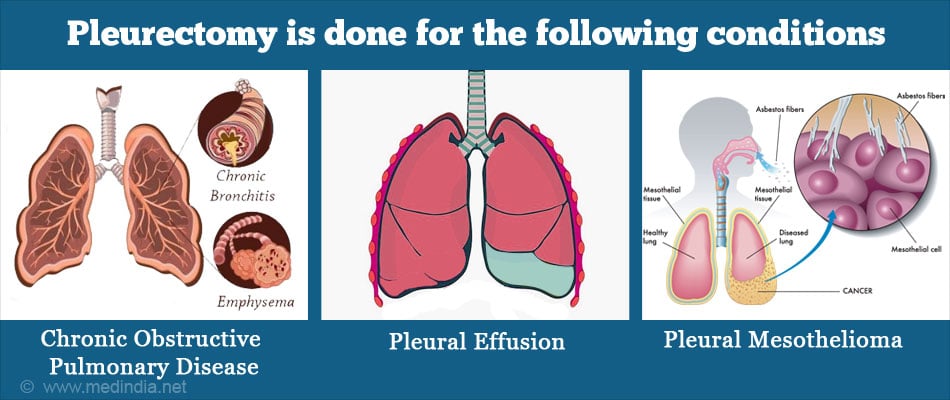
Why is it done?
Pleurectomy is done for medical conditions that damage the pleura and affects the lungs. This procedure aims to revert the affected lung to a normal breathing state. Once the pleura is removed, it tends to improve or enhances the affected patient's respiratory movement.
Who should undergo this Surgery?
Pleurectomy is for patients with the following conditions:
Pneumothorax:
Pneumothorax or a collapsed lung - Primary Spontaneous Pneumothorax occurs due to factors such as smoking, family history and Secondary Spontaneous Pneumothorax occurs due to lung diseases such as chronic obstructive pulmonary disease or COPD. Spontaneous pneumothorax, pleurectomy is done to intercept the lungs from collapsing.
Pleural Effusions:
The excess fluid deposition between the pleural space is known as pleural effusion. It leads to difficulty in breathing, which is evident in lung and breast cancer. Pleurectomy is performed to abort the fluid deposition which improves breathing.
Pleural Mesothelioma:
Due to inhalation of asbestos particles, pleura can become cancerous. Though palliative treatment is available, pleurectomy maybe done in an early case to treat mesothelioma.
What are the Types of Pleurectomy?
Video-Assisted Thoracoscopic Surgery(VATS) is a minimally invasive surgery that is now regarded by many surgeons to be the gold standard in the surgical management of spontaneous pneumothorax (SP), and other pleural diseases.
Pleurectomy in combination with Decortication(PD) is a lung-saving surgery for pleural mesothelioma where the diseased pleura of a patient’s lung along with any other tumors in the chest is removed. The lung remains intact.
Thoracotomy is an incision into the pleural space of the chest performed to gain access to the thoracic organs.
Total Parietal Pleurectomy is a complete resection of the parietal pleura to treat patients with recurrent pneumothorax. Total parietal pleurectomy can also be performed by a thoracoscopic procedure know as Thoracoscopic parietal pleurectomy to treat primary spontaneous pneumothorax.
Pulmonary Wedge Resection in combination with parietal Pleurectomy (WRPP) is a two step surgery process to remove a part of the lung tumor and a complete resection of the parietal pleura. It is to treat patients with recurrent primary spontaneous pneumothorax.
How do you Prepare before Pleurectomy?
During your first appointment after prior admission check-up, a surgeon will explain details about the admission date, and the procedure details. If you are taking any medications, please inform about them to the doctor during this screening process. A nurse will access your health condition to check if you are fit for surgery. It will include some mandatory tests before undergoing pleurectomy.
What are the Tests Required before Pleurectomy?
The following tests are done in a combination depending upon each patient's complications.
Chest Radiography (X-Ray)
Chest X-ray is the primary test to confirm a lung disease such as mesothelioma to know if you have to undergo pleurectomy. It helps to identify any infection, tumor, and any abnormality in the lungs.
CT Scan
For a CT scan, you will be asked to lie down still on a table for a few minutes. A doughnut-shaped instrument will pass over the part to be screened, and images will be taken. A contrast may be injected into your vein; therefore you should inform the radiologist if you suffer from any allergies.
MRI
For an MRI, you will be placed inside a narrow tube, which can sometimes make you claustrophobic if you have a fear of enclosed spaces. Few centers do offer more open MRI machines, but the drawback is that the pictures may not be as clear. The MRI machine makes loud clicking noises, and it is advisable to ask for earplugs to help block these sounds out.
Routine Tests
Every patient who undergoes an elective surgery (which is more planned) needs to have some regular checks done that include the following:
- Blood tests like hemoglobin levels, and blood group
- Liver and kidney function tests
- Urine tests
- Pulmonary Function Tests (PFT)
- ECG to study the electrical activity of the heart
- In older patients, a detailed assessment of the heart may be required.
How is Pleurectomy Performed?
Type of Anesthesia: Pleurectomy is practiced under general anesthesia. You will be asleep during the procedure and will not be aware of what is going on.

Pre-operative Checkup: Routine tests as indicated above are ordered a few days before the surgery. Admission is required a day or two before the surgery. You will be asked to stop taking aspirin or any other blood thinners before the procedure.
Fasting before surgery: Partial fasting is necessary for this operation. You should maintain a nutritious fluid diet for 48 hours before surgery. Intravenous fluid may be needed to keep you well hydrated. At times, sedation is given for good overnight sleep before the surgery.
The shift from ward or room to the waiting area in the operating room:
You will be asked to get admitted to the hospital one day before your surgery appointment. An hour or two before the surgery, you will be shifted to the operating room's waiting area on a trolley. Once the surgical room is ready, you will be moved to the operating room.
Shift to the Operating room: The ambiance in the operating room can sometimes be very daunting, and a small amount of sedation can help overcome your anxiety. From the trolley, you will be shifted on to the operating table. As you look up, you will see the operating light console at the head, and at the end will be the anesthesia machine. There may also be monitors to check oxygen levels, ECG, and other vital parameters. A constant beeping sound may be present from the monitors, which may sometimes be irritating.
Anesthesia before surgery: The anesthetist will inject drugs through an intravenous line and make you inhale some gases through a mask that will put you in a deep sleep. Once you are in a deep sleep, a tube will be inserted into your mouth and windpipe to administer the anesthetic gases to overcome pain and keep you comfortable.
What Happens during the Surgery?
Pleurectomy: You are placed in a lateral position with an endotracheal tube inside your mouth. Posterolateral thoracotomy incision is made, and the parietal pleura is dissected. Later, the visceral pleura is abolished by opening the parietal pleura. Prior to suturing the incision, a drainage tube is placed to drain discharge and bleeding Once, the surgery is complete, you will be asked to start walking slowly. This will help to heal and expand your lungs.The recovery period is one to two months.
VATS pleurectomy: During VATS pleurectomy you will be lying down in a lateral position. Three 2 cm cuts will be made between the ribs. A camera and surgical instruments will be inserted in a triangular position to remove the pleura with mesothelioma. Later, the small incisions will be sutured. Since it is a minimally invasive procedure, the benefits include lesser chances of infection and faster recovery.
What Happens after Pleurectomy?
Waking up from Anesthesia: Once the surgery is over you will wake up, and they will remove the tube down the windpipe. You will be sedated, and the voice of the anesthetist may be faint. Once the tube is out, you may have a cough and sometimes nausea.
The intravenous line will remain. You will also remain on oxygen. Once fully awake, you will be shifted on the trolley and taken to the recovery room.
Recovery after Pleurectomy
Recovery: Post surgery, you will move to a recovery room inside the theater. A nurse will monitor your vitals and observe you for an hour or two before moving you to the ward.
Post-Operative Recovery: Once you return to the ward you may be kept in the hospital for up to 1 week. Change of dressing will be required. A nurse will monitor your breathing, pulse, and BP.
Follow-ups: You will have to visit the hospital for follow-ups as recommended by your doctor. You will be prescribed antihistamines and analgesics to control pain discomfort. Respiratory therapy will also be given until full recovery.
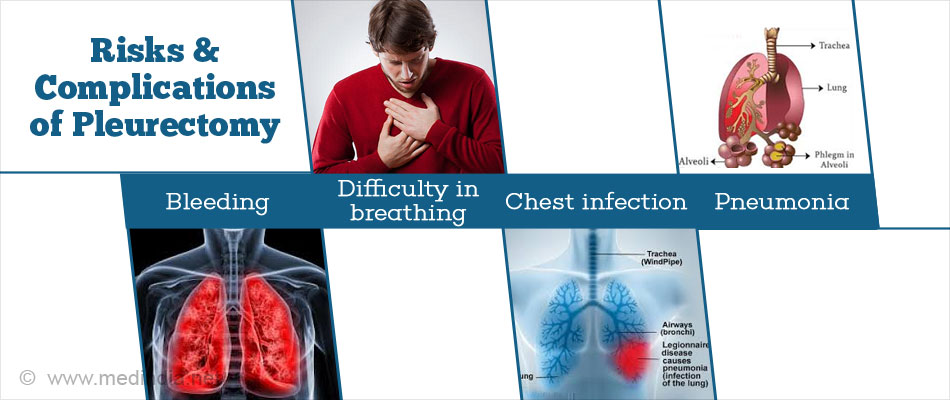
What are the Risks and Complications of Pleurectomy?
Any procedure may contain a minimum risk or complication. Possible risks/complications of pleurectomy include the following:
- Difficulty in breathing
- Pneumonia
- Bleeding
- Chest infection
- Lungs and chest wall damage
- Air Leak: makes the chest tube challenging to remove post surgery
- Post operative pain