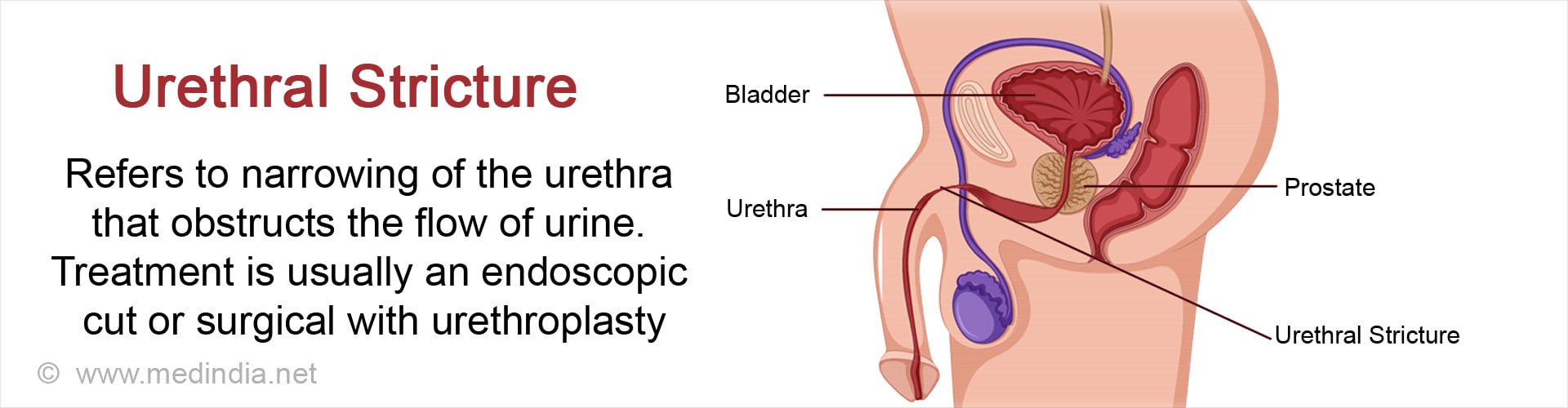
What is a Urethral Stricture?
Urethral stricture refers to narrowing of the urethra due to formation of scar tissue. It obstructs the free flow of urine through the urethra.
Anatomy of the Urethra
The urethra is the conduit for urine from the urinary bladder into the exterior. The male urethra is longer, around 17 to 20 cm in length. Besides urine, it also carries semen. It can be divided into two parts:
The posterior urethra which consists of:
- The prostatic urethra, which passes through the prostate
- The membranous urethra, which is surrounded by the external urethral sphincter and the perineal membrane
The anterior urethra which consists of:
- The bulbous urethra, which is the upper part at the root of the penis
- The penile urethra, which passes through the penis and opens out into the exterior through the external meatus. Its lower dilated end is called the fossa navicularis
The urethra in females is smaller (about 4 to 5cms long or about 2 inches) and is less susceptible to injuries and strictures.
Depending on their location, urethral strictures are classified as:
- Anterior urethral strictures, which are more common
- Posterior urethral strictures, which are often associated with pelvic fractures
Most strictures occur in the bulbar urethra, and next commonly in the penile urethra. Strictures may occur in both the parts together as well or they may extend the whole length of the anterior urethra.
What are the Causes of Urethral Stricture?
A urethral stricture consists of scar tissue that narrows the lumen of the urethra. Causes of urethral stricture include:
- Infection like gonococcalurethritis- Since these infections are less common nowadays, urethral strictures due to these infections are also rare
- Inflammatory conditions like lichen sclerosus affecting the penile skin
- Trauma to the urethra, which may occur due to:
- Direct injury to the urethra resulting in rupture of the urethra

- A fracture of the pelvic bones
- Use of instruments through the urethra like cystoscope, urinary catheter or urethral dilators for various procedures
- After surgical procedures like radical prostatectomy and transurethral resection of prostate
- Radiation to the pelvic region, which is often administered to patients with prostate cancer
In some cases, the cause of urethral stricture cannot be determined.
What are the Symptoms and Signs of Urethral Stricture?
Symptoms and signs of urethral stricture include the following:
- Difficulty and hesitancy while passing urine
- A poor urinary stream
- The need to strain while passing urine
- Prolonged dribbling of urine in the end due to incomplete emptying of the urinary bladder
- Increased frequency of urination during the day as well as at night especially if there is associated urinary infection
- Enlarged bladder that may be noticed in the lower abdomen
These symptoms are similar to those experienced by patients with prostate enlargement. However, patients with urethral stricture are usually younger than those affected by prostate enlargement.
What are the Complications of Urethral Stricture?
Most of the complications of urethral stricture arise due to incomplete emptying of the urinary bladder. These include the following:
- Acute retention of urine especially after drinking alcohol or following postponement of micturition
- Stone formation in the urinary bladder
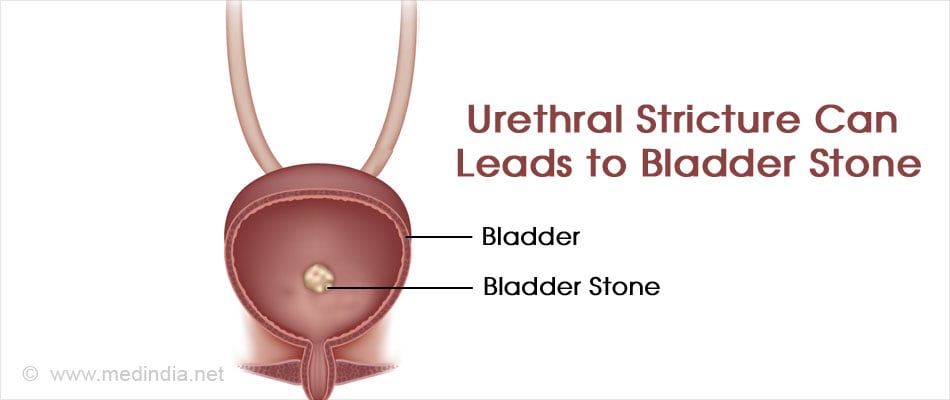
- Hydronephrosis or swelling of the kidney
- Thickening of bladder wall
- Repeated urinary tract infections
- Abscesses around the urethra
- Infection of the prostate or testis
- Sepsis
- Kidney failure in long standing stricture and obstruction
How is Urethral Stricture Diagnosed?
Urethral stricture is diagnosed based on the medical history and examination of the patient, and certain tests. The patient may give a history of suffering from a previous gonorrheal infection, or prior injury or surgical procedure on the urethra. The stricture may be obvious on examining the penis. The following tests are required in a patient with suspected urethral stricture:
- Urine test: A urine test is done to diagnose the presence of a urinary tract infection.
- A uroflow study is done to note the extent of obstruction.
- Ascending Urethrography: Urethrography is the study of the passage of a contrast medium through the urethra, which helps to identify the stricture, its location and its extent. In retrograde urethrography, the contrast is introduced through a catheter into the urethra, and images are taken while it passes through the urethra, which help to identify the stricture and its length.
In antegrade urethrography, the contrast is introduced into the urinary bladder through a suprapubic catheter, a catheter directly introduced into the urinary bladder, or through the urethra, and images are taken while the patient passes urine

- Urethroscopy / Cystoscopy: Cystoscopy is a procedure where an endoscope is introduced through the urethra into the urinary bladder to examine the inner surface of the urethra and urinary bladder.
- Ultrasound: Ultrasound can be used to evaluate the stricture especially before surgery and to check the post-void volume of urine retained within the bladder. High post void urine makes it prone to infection.
How is Urethral Stricture Treated?
Emergency Treatment - If the patient suffers from acute retention of urine due to urethral strictures, an emergency suprapubic catheterization is required.
Endoscopic Stricture –
- Direct visualization internal urethrotomy (DVIU): This procedure is done with the help on an endoscope. The scar tissue is incised so that the width of the lumen is increased. Recurrence of stricture is commonly noted with the procedure.
- Urethral dilatation: Dilatation of the urethra can be done with the help of catheters, balloons or other methods. The results are similar to that of DVIU. They should be done over a guide wire and not blindly for a stricture.
Endoscopic surgery can be done under local anesthesia as a day or overnight stay in the hospital. However long term results may not be the best. They are reserved for short segment strictures and re-strictures after open urethroplasty.
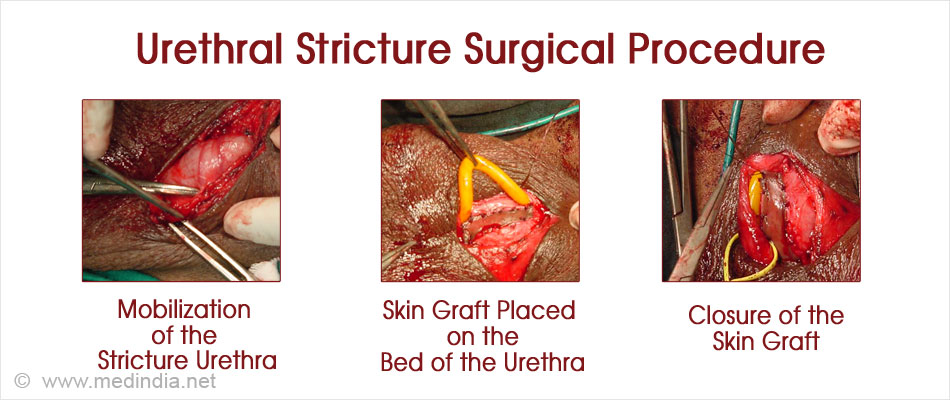
Open Urethroplasty Surgery
The open surgical procedure used to treat urethral strictures is called urethroplasty. Open surgery involves longer stay and needs to be done under regional or general anesthesia. The surgery itself can take 3 to 4 hours to perform. It is the preferred treatment for recurrent and failed endoscopic strictures. Its long term chances of success is better and has low chances of recurrence. Type of open surgery depends on length and type of stricture.
The types of urethroplasty include:
- Excision and end-to-end urethroplasty. This procedure is performed on small strictures in the bulbar urethra of less than 2 cm in length. The stricture is excised and the cut ends are spatulated and re-attached. Possible complications of the procedure include problems with erection or ejaculation, a glans with less sensation, a smaller penis and chordee (where the head of the penis bends downwards or upwards)
- Substitution graft urethroplasty: In this procedure, the stricture is incised but not removed, and an external graft is placed to widen the lumen. The graft is obtained from the inner surface of the cheek (buccal mucosa) or the undersurface of the tongue. The graft is placed either ventrally or dorsally or both, depending on the type and extent of the stricture. The procedure avoids some of the complications of end-to-end urethroplasty. Difficult or recurrent cases may require a two-staged and more complex procedures.
Pre-operative Care
Pre-operative Check-up - Routine tests as indicated above are ordered a few days before the surgery. Admission is required a day before the surgery.
Fasting before surgery - Overnight fasting is required and occasionally intravenous fluid maybe required to keep you well hydrated. Sedation is sometimes required for good overnight sleep before the surgery.
Shift from the ward or room to the waiting area in the operating room - An hour or two before the surgery, you will be shifted to the operating room waiting area on a trolley.
Once the surgical room is ready, you will be shifted to the operating room.
Type of Anesthesia -
Urethroplasty is done under regional or general anesthesia.
You will be usually asleep during the procedure and will not be aware of what is going on.
Shift to the Operating room - The ambience in the operating room can sometimes be daunting and a small amount of sedation can help overcome your anxiety.
From the trolley, you will be shifted on to the operating table. As you look up, you will see the operating light console and at the head end will be the anesthesia machine. There may also be monitors to check oxygen levels, ECG and other vital parameters. A constant beeping sound may be present from the monitors, which may sometimes be irritating.
Anesthesia before surgery - The anesthetist will inject drugs through an intravenous line and make you inhale some gases through a mask that will put you in deep sleep for anesthesia. Once you are in deep sleep, a tube will be inserted into your mouth and windpipe to administer the anesthesia gases to overcome pain and keep you comfortable.
Waking up from Anesthesia - Once the surgery is over you will wake up and the tube down the wind pipe will be removed. You will be asked to open your eyes before the tube is removed. You will be sedated and the voice of the anesthetist may be faint. Once the tube is out, you may have cough and sometimes nausea.
There will be an intravenous line. You will remain on oxygen. Once fully awake, you will be shifted on the trolley and taken to the recovery room.
Regional Anesthesia - It can be a spinal or epidural anesthesia. The spinal anesthesia involves injection of the anesthetic agent adjacent to the spinal cord or just outside it using a long needle. This renders the portion of the body beyond or below (as the case maybe) the point of injection numb and anesthetized, while the rest of the body remains unanesthetised.
The injection is usually administered in the lumbar (low back) spine. This form of anesthesia is easy to be administered and is ideally suited for surgeries performed in the lower parts of the body.
For this anaesthesia the patient is usually positioned in a sitting posture on the operating table. The forearms can be made to rest on the thighs to make the patient stable and comfortable. Alternatively, the procedure can be performed with the patient lying on their side with their hips and knees maximally flexed.
Following positioning, the anesthetist will clean the back region using anti-septic solution. He may administer a little bit of local anesthetic to numb the skin at the point where he is going to give the spinal, so that no pain is felt due to the spinal needle. The local anesthetic solution is then injected into the spinal space through a long needle. (Usually between L3 - L4, it is subject to change and vary from individual to individual). After successful administration, the patient is positioned in the required position and once again all your parameters will be checked by the anesthetist.
Recovery room - In the recovery room, a nurse will monitor your vitals and observe you for an hour or two before shifting you to the room or a ward.
Post-operative Care
- Drains that are left in are removed after 24 to 48 hours.
- Mobilisation starts after 2 to 3 days
- Intravenous fluids maybe discontinued after 2 days once the patient starts taking oral fluids
- A urinary catheter that is left in the bladder after the surgery is removed after 2 to 3 weeks
- A uroflow study is done once the catheter is removed to note the extent of improvement
- Hospital stay is usually a week to 10 days.
- A contrast study is sometimes undertaken before or after catheter removal
- Follow up visits are usually planned at 3 months, 6 months and then every year for at least 5 years.
- A uroflow study is done during the follow up.