Dr.Sunil Shroff, Dr. S.Venkat Ramanan
Urethral Pressure Profile (UPP)
For measuring UPP a triple lumen catheter is required. This needs to be positioned accurately before the start of the procedure. It measures the passive resistance of a particular point within the urethra. Many factors contribute to this resistance, including the elastic properties of the tissues surrounding the lumen and the tension generated by the smooth and skeletal muscles of the urethra, which are constantly changing during the micturition cycle It is difficult to extrapolate data obtained when the bladder is empty and apply it to periods when the bladder is full, is responding to increases in abdominal pressure, or is in the process of emptying . Failure to recognize this fact leads to false assumptions and improper treatment. In view of this many centres use leak point pressure (LPP) (pressure at which leak occurs) instead of UPP
Video Urodynamics
Video urodynamics has gained popularity since its introduction in 1970. Visualization of the bladder and bladder neck during filling and of the urethra during voiding has added a dimension for more accurately integrating all aspects of lower urinary tract function and characterizing an abnormality. Incompetence of the bladder neck or pelvic floor or the location of any posterior urethral obstruction can be correlated with pressure measurements recorded simultaneously. Sometimes, aberrations noted on pressure monitoring of sphincter EMG tracings can be confirmed, enhancing these findings.
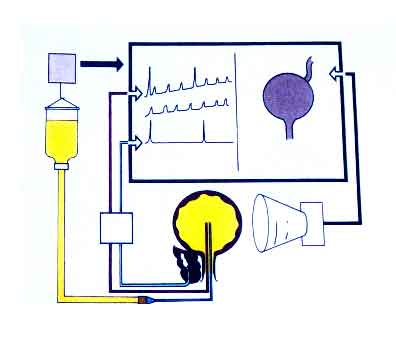
Ambulatory urodynamics
This technique measures natural fill cystometry with the help of an ambulatory urodynamic monitor linked to a notebook computer. It has become available and feasible in children with the development of micro transducers mounted on small catheters positioned in the bladder. Data can be stored up to 24 hours at a time and analyzed later. When combined with techniques to monitor wetness, it can be a very effective way to determine the cause of incontinence. Intravesical pressures are measured via 5F suprapubic catheters inserted 24 hrs earlier. Factors assessed include: activity during fill, voiding pressures and flow, uroflow, PdMax, PVR, emptying efficiency (voided volume/capacity).
Urodynamics in Dysfunctional Voiding
The clinical features of bladder hyperactivity—urgency, frequency, and precipitate voiding—occur in about 60% to 70% of affected patients. These symptoms characterize the commonly occurring urgency-incontinence syndrome in children whose bladder instability elicits a weak or absent sphincteric response. Incontinence may vary in severity. Urodynamic study is not required in most cases for diagnosis; it may be safely reserved for children who fail an empiric trial of anticholinergic drug therapy. When performed, it confirms bladder instability with minimal evidence of dyssynergia or obstruction. Consequently, UTI is not a major feature of this subcategory. Ultrasonography of the urinary tract is characteristically normal except for bladder wall thickening, and VCUG, if performed to evaluate for UTI, typically demonstrates a smooth-walled bladder with capacity nearly appropriate for age. Children with bladder instability void normally to completion without residue, so the occurrence of a large residual urine volume should make the diagnosis suspect. One sign that is almost pathognomonic is Vincent's curtsey, so named because the child squats with the heel of one foot compressing the perineum and urethra to prevent urinary leakage.
The small-capacity, hypertonic bladder subcategory is characterized clinically by more prominent symptoms and urodynamically by more obvious bladder-sphincter dyssynergia causing functional obstruction. UTIs commonly occur and are associated with prominent urgency and incontinence that characteristically persist after eradication of the infection. Typically, functional bladder capacity is observed to be reduced during urodynamic study or cystography. This appears to be the result of chronic repetitive functional obstruction during unstable contractions, which is reflected in radiographic studies that may show bladder wall thickening, saccules, and diverticula. Very severe spectrum of this disorder represents Hinman’s Syndrome, the non neurogenic neurogenic bladder.
Urodynamics in Neurogenic Bladder
A combination of bladder contractility and external sphincter activity results in three categories of lower urinary tract dynamics: synergic (19%), dyssynergic with and without detrusor hyper tonicity (45%), and complete denervation (36%). In the past these bladders are classified in to contractile, mixed and acontractile bladders. DSD occurs when the external sphincter fails to decrease or actually increases its activity during a detrusor contraction or a sustained increase in intravesical pressure as the bladder is filled to capacity. Frequently, a poorly compliant bladder with a high intravesical pressure occurs in conjunction with a dyssynergic sphincter, resulting in a bladder that empties only at high intravesical pressures Complete denervation is noted when no bioelectric potentials are detectable in the region of the external sphincter at any time during the micturition cycle or in response to sacral stimulation or a Credé manoeuvre.
The categorization of lower urinary tract function in this way has been extremely useful because it reveals which children are at risk for urinary tract changes, which ones should be treated prophylactically, which need close surveillance, and which can be monitored at greater intervals. Aggressive observation and prompt intervention is essential to prevent upper tract deterioration in these children. A typical child for bladder augmentation is the one with small capacity non compliant bladder with deteriorating renal function and worsening hydronephrosis.
Urodynamics in Posterior urethral valves (PUV)
For many years, it has been recognized that most children treated for urethral valves have varying degrees of abnormal bladder function. Most often, this abnormality presents as urinary incontinence, with half of the boys still damp during the day well into late childhood. In the past, investigators assumed that this incontinence was primarily a result of incompetent sphincter function. However, with the application of modern urodynamics to paediatric urology, it has become increasingly obvious that primary vesical dysfunction is commonly present in association with urethral valves, that this vesical dysfunction does not necessarily abate after relief of the obstruction, and that, ultimately, this abnormal bladder function has a significant impact on prognosis.
Three different types of vesical dysfunction has been categorised with the help of urodynamics. These include: bladder instability; non compliant bladder; and myogenic failure. Progressing from instability during infancy to findings more consistent with myogenic failure in older boys has been seen during observations. Regular monitoring with base line urodynamics starting from the age of four is becoming the norm these days.
Urodynamics in Vesico ureteric reflux VUR
Studies of urodynamics are indicated for any child with a suspected secondary cause for reflux (e.g., valves, neurogenic bladder, non-neurogenic neurogenic bladder, voiding dysfunction). This is becoming even more important with the realization that a significant number of patients with reflux have bladder instability, inadequate urethral relaxation during voiding, and voiding dysfunction. Complete evaluations include cystometrography, flow studies with electromyography, and video recordings. Valid urodynamic values can be difficult to obtain in the face of massive reflux. When this is the case, ureteral occlusion catheters can be placed to eliminate the dampening effect of deleterious pressures that reflux offers the bladder.
Conclusion
Urodynamics in children require several adaptations in view of the small bladder size and patient size. As stressed earlier, it should not be take lightly and should be supervised by the physician in charge of the patient. Because of the invasive nature and inherent sepsis risk, urodynamics should be recommended only after non invasive tests like uroflowmetry have been exhausted. Interpretation of urodynamics in children should be done cautiously as it can have a lot of fallacies and artefacts. EMG, rectal catheters and video are important tools in children to minimize artefacts. Identifying the high risk bladder, the small capacity non compliant bladder with high leak point pressure is of paramount importance. Prompt medical or surgical intervention with clean intermittent catheterisation (CIC) will save these children from renal failure in the long term.
Subscribe to our Free Newsletters!